Abstract
Purpose
The aim of the present study was to compare two clinical pathways: the multiple-access outpatient pathway versus the telemedicine pathway.
Methods
The multiple-access outpatient pathway and the telemedicine pathway were both performed with WatchPAT and implemented in a real-life healthcare scenario, adopting a cost-minimization approach. A cost-minimization analysis was undertaken to assess the economic impact of the two alternatives. The cost analyses were performed in euros for the year 2021 adopting the patient, the hospital, and the societal perspectives. Given the chosen perspectives, direct medical costs, direct nonmedical costs, and indirect costs were considered. In addition, a univariate sensitivity analysis was conducted.
Results
From a hospital perspective, the telemedicine approach was estimated to cost €49 more than the multiple-access alternative. Considering the patient perspective, the telemedicine approach was estimated to cost €167 less than the multiple-access pathway. Considering the societal perspective, the telemedicine approach is estimated to cost €119 less than the multiple-access pathway.
Conclusion
The adoption of telemedicine home sleep apnea testing could improve the efficiency of the healthcare processes if considering the direct and indirect costs incurred by patients and not only by healthcare providers.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is a sleep disorder characterized by intermittent complete and partial airway collapse, resulting in frequent episodes of apnea and hypopnea. The breathing pauses cause acute adverse effects, including oxyhemoglobin desaturation, fluctuations in blood pressure and heart rate, increased sympathetic activity, cortical arousal, and sleep fragmentation [1]. The OSA prevalence reported by population-based epidemiological studies from the USA, China, Spain, India, Korea, Japan, and Sweden published between 1993 and 2013 was a mean of 22% (range, 9–37%) in men and 17% (range, 4–50%) in women. The prevalence in different studies, ranging from 2003 to 2021 and set in countries such as the USA, Belgium, and Italy, has increased with time and OSA in the last studies was reported in 37% of men and in 50% of women [2, 3]. The differences over time could be due to different equipment and definitions for the apnea-hypopnea scoring [2].
OSA has been strongly associated with metabolic diseases, including obesity [4]. As the number of obese people continues to rise, OSA is becoming increasingly prevalent [5]. Despite its high prevalence in the general population, significant undiagnosed disease burden remains. Simple, widely available, and cost-effective diagnostic capabilities are needed [6].
Polysomnography (PSG), the “gold standard” diagnostic procedure for diagnosing OSA, is scarce, complex, costly, and resource-intensive. The high cost of attended in-lab PSG (e.g., equipment, maintenance costs, staff costs, and hospitalization) can be a limiting factor and as such has received increasing attention in literature [7,8,9]. The advent of home sleep apnea testing (HSAT) introduced a simple technical solution for the diagnosis of OSA, with greater accessibility, lower cost, and reasonable accuracy in subjects without other sleep or medical comorbidities. HSAT avoids the need for patients to face long waiting lists for an attended in-hospital PSG [10,11,12]. Further advantages include the ability to record data in a natural sleep environment and reduced costs. The OSA diagnosis could be provided to wide sectors of the population using home-based techniques[13]. In recent years, testing for OSA outside of the hospital has become increasingly common in the USA as well as in the rest of the world. Development of simplified portable monitoring devices (PMD), to perform home sleep testing, began in the 1980s and continues today [12]. The preferred terminology is home sleep apnea testing (HSAT), which denotes that the devices utilized for this purpose should be used to diagnose OSA [7].
Currently, patients with suspected OSA can choose between two different pathways (i.e., multiple-access outpatient pathway and telemedicine pathway) for sleep apnea testing. No comparisons between the multiple-access pathway and the telemedicine alternative have been undertaken.
However, there is published evidence of economic evaluations comparing in-lab sleep apnea testing with HSAT pathway, aiming to estimate the costs and the cost-effectiveness of each alternative. Studies have shown that the home-based pathway is a cost-effective and cost-saving strategy compared with the laboratory-based one.
Therefore, the aim of the present study was to compare two clinical pathways: the multiple-access outpatient pathway versus the telemedicine pathway, both performed with WatchPAT and implemented in a real-life healthcare scenario.
