Abstract
Background
The impact of preoperative body composition as independent predictor of prognosis for esophageal cancer patients after esophagectomy is still unclear. The aim of the study was to explore such a relationship.
Methods
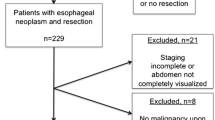
This is a multicenter retrospective study from a prospectively maintained database. We enrolled consecutive patients who underwent Ivor-Lewis esophagectomy in four Italian high-volume centers from May 2014. Body composition parameters including total abdominal muscle area (TAMA), visceral fat area (VFA), and subcutaneous fat area (SFA) were determined based on CT images. Perioperative variables were systematically collected.
Results
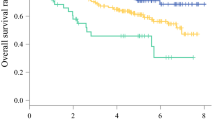
After exclusions, 223 patients were enrolled and 24.2% had anastomotic leak (AL). Sixty-eight percent of patients were sarcopenic and were found to be more vulnerable in terms of postoperative 90-day mortality (p = 0.028). VFA/TAMA and VFA/SFA ratios demonstrated a linear correlation with the Clavien-Dindo classification (R = 0.311 and 0.239, respectively); patients with anastomotic leak (AL) had significantly higher VFA/TAMA (3.56 ± 1.86 vs. 2.75 ± 1.83, p = 0.003) and VFA/SFA (1.18 ± 0.68 vs. 0.87 ± 0.54, p = 0.002) ratios. No significant correlation was found between preoperative BMI and subsequent AL development (p = 0.159). Charlson comorbidity index correlated significantly with AL (p = 0.008): these patients had a significantly higher index (≥ 5).
Conclusion
Analytical morphometric assessment represents a useful non-invasive tool for preoperative risk stratification. The concurrent association of sarcopenia and visceral obesity seems to be the best predictor of AL, far better than simple BMI evaluation, and potentially modifiable if targeted with prehabilitation programs.




Similar content being viewed by others
References
J. M. Leers et al., “The CARDIA-trial protocol: a multinational, prospective, randomized, clinical trial comparing transthoracic esophagectomy with transhiatal extended gastrectomy in adenocarcinoma of the gastroesophageal junction (GEJ) type II,” BMC Cancer, vol. 20, no. 1, p. 781, Aug. 2020.
D. E. Low et al., “Guidelines for Perioperative Care in Esophagectomy: Enhanced Recovery After Surgery (ERAS®) Society Recommendations,” World J. Surg., vol. 43, no. 2, pp. 299–330, 2019.
T. Lerut, W. Coosemans, G. Decker, P. De Leyn, P. Nafteux, and D. Van Raemdonck, “Anastomotic complications after esophagectomy,” Dig. Surg., vol. 19, no. 2, pp. 92–98, 2002.
N. Yoshida et al., “An original scoring system for predicting postoperative morbidity after esophagectomy for esophageal cancer,” Surg. Today, vol. 45, no. 3, pp. 346–354, 2015.
U. Fumagalli et al., “Incidence and treatment of mediastinal leakage after esophagectomy: Insights from the multicenter study on mediastinal leaks,” World J. Gastroenterol., vol. 25, no. 3, pp. 356–366, 2019.
D. E. Low et al., “Benchmarking Complications Associated with Esophagectomy,” Ann. Surg., vol. 269, no. 2, 2019.
L. Schaheen, S. H. Blackmon, and K. S. Nason, “Optimal approach to the management of intrathoracic esophageal leak following esophagectomy: A systematic review,” Am. J. Surg., vol. 208, no. 4, pp. 536–543, 2014.
P. Parise, U. Elmore, U. Fumagalli, G. De Manzoni, S. Giacopuzzi, and R. Rosati, “Esophageal surgery in Italy. Criteria to identify the hospital units and the tertiary referral centers entitled to perform it,” Updates Surg., vol. 68, no. 2, pp. 129–133, 2016.
