Abstract
Introduction and objectives
Urodynamic studies are often performed in the evaluation of post-prostatectomy urinary incontinence (PPUI). The male transobturator sling (TOS) is a minimally invasive treatment for PPUI. Others have reported their results with a specific Valsalva leak point pressure (VLPP) that predicts a good outcome with the male TOS. Our objective was to determine the relationship of the pre-operative VLPP on the success rate of the male TOS in a high-volume, single center. We hypothesized that a higher pre-operative VLPP better predicts successful outcomes.
Methods
We reviewed patients undergoing a male TOS placement from 2006 to 2012 at our institution. Patients who underwent TOS placement were identified using our patient data portal (DEDUCE). Demographic, urodynamic, and follow-up data were extracted by chart review. Post-operative success was defined by the use of 0 or 1 security pad, a negative stress test on exam, or pad weight of less than 8 g per 24 h. Cox and linear regression models were performed.
Results
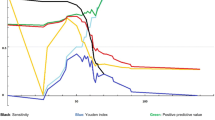
290 patients were included. All patients underwent a radical prostatectomy for prostate cancer and presented with PPUI. Mean age at surgery was 66.3 (± 7.4) years and 84% were Caucasian. Median time to follow-up was 5 months (IQR 1–15). A linear regression model shows an inverse prediction curve for sling failure versus VLPP (p = 0.02). The hazard ratio for failure with a VLPP of ≤ 70 cm H2O compared with a VLPP of > 70 cm H2O, adjusted for pelvic radiation and 24-h pad weight was 0.5 (95% CI 0.2–0.98).
Conclusion
Patient selection is imperative in the success of the male TOS for patients with PPUI. In our cohort of patients with PPUI, those with a pre-procedural VLPP of > 70 cm H2O were 50% less likely to fail after TOS placement versus those with a VLPP ≤ 70 cm H2O. In our practice, we use these data to support the use of VLPP cut off of 70 cm H2O as an indicator for success to help in the evaluation and counseling of patients.

Similar content being viewed by others
Abbreviations
- TOS:
-
Transobturator sling
- VLPP:
-
Valsalva leak point pressure
- PPUI:
-
Post-prostatectomy urinary incontinence
- IQR:
-
Interquartile range
References
Tubaro A, Carter S, Hind A, Vicentini C, Miano L (2001) A prospective study of the safety and efficacy of suprapubic transvesical prostatectomy in patients with benign prostatic hyperplasia. J Urol 166(1):172–176. https://doi.org/10.1016/S0022-5347(05)66102-2
Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG (1995) A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med 332(2):75–79. https://doi.org/10.1056/nejm199501123320202
Peterson AC, Chen Y (2012) Patient reported incontinence after radical prostatectomy is more common than expected and not associated with the nerve sparing technique: results from the Center for Prostate Disease Research (CPDR) database. Neurourol Urodyn 31(1):60–63. https://doi.org/10.1002/nau.21189
Foote J, Yun S, Leach GE (1991) Postprostatectomy incontinence. Pathophysiology, evaluation, and management. Urol Clin N Am 18(2):229–241
Herr HW (1994) Quality of life of incontinent men after radical prostatectomy. J Urol 151(3):652–654
Herschorn S, Bruschini H, Comiter C, Grise P, Hanus T, Kirschner-Hermanns R, Abrams P, Committee of the International Consultation on I (2010) Surgical treatment of stress incontinence in men. Neurourol Urodyn 29(1):179–190. https://doi.org/10.1002/nau.20844
Welk BK, Herschorn S (2012) The male sling for post-prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int 109(3):328–344. https://doi.org/10.1111/j.1464-410X.2010.10502.x
Warner JN, Grimsby GM, Tyson MD, Wolter CE (2012) Bladder capacity on preoperative urodynamics may impact outcomes on transobturator male slings. Neurourol Urodyn 31(7):1124–1127. https://doi.org/10.1002/nau.22233
Crites MA, Sorial A, Ghoniem GM (2011) Risk factors for male slings: a comparative study of two techniques. Urology 78(1):192–196. https://doi.org/10.1016/j.urology.2011.01.063
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 187(1):116–126