Methods
The WatchPAT device has been utilized in both the multiple-access and telemedicine pathways. It is a HSAT device that utilizes a signal generated from vascular tone in a finger (usually the first digit). The WatchPAT (peripheral arterial tonometry) or WP technology is based on peripheral arterial tone signal’s amplitude and rate, oxygen saturation, and actigraphy. The WP provides accurate sleep/wake and REM/NREM discrimination together with non-REM categorization into deep and light sleep. In addition, the WP provides accurate measurements of snoring and body position [14]. The device is attached to the patient’s wrist, like a watch [15]. The WatchPAT is a wrist-worn ambulatory device that is used to diagnose or screen for OSA and is categorized as a type 3 monitoring device by the American Academy of Sleep Medicine (AASM) [16].
The first approach, known as multiple-access HSAT, is based on multiple-accesses: first the patient undergoes the diagnostic visit and then goes back to the hospital to get the machine. The patient then performs the test at home, return the device for redelivery, and then comes back to pick up the medical reports.
The second pathway, named telemedicine HSAT, is characterized by digital health technologies in the context of sleep recording and medical reports delivery: the patient receives the testing device directly at home [17].
At the end of both the pathways, a follow-up consultation is performed. It consists of an interview during which the medical staff communicate the test results to the patient and re-assess the patient’s clinical conditions, in light of the test’s results, in order to formulate the correct diagnosis and to define further actions to be undertaken. The difference between the pathways lies in the way the service is delivered. Particularly, in the telemedicine pathway, the follow-up visit is delivered to the patients through information and communication technology.
Table 1 summarizes the two different approaches: the multiple-access pathway versus the telemedicine pathway.
A cost-minimization analysis was undertaken to assess the economic impact of two alternative home-based sleep apnea testing pathways, the “multiple-access” versus “telemedicine” approach, in the diagnosis of OSA.
Setting and data sources
The analysis was conducted from January 2021 to May 2021 and took place in Campus Bio-Medico University located in the south of Rome in Central Italy.
Data on required personnel, the relative hourly wage and working hours, equipment costs, and outpatient structure costs were collected from the 2020 accounting files. Data on the fuel costs and public transport cost as well as the mean distance to the hospital were obtained from the selected sources [18, 19]. The individuals’ working hours and median wage were acquired from the Istituto Nazionale Previdenza Sociale (INPS) [20] and Istituto Nazionale di Statistica (ISTAT) [21], respectively.
Effect assumption
The scientific literature has not reported any significant differences in terms of health outcomes between the two alternatives, thus highlighting a condition of equal effectiveness in the diagnosis of OSA adopting the two approaches [16, 22, 23].
Cost estimation
The cost analyses were performed in euros for the year 2021 adopting the patient, the hospital, and the societal perspectives [24]. The micro-costing method was used to estimate the costs associated with the two pathways. Given the chosen perspectives, direct medical costs, direct nonmedical costs, and indirect costs were considered.
From the patient perspective, direct medical costs included the outpatient visit out-of-pocket cost and the potential cost for negative studies requiring additional diagnostic investigation. The cost for potential negative studies was computed weighing the cost for in-lab diagnostic procedures [25] by the percentage of negative HSAT studies, retrieved from the scientific literature [26,27,28,29,30]. Direct nonmedical costs were mainly related to travel expenses. It was assumed that patients traveled to the hospital using their own private vehicles. The travel cost was estimated considering the mean distance of individuals to the hospital and the mean cost of fuel (i.e., petrol, diesel, and liquefied petroleum gas). Indirect costs referred to the individual temporary loss of productivity and includes the time spent by patients out of work on medical leave. The productivity loss was computed taking into account the individuals’ number of working hours lost due to medical appointments, the median hourly wage, and the daily number of working hours.
From the hospital perspective, direct medical costs included consumables costs, staff costs, equipment costs, and facility costs. Personnel costs were computed quantifying the actual work time of the staff involved (i.e., one physician for the telemedicine pathway and one physician and one health assistant for the multiple-access approach). Equipment costs were calculated on the basis of the manufacturer’s list price (including maintenance costs and taxes). Facility costs were evaluated considering the administrative costs, maintenance costs, cleaning, water, and electricity utilities. Facility costs comprised also the potential cost for negative studies.