E. R. C. Hagens, M. C. J. Anderegg, M. I. van Berge Henegouwen, and S. S. Gisbertz, “International Survey on the Management of Anastomotic Leakage After Esophageal Resection,” Ann. Thorac. Surg., vol. 106, no. 6, pp. 1702–1708, Dec. 2018.
A. Turkyilmaz, A. Eroglu, Y. Aydin, C. Tekinbas, M. Muharrem Erol, and N. Karaoglanoglu, “The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma,” Dis. Esophagus, vol. 22, no. 2, pp. 119–126, Apr. 2009.
S. S. Shachar, G. R. Williams, H. B. Muss, and T. F. Nishijima, “Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review,” Eur. J. Cancer, vol. 57, pp. 58–67, Apr. 2016.
V. Baracos and S. M. R. Kazemi-Bajestani, “Clinical outcomes related to muscle mass in humans with cancer and catabolic illnesses,” Int. J. Biochem. Cell Biol., vol. 45, no. 10, pp. 2302–2308, 2013.
J. C. Brown and J. A. Meyerhardt, “Obesity and Energy Balance in GI Cancer,” J. Clin. Oncol., vol. 34, no. 35, pp. 4217–4224, Dec. 2016.
C. Palmela et al., “Body Composition as a Prognostic Factor of Neoadjuvant Chemotherapy Toxicity and Outcome in Patients with Locally Advanced Gastric Cancer,” J. Gastric Cancer, vol. 17, no. 1, pp. 74–87, Mar. 2017.
A. J. Cruz-Jentoft et al., “Sarcopenia: Revised European consensus on definition and diagnosis,” Age Ageing, vol. 48, no. 1, pp. 16–31, 2019.
P. R. Boshier et al., “Long-term variation in skeletal muscle and adiposity in patients undergoing esophagectomy,” Dis. Esophagus, pp. 1–7, 2021.
N. Pecorelli et al., “Effect of sarcopenia and visceral obesity on mortality and pancreatic fistula following pancreatic cancer surgery,” Br. J. Surg., vol. 103, no. 4, pp. 434–442, 2016.
P. Parise et al., “Application of ERAS protocol in esophagectomy: a national survey among Italian centers performing esophageal surgery,” Updates Surg., vol. 73, no. 1, pp. 297–303, 2021.
C. M. M. Prado et al., “Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study,” Lancet Oncol., vol. 9, no. 7, pp. 629–635, Jul. 2008.
N. Mitsiopoulos, R. N. Baumgartner, S. B. Heymsfield, W. Lyons, D. Gallagher, and R. Ross, “Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography,” J. Appl. Physiol., vol. 85, no. 1, pp. 115–122, Jul. 1998.
M. Ferland et al., “Assessment of adipose tissue distribution by computed axial tomography in obese women: association with body density and anthropometric measurements,” Br. J. Nutr., vol. 61, no. 2, pp. 139–148, 1989.
I. Lewis, “The surgical treatment of carcinoma of the oesophagus* with special reference to a new operation for growths of the middle third,” Br. J. Surg., vol. 34, no. 133, pp. 18–31, Jul. 1946.
A. Pennathur, O. Awais, and J. D. Luketich, “Technique of Minimally Invasive Ivor Lewis Esophagectomy,” Ann. Thorac. Surg., vol. 89, no. 6, pp. S2159–S2162, Jun. 2010.
J. Veziant et al., “Imaging of postoperative complications following Ivor-Lewis esophagectomy,” Diagn. Interv. Imaging, 2021.
C. Mariette et al., “Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer,” N. Engl. J. Med., vol. 380, no. 2, pp. 152–162, 2019.
I. Nozaki et al., “Impact of laparoscopy on the prevention of pulmonary complications after thoracoscopic esophagectomy using data from JCOG0502: a prospective multicenter study,” Surg. Endosc., vol. 32, no. 2, pp. 651–659, 2018.
D. Dindo, N. Demartines, and P. A. Clavien, “Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey,” Ann. Surg., vol. 240, no. 2, pp. 205–213, 2004.