Winters JC (2011) Male slings in the treatment of sphincteric incompetence. Urol Clin N Am 38(1):73–81. https://doi.org/10.1016/j.ucl.2010.12.010 (vi–vii)
Barnard J, van Rij S, Westenberg AM (2014) A Valsalva leak-point pressure of >100 cmH O is associated with greater success in AdVance sling placement for the treatment of post-prostatectomy urinary incontinence. BJU Int. https://doi.org/10.1111/bju.12791
Moore K, Allen M, Voaklander DC (2004) Pad tests and self-reports of continence in men awaiting radical prostatectomy: establishing baseline norms for males. Neurourol Urodyn 23(7):623–626. https://doi.org/10.1002/nau.20067
Rehder P, Gozzi C (2007) Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol 52(3):860–866. https://doi.org/10.1016/j.eururo.2007.01.110
Lentz AC, Peterson AC, Webster GD (2012) Outcomes following artificial sphincter implantation after prior unsuccessful male sling. J Urol 187(6):2149–2153. https://doi.org/10.1016/j.juro.2012.01.119
Torrey R, Rajeshuni N, Ruel N, Muldrew S, Chan K (2013) Radiation history affects continence outcomes after advance transobturator sling placement in patients with post-prostatectomy incontinence. Urology 82(3):713–717. https://doi.org/10.1016/j.urology.2013.03.075
Davies TO, Bepple JL, McCammon KA (2009) Urodynamic changes and initial results of the AdVance male sling. Urology 74(2):354–357. https://doi.org/10.1016/j.urology.2008.12.082
Rehder P, Mitterberger MJ, Pichler R, Kerschbaumer A, Glodny B (2010) The 1 year outcome of the transobturator retroluminal repositioning sling in the treatment of male stress urinary incontinence. BJU Int 106(11):1668–1672. https://doi.org/10.1111/j.1464-410X.2010.09400.x
Inouye BM, Premo HA, Weil D, Peterson AC (2021) The male sling for stress urinary incontinence: tips and tricks for success. Int Braz J Urol Off J Braz Soc Urol 47(6):1131–1135. https://doi.org/10.1590/s1677-5538.Ibju.2020.1122
Borawski K, Rapoport D, Webster G (2010) Large volume pad weight is predictive of failure in treating post prostatectomy incontinence with the Advance sling. J Urol 183(4 SUPPL. 1):e587
Soljanik I, Gozzi C, Becker AJ, Stief CG, Bauer RM (2012) Risk factors of treatment failure after retrourethral transobturator male sling. World J Urol 30(2):201–206. https://doi.org/10.1007/s00345-011-0671-6
Rapoport D, Walter JR, Borawski KM, Webster GD (2009) The advance male sling: Predictors of success. J Urol 181(4 SUPPL. 1):619
Sturm RM, Guralnick ML, Stone AR, Bales GT, Dangle PP, O’Connor RC (2014) Comparison of clinical outcomes between “ideal” and “nonideal” transobturator male sling patients for treatment of postprostatectomy incontinence. Urology 83(5):1186–1188. https://doi.org/10.1016/j.urology.2013.12.061
Ajay D, Selph J, Belsante M, Zhang H, Lentz A, Le N-B, Webster G, Peterson A (2015) PD24-12 low cystometric capacity is associated with male transobturator sling failure and does not correlate with the voiding diary; pre-operative urodynamics are helpful in the evaluation of urinary incontinence. J Urol 193(4S):e490–e491. https://doi.org/10.1016/j.juro.2015.02.1467
Ajay D, Madden-Fuentes RJ, Peterson AC (2018) Detrusor overactivity on preoperative urodynamics better predicts male transobturator sling failure than clinical findings of urgency. In: Paper presented at the 82nd annual SESAUA conference, Orlando, Florida
Chung ASJ, Suarez OA, McCammon KA (2017) AdVance male sling. Transl Androl Urol 6(4):674–681. https://doi.org/10.21037/tau.2017.07.29
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Divya Ajay—none. Arman A. Kahokehr—none. Aaron C. Lentz—Consultant Boston Scientific and Coloplast. Andrew C. Peterson—consultant Boston Scientific.
Research involving human participants and/or animals
None.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ajay, D., Kahokehr, A.A., Lentz, A.C. et al. Valsalva leak point pressure (VLPP) greater than 70 cm H2O is an indicator for sling success: a success prediction model for the male transobturator sling. Int Urol Nephrol 54, 1499–1503 (2022). https://doi.org/10.1007/s11255-022-03222-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03222-4