Given the nature of this perspective, direct nonmedical costs and indirect costs were not included in the analysis.
From the societal perspective, being the broadest among the others, all the above-described costs (i.e., direct medical, direct nonmedical, and indirect costs) were included [31, 32].
Sensitivity analysis
Sensitivity analysis was used to explore and to illustrate the impact of parameters uncertainty on study findings [33].
A one-way deterministic sensitivity analysis, from the societal perspective, appraised the effect of varying various parameters one at a time while the remaining values were held at their baseline value.
Both outpatient visit and fuel costs were varied by ±50% while equipment costs were varied by ±25%. Individual hourly salaries were also varied by ±50%. The percentage of negative HSAT studies was varied between the values reported in the literature (i.e., 13% and 20%).
Results
Table 2 details the costs, from each considered perspective, comparing the telemedicine alternative with the multiple-access one.
From a hospital perspective, the telemedicine approach was estimated to cost €49 more than the multiple-access alternative. Equipment cost was the most important item accounting for 63% for the telemedicine alternative and 42% for the multiple-access pathway.
Considering the patient perspective, the telemedicine approach was estimated to cost €167 less than the multiple-access pathway. Travel expenses and temporary productivity loss were four times higher using the multiple-access approach with respect to the telemedicine alternative.
Taking into account the societal perspective, in the base-case analysis, the telemedicine approach was estimated to cost €119 less than the multiple-access pathway.
Both travel costs and costs associated with temporary productivity loss were notably larger for the multiple-access pathway. By contrast, direct medical costs were remarkably higher for the telemedicine alternative than for the multiple-access approach, equaling 44% of the total cost.
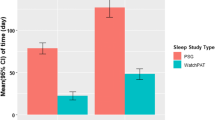
From the societal perspective, univariate deterministic sensitivity analyses were run by varying the equipment cost by 25%, fuel cost by 50%, outpatient visit by 50%, and the individual salary per hour by 50%. Figure 1 depicts the results of the univariate deterministic sensitivity analyses. The base-case cost saving was most sensitive to changes in individual hourly salary, fuel cost, and outpatient visit while it was less sensitive to changes in equipment costs.
Based on the findings, individual hourly salary had the largest impact on the base-case cost saving, increasing the cost difference between the two alternatives up to €187.
In addition, reducing the cost of the outpatient visit by 50% raised the cost savings to €148 while an increase of 50% lead to a smaller cost savings of €88.
A similar result was obtained decreasing the cost of fuel by 50% with a consequent cost savings of €73 while an increment of 50% produced a cost savings of €165.
Changes in equipment were similar to the base-case scenario and savings ranged from €134 to €102 as well as changes in the percentage of negative HSAT studies characterized by savings equal to the base-case estimate.
Discussion
The study results pointed out that, considering only the hospital perspective, the telemedicine approach was more costly than the multiple-access pathway. However, also assessing the patient and the broader societal perspective, the telemedicine alternative was likely to be a cost-saving approach.
Findings from the cost-minimization analysis were explored and confirmed by one-way deterministic sensitivity analyses highlighting that the telemedicine approach was a cost-minimizing pathway in all the assessed scenarios.
From a public health point of view, one can assume that, given the high epidemiological prevalence of OSA [2], the implementation of telemedicine approach should be promoted to allow the large share of patients who would benefit from this less costly and more easily accessible diagnostic tool.
The combination of study findings provides support for another implication. Since from a merely hospital perspective it is not cost-efficient to adopt the clinic pathway for the OSA diagnosis, decision-makers should adopt, from a perspective of public health, health policies to promote the adoption of this clinical pathway on behalf of the individual and population health. At the current time only 4% [7] of individuals are diagnosed with OSA.
Furthermore, the described comparison is of fundamental importance, not only from an economic point of view, but especially in light of the ongoing pandemic. The COVID-19 pandemic fuels the need for implementation of telemedicine in clinical practice mainly to prevent unnecessary traveling and face-to-face consultations of patients with a consequent reduction in exposure time, a decrease in infection risk, and in the provision of clinical capacities for COVID-19 patients [34,35,36]. In particular, the decrease in infection risk is achieved both by limiting the number of time patients access the hospital and by the use of disposable devices, with a much higher degree of safety with respect to devices in need of disinfection.