D. E. Low et al., “International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG),” Ann. Surg., vol. 262, no. 2, pp. 286–294, 2015.
J. A. Elliott, S. L. Doyle, C. F. Murphy, E. M. Guinan, P. Beddy, N. Ravi and J. V. Reynolds, “Sarcopenia: Prevalence, and Impact on Operative and Oncologic Outcomes in the Multimodal Management of Locally Advanced Esophageal Cancer”, Ann Surg 2017; 266:822–830
P. yu Wang et al., “Sarcopenia and Short-Term Outcomes After Esophagectomy: A Meta-analysis,” Ann. Surg. Oncol., vol. 27, no. 8, pp. 3041–3051, 2020.
P. R. Boshier, R. Heneghan, S. R. Markar, V. E. Baracos, and D. E. Low, “Assessment of body composition and sarcopenia in patients with esophageal cancer: a systematic review and meta-analysis,” Dis. Esophagus, vol. 31, no. 8, Aug. 2018.
Tomo Ishida, Tomoki Makino, Makoto Yamasaki et al. “Quantity and Quality of Skeletal Muscle as an Important Predictor of Clinical Outcomes in Patients with Esophageal Cancer Undergoing Esophagectomy after Neoadjuvant Chemotherapy” Ann Surg Oncol (2021) 28:7185–7195. https://doi.org/10.1245/s10434-021-10025-x.
K. Kataoka et al., “Prognostic Impact of Postoperative Morbidity After Esophagectomy for Esophageal Cancer: Exploratory Analysis of JCOG9907.,” Ann. Surg., vol. 265, no. 6, pp. 1152–1157, Jun. 2017.
X. Zhang, H. Li, M. He, J. Wang, Y. Wu, and Y. Li, “Immune system and sarcopenia: Presented relationship and future perspective,” Exp. Gerontol., vol. 164, p. 111823, 2022.
Z. Liang et al., “Inflammaging: The ground for sarcopenia?,” Exp. Gerontol., vol. 168, p. 111931, 2022.
G. E. A. U.-M.-G. Jimenez-Gutierrez Laura E.AU - Martínez-Armenta, CarlosAU - Pineda, CarlosAU - Martínez-Nava, Gabriela A.AU - Lopez-Reyes, AlbertoTI - Molecular Mechanisms of Inflammation in Sarcopenia: Diagnosis and Therapeutic Update, “No Title,” Cells, vol. 11, no. 15. 2022.
M. G. Farb and N. Gokce, “Visceral adiposopathy: a vascular perspective,” vol. 21, no. 2, pp. 125–136, 2015.
U. Fehrenbach et al., “Ct body composition of sarcopenia and sarcopenic obesity: Predictors of postoperative complications and survival in patients with locally advanced esophageal adenocarcinoma,” Cancers (Basel)., vol. 13, no. 12, 2021.
J. KONDRUP, H. H. RASMUSSEN, O. L. E. HAMBERG and Z. STANGA, “Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials,” Clin. Nutr., vol. 22, no. 3, pp. 321–336, Jun. 2003.
K. Valkenet, J. C. Trappenburg, R. Gosselink et al. “Preoperative inspiratory muscle training to prevent postoperative pulmonary complications in patients undergoing esophageal resection (PREPARE study): study protocol for a randomized controlled trial”, Trials, 2014; 15:144.
L. K. Chen, L. K. Liu, J. Woo, et al. “Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia”, J Am Med Dir Assoc. 2014; 15:95–101. https://doi.org/10.1016/j.jamda.2013.11. 025.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cossu, A., Palumbo, D., Battaglia, S. et al. Sarcopenia and Patient’s Body Composition: New Morphometric Tools to Predict Clinical Outcome After Ivor Lewis Esophagectomy: a Multicenter Study. J Gastrointest Surg 27, 1047–1054 (2023). https://doi.org/10.1007/s11605-023-05611-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05611-1