Abstract
Background
The American Association for the Surgery of Trauma (AAST) splenic organ injury scale (OIS) is the most frequently used CT-based grading system for blunt splenic trauma. However, reported inter-rater agreement is modest, and an algorithm that objectively automates grading based on transparent and verifiable criteria could serve as a high-trust diagnostic aid.
Purpose
To pilot the development of an automated interpretable multi-stage deep learning-based system to predict AAST grade from admission trauma CT.
Methods
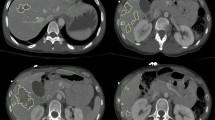
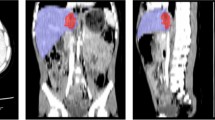
Our pipeline includes 4 parts: (1) automated splenic localization, (2) Faster R-CNN-based detection of pseudoaneurysms (PSA) and active bleeds (AB), (3) nnU-Net segmentation and quantification of splenic parenchymal disruption (SPD), and (4) a directed graph that infers AAST grades from detection and segmentation results. Training and validation is performed on a dataset of adult patients (age ≥ 18) with voxelwise labeling, consensus AAST grading, and hemorrhage-related outcome data (n = 174).
Results
AAST classification agreement (weighted κ) between automated and consensus AAST grades was substantial (0.79). High-grade (IV and V) injuries were predicted with accuracy, positive predictive value, and negative predictive value of 92%, 95%, and 89%. The area under the curve for predicting hemorrhage control intervention was comparable between expert consensus and automated AAST grading (0.83 vs 0.88). The mean combined inference time for the pipeline was 96.9 s.
Conclusions
The results of our method were rapid and verifiable, with high agreement between automated and expert consensus grades. Diagnosis of high-grade lesions and prediction of hemorrhage control intervention produced accurate results in adult patients.



Similar content being viewed by others
References
Dreizin D, Munera F (2012) Blunt polytrauma: evaluation with 64-section whole-body CT angiography. Radiographics 32(3):609–631
Chahine AH, Gilyard S, Hanna TN, Fan S, Risk B, Johnson JO, Duszak R Jr, Newsome J, Xing M, Kokabi N (2021) Management of splenic trauma in contemporary clinical practice: a national trauma data bank study. Acad Radiol 28:S138–S147
Dreizin D, Champ K, Dattwyler M, Bodanapally U, Smith EB, Li G, Singh R, Wang Z, Liang Y (2022) Blunt splenic injury in adults: association between volumetric quantitative CT parameters and intervention. J Trauma Acute Care Surg. https://doi.org/10.1097/ta.0000000000003684
Zarzaur BL, Kozar R, Myers JG, Claridge JA, Scalea TM, Neideen TA, Maung AA, Alarcon L, Corcos A, Kerwin A (2015) The splenic injury outcomes trial: an American Association for the Surgery of Trauma multi-institutional study. J Trauma Acute Care Surg 79(3):335–342
Haan JM, Biffl W, Knudson MM, Davis KA, Oka T, Majercik S, Dicker R, Marder S, Scalea TM (2004) Committee WTAM-IT Splenic embolization revisited: a multicenter review. J Trauma Acute Care Surg 56(3):542–547
Krausz MM, Hirsh M (2003) Bolus versus continuous fluid resuscitation and splenectomy for treatment of uncontrolled hemorrhagic shock after massive splenic injury. J Trauma Acute Care Surg 55(1):62–68
Zarzaur BL, Kozar RA, Fabian TC, Coimbra R (2011) A survey of American Association for the Surgery of Trauma member practices in the management of blunt splenic injury. J Trauma Acute Care Surg 70(5):1026–1031
Barquist ES, Pizano LR, Feuer W, Pappas PA, McKenney KA, LeBlang SD, Henry RP, Rivas LA, Cohn SM (2004) Inter-and intrarater reliability in computed axial tomographic grading of splenic injury: why so many grading scales? J Trauma Acute Care Surg 56(2):334–338
Clark R, Hird K, Misur P, Ramsay D, Mendelson R (2011) CT grading scales for splenic injury: Why can’t we agree? J Med Imaging Radiat Oncol 55(2):163–169
Banaste N, Caurier B, Bratan F, Bergerot J-F, Thomson V, Millet I (2018) Whole-body CT in patients with multiple traumas: factors leading to missed injury. Radiology 289(2):374–383
Watchorn J, Miles R, Moore N (2013) The role of CT angiography in military trauma. Clin Radiol 68(1):39–46
Glover M IV, Almeida RR, Schaefer PW, Lev MH, Mehan WA Jr (2017) Quantifying the impact of noninterpretive tasks on radiology report turn-around times. J Am Coll Radiol 14(11):1498–1503
Hunter TB, Taljanovic MS, Krupinski E, Ovitt T, Stubbs AY (2007) Academic radiologists’ on-call and late-evening duties. J Am Coll Radiol 4(10):716–719
Hanna TN, Loehfelm T, Khosa F, Rohatgi S, Johnson J-O (2016) Overnight shift work: factors contributing to diagnostic discrepancies. Emerg Radiol 23(1):41–47
Cruz-Romero C, Agarwal S, Abujudeh HH, Thrall J, Hahn PF (2016) Spleen volume on CT and the effect of abdominal trauma. Emerg Radiol 23(4):315–323
Wood A, Soroushmehr SR, Farzaneh N, Fessell D, Ward KR, Gryak J, Kahrobaei D, Na K. Fully automated spleen localization and segmentation using machine learning and 3D active contours. 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC): IEEE, 2018; p. 53–56.