The findings of the present research must be considered in light of the study’s weaknesses and strengths. First of all, the advantages of home-based sleep apnea testing in the OSA diagnostic pathway are still debated [13, 37,38,39,40]. However, the HSAT method is widely adopted in the scientific literature [41].
The temporary productivity loss was not stratified by age classes. Travel costs were not stratified by individuals’ distance to the hospital. Notwithstanding, the estimation of the temporary productivity loss was based on a robust methodology and assuming that patients were in working age [42,43,44], while the calculation of travel costs was based on mean distance. An additional limitation of this study was that the share of patients with comorbidities, requiring an in-lab approach, was not taken into account.
Further studies investigating differences in terms of health outcomes, besides assessing costs, between the two alternatives are required. Additional research is required to provide robust Health Technology Assessment reports, based on the EUnetHTA Core Model [45], investigating all the relative domains.
Conclusions
Study results showed from a patient and societal perspective that the telemedicine HSAT is a cost-minimizing approach, highlighting that the adoption of this diagnostic tool may improve the efficiency of healthcare processes if considering the direct and indirect costs incurred by patients and not only by healthcare providers.
However, further medico-economic evaluations of these technologies are needed in order to validate these findings before wide dissemination of the process can be implemented.
References
McNicholas W, Krieger J (2002) Public health and medicolegal implications of sleep apnoea. Eur Respir J 20:1594–1609. https://doi.org/10.1183/09031936.02.00404502
Franklin KA, Lindberg E (2015) Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis 7:1311–1322. https://doi.org/10.3978/j.issn.2072-1439.2015.06.11
Nakayama-Ashida Y, Takegami M, Chin K et al (2008) Sleep-disordered breathing in the usual lifestyle setting as detected with home monitoring in a population of working men in Japan. Sleep 31:419–425. https://doi.org/10.1093/sleep/31.3.419
Li M, Li X, Lu Y (2018) Obstructive sleep apnea syndrome and metabolic diseases. Endocrinology 159:2670–2675. https://doi.org/10.1210/en.2018-00248
Peppard PE, Young T, Barnet JH et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. https://doi.org/10.1093/aje/kws342
Ioachimescu OC, Dholakia SA, Venkateshiah SB et al (2020) Improving the performance of peripheral arterial tonometry-based testing for the diagnosis of obstructive sleep apnea. J Investig Med 68:1370–1378. https://doi.org/10.1136/jim-2020-001448
CERGAS SDA Bocconi & Philips (2020) Cost-of-illness study of obstructive sleep apnea syndrome (OSAS) in Italy. https://www.sdabocconi.it/it/news/19/7/la-prima-analisi-dellimpatto-socio-economico-delle-apnee-ostruttive-del-sonno-osas-in-italia. Accessed 20 May 2021
Geessinck FAJ, Pleijhuis RG, Mentink RJ et al (2018) Cost-effectiveness analysis of the DiagnOSAS Screening Tool compared with polysomnography diagnosis in Dutch primary care. J Clin Sleep Med 14:1005–1015. https://doi.org/10.5664/jcsm.7170
Toraldo DM, Passali D, Sanna A et al (2017) Cost-effectiveness strategies in OSAS management: a short review. Acta Otorhinolaryngol Ital 37:447–453. https://doi.org/10.14639/0392-100X-1520
Bruyneel M (2019) Telemedicine in the diagnosis and treatment of sleep apnoea. Eur Respir Rev 28:180093. https://doi.org/10.1183/16000617.0093-2018
Flemons WW, Douglas NJ, Kuna ST et al (2004) Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med 169:668–672. https://doi.org/10.1164/rccm.200308-1124PP
Campbell AJ, Neill AM (2011) Home set-up polysomnography in the assessment of suspected obstructive sleep apnea. J Sleep Res 20:207–213. https://doi.org/10.1111/j.1365-2869.2010.00854.x
Coma-del-Corral MJ, Alonso-Álvarez ML, Allende M et al (2013) Reliability of telemedicine in the diagnosis and treatment of sleep apnea syndrome. Telemed e-Health 19:7–12. https://doi.org/10.1089/tmj.2012.0007
Tauman R, Berall M, Berry R et al (2020) Watch-PAT is useful in the diagnosis of sleep apnea in patients with atrial fibrillation. Nat Sci Sleep 12:1115–1121. https://doi.org/10.2147/NSS.S278752
Bar A, Pillar G, Dvir I et al (2003) Evaluation of a portable device based on peripheral arterial tone for unattended home sleep studies. Chest 123:695–703. https://doi.org/10.1378/chest.123.3.695
Kinoshita T, Yahaba M, Terada J et al (2018) Impact of arterial stiffness on WatchPAT variables in patients with obstructive sleep apnea. J Clin Sleep Med 14:319–325. https://doi.org/10.5664/jcsm.6970
Università Campus Bio-Medico di Roma (2021) Home-based Polysomnography. https://www.policlinicocampusbiomedico.it/units/geriatric-care/home-based-polysomnography. Accessed 16 May 2021
Ministero della Transizione Ecologica (2021) Prezzi medi settimanali dei carburanti e combustibili. https://dgsaie.mise.gov.it/prezzi_carburanti_settimanali.php. Accessed 12 May 2021
Azienda Sanitaria Locale Roma 2 PARM 2020. Piano Annuale di Risk Management ASL Roma 2. Roma
Istituto Nazionale della Previdenza Sociale (2021) Orario di Lavoro
Istituto Nazionale di Statistica (2019) Differenziali Retributivi in Italia. Roma
Jen R, Orr JE, Li Y et al (2020) Accuracy of WatchPAT for the diagnosis of obstructive sleep apnea in patients with chronic obstructive pulmonary disease. COPD J Chronic Obstr Pulm Dis 17:34–39. https://doi.org/10.1080/15412555.2019.1707789
Camilon PR, Nguyen SA, Camilon MP, Gillespie MB (2014) WatchPAT versus polysomnography: a meta-analysis. Otolaryngol Neck Surg 151:P265–P265. https://doi.org/10.1177/0194599814541629a405
Garrison LP, Pauly MV, Willke RJ, Neumann PJ (2018) An overview of value, perspective, and decision context—a health economics approach: an ISPOR Special Task Force report [2]. Value Heal 21:124–130. https://doi.org/10.1016/j.jval.2017.12.006
Regione Lazio (2013) Approvazione Nomenclatore Tariffario Regionale per Prestazioni di Assistenza Specialistica Ambulatoriale.D.M. 18.10.2012
Rosenberg R, Hirshkowitz M, Rapoport DM, Kryger M (2019) The role of home sleep testing for evaluation of patients with excessive daytime sleepiness: focus on obstructive sleep apnea and narcolepsy. Sleep Med 56:80–89. https://doi.org/10.1016/j.sleep.2019.01.014
Kapoor M, Greenough G (2015) Home sleep tests for obstructive sleep apnea (OSA). J Am Board Fam Med 28:504–509. https://doi.org/10.3122/jabfm.2015.04.140266
Punjabi NM, Aurora RN, Patil SP (2013) Home sleep testing for obstructive sleep apnea. Chest 143:291–294. https://doi.org/10.1378/chest.12-2699
Qaseem A, Dallas P, Owens DK et al (2014) Diagnosis of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med 161:210. https://doi.org/10.7326/M12-3187
Zeidler MR, Santiago V, Dzierzewski JM et al (2015) Predictors of obstructive sleep apnea on polysomnography after a technically inadequate or normal home sleep test. J Clin Sleep Med 11:1313–1318. https://doi.org/10.5664/jcsm.5194
Gold M, Siegel J, Russel L, et al (1997) Cost-effectiveness in health and medicine. John Wiley and Sons Ltd
Byford S, Raftery J (1998) Economics notes: perspectives in economic evaluation. BMJ 316:1529–1530. https://doi.org/10.1136/bmj.316.7143.1529
Andronis L, Barton P, Bryan S (2009) Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making. Health Technol Assess (Rockv) 13. https://doi.org/10.3310/hta13290
Schöbel C, Werther S, Teschler H, Taube C (2020) Telemedicine in respiratory sleep medicine: COVID-19 pandemic unmasks the need for a process-oriented, replicable approach for implementation in clinical routine. J Thorac Dis 12:S261–S263. https://doi.org/10.21037/jtd-cus-2020-011
The Health Foundation (2020) Non-COVID-19 NHS care during the pandemic. Activity trends for key NHS services in England
Pan American Health Organization (2021) COVID-19 AND TELEMEDICINE. https://www3.paho.org/ish/index.php/en/telemedicine. Accessed 27 May 2021
Mykytyn IJ, Sajkov D, Neill AM, Mc Evoy RD (1999) Portable computerized polysomnography in attended and unattended settings. Chest 115:114–122. https://doi.org/10.1378/chest.115.1.114
Portier F, Portmann A, Czernichow P et al (2000) Evaluation of home versus laboratory polysomnography in the diagnosis of sleep apnea syndrome. Am J Respir Crit Care Med 162:814–818. https://doi.org/10.1164/ajrccm.162.3.9908002
Redline S, Sanders MH, Lind BK et al (1998) Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep 21:759–767
Whitney CW, Gottlieb DJ, Redline S et al (1998) Reliability of scoring respiratory disturbance indices and sleep staging. Sleep 21:749–757. https://doi.org/10.1093/sleep/21.7.749
Yalamanchali S, Farajian V, Hamilton C et al (2013) Diagnosis of obstructive sleep apnea by peripheral arterial tonometry. JAMA Otolaryngol Neck Surg 139:1343. https://doi.org/10.1001/jamaoto.2013.5338
Stendardo M, Schito M, Casillo V, et al (2017) Obstructive sleep apnea syndrome and work ability. In: Occupational and Environmental Health. European Respiratory Society, p PA1239
Benjafield AV, Ayas NT, Eastwood PR et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698. https://doi.org/10.1016/S2213-2600(19)30198-5
Lyons MM, Bhatt NY, Pack AI, Magalang UJ (2020) Global burden of sleep-disordered breathing and its implications. Respirology 25:690–702. https://doi.org/10.1111/resp.13838
European Network For Health Technology Assessment (2016) HTA Core Model Version 3.0
Acknowledgements
Jonathan George Hart and Michele Urbano from Hospital Management, Campus Bio-Medico University, Rome, Italy, performed data extraction and analysis for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: Manuele Casale and Gianfranco Damiani; methodology: Mario Cesare Nurchis and Marcello Di Pumpo; validation: Manuele Casale, Lorenzo Sommella, and Gianfranco Damiani; formal analysis: Mario Cesare Nurchis, Marcello Di Pumpo, Antonio Moffa, and Lorenzo Sabatino; investigation: Mario Cesare Nurchis, Marcello Di Pumpo, and Antonio Moffa; resources: Mario Cesare Nurchis, Marcello Di Pumpo, Antonio Moffa, and Lorenzo Sabatino; data curation: Mario Cesare Nurchis, Marcello Di Pumpo, Antonio Moffa, and Lorenzo Sabatino; writing—original draft preparation: Mario Cesare Nurchis, Marcello Di Pumpo, Antonio Moffa, Lorenzo Sabatino, and Lucrezia Giorgi; writing—review and editing: Mario Cesare Nurchis, Marcello Di Pumpo, Antonio Moffa, Lorenzo Sabatino, Peter Baptista, Manuele Casale, Lorenzo Sommella, and Gianfranco Damiani; visualization: Mario Cesare Nurchis, Marcello Di Pumpo, Antonio Moffa, Lorenzo Sabatino, Peter Baptista, Manuele Casale, Lorenzo Sommella, and Gianfranco Damiani; supervision: Manuele Casale, Peter Baptista, Lorenzo Sommella, and Gianfranco Damiani; funding acquisition: none. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
This type of study does not require informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Pumpo, M., Nurchis, M.C., Moffa, A. et al. Multiple-access versus telemedicine home-based sleep apnea testing for obstructive sleep apnea (OSA) diagnosis: a cost-minimization study. Sleep Breath 26, 1641–1647 (2022). https://doi.org/10.1007/s11325-021-02527-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02527-5