Dandin O, Teomete U, Osman O, Tulum G, Ergin T, Sabuncuoglu MZ (2016) Automated segmentation of the injured spleen. Int J Comput Assist Radiol Surg 11(3):351–368
Wang J, Wood A, Gao C, Najarian K, Gryak J (2021) Automated Spleen Injury Detection Using 3D Active Contours and Machine Learning. Entropy 23(4):382
Teomete U, Tulum G, Ergin T, Cuce F, Koksal M, Dandin O, Osman O (2018) Automated computer-aided diagnosis of splenic lesions due to abdominal trauma. Hippokratia 22(2):80
DeGrave AJ, Janizek JD, Lee S-I (2021) AI for radiographic COVID-19 detection selects shortcuts over signal. Nature Machine Intelligence 3(7):610–619
Zapaishchykova A, Dreizin D, Li Z, Wu JY, Roohi SF, Unberath M. An interpretable approach to automated severity scoring in pelvic trauma. arXiv preprint arXiv:210510238 2021.
Chen H, Gomez C, Huang C-M, Unberath M. INTRPRT: A systematic review of and guidelines for designing and validating transparent AI in medical image analysis. arXiv preprint arXiv:211212596 2021.
Vlontzos A, Rueckert D, Kainz B. A review of causality for learning algorithms in medical image analysis. arXiv preprint arXiv:220605498 2022.
Arrieta AB, Díaz-Rodríguez N, Del Ser J, Bennetot A, Tabik S, Barbado A, García S, Gil-López S, Molina D, Benjamins R (2020) Explainable Artificial Intelligence (XAI): concepts, taxonomies, opportunities and challenges toward responsible AI. Information fusion 58:82–115
Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, Kaups K, Schuster K, Tominaga GT, Committee APA (2018) Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg 85(6):1119–1122
Boscak AR, Shanmuganathan K, Mirvis SE, Fleiter TR, Miller LA, Sliker CW, Steenburg SD, Alexander M (2013) Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology 268(1):79–88
Uyeda JW, LeBedis CA, Penn DR, Soto JA, Anderson SW (2014) Active hemorrhage and vascular injuries in splenic trauma: utility of the arterial phase in multidetector CT. Radiology 270(1):99–106
Zhou Y, Dreizin D, Wang Y, Liu F, Shen W, Yuille AL. External attention assisted multi-phase splenic vascular injury segmentation with limited data. IEEE Transactions on Medical Imaging 2021.
Antonelli M, Reinke A, Bakas S, Farahani K, Landman BA, Litjens G, Menze B, Ronneberger O, Summers RM, van Ginneken B. The medical segmentation decathlon. arXiv preprint arXiv:210605735 2021.
Cooney R, Ku J, Cherry R, Maish GO III, Carney D, Scorza LB, Smith JS (2005) Limitations of splenic angioembolization in treating blunt splenic injury. J Trauma Acute Care Surg 59(4):926–932
Bhullar IS, Frykberg ER, Siragusa D, Chesire D, Paul J, Tepas JJ III, Kerwin AJ (2012) Selective angiographic embolization of blunt splenic traumatic injuries in adults decreases failure rate of nonoperative management. J Trauma Acute Care Surg 72(5):1127–1134
Crichton JCI, Naidoo K, Yet B, Brundage SI, Perkins Z (2017) The role of splenic angioembolization as an adjunct to nonoperative management of blunt splenic injuries: a systematic review and meta-analysis. J Trauma Acute Care Surg 83(5):934–943
Requarth JA, D’Agostino RB Jr, Miller PR (2011) Nonoperative management of adult blunt splenic injury with and without splenic artery embolotherapy: a meta-analysis. J Trauma Acute Care Surg 71(4):898–903
Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR (1995) Organ injury scaling: spleen and liver (1994 revision). J Trauma Acute Care Surg 38(3):323–324
Haan JM, Bochicchio GV, Kramer N, Scalea TM (2005) Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma Acute Care Surg 58(3):492–498
Miller PR, Chang MC, Hoth JJ, Mowery NT, Hildreth AN, Martin RS, Holmes JH, Meredith JW, Requarth JA (2014) Prospective trial of angiography and embolization for all grade III to V blunt splenic injuries: nonoperative management success rate is significantly improved. J Am Coll Surg 218(4):644–648
Ren S, He K, Girshick R, Sun J. Faster r-cnn: Towards real-time object detection with region proposal networks. Advances in neural information processing systems 2015;28.
Isensee F, Jaeger PF, Kohl SA, Petersen J, Maier-Hein KH (2021) nnU-Net: a self-configuring method for deep learning-based biomedical image segmentation. Nat Methods 18(2):203–211
Xie Q, Luong M-T, Hovy E, Le QV. Self-training with noisy student improves imagenet classification. Proceedings of the IEEE/CVF conference on computer vision and pattern recognition2020; p. 10687–10698.
Consortium M. Project MONAI. Zenodo. Available online: https://zenodoorg/record/4323059#YXaMajgzaUk (accessed on 25 May 2020) 2020.
Ronneberger O, Fischer P, Brox T. U-net: Convolutional networks for biomedical image segmentation. International Conference on Medical image computing and computer-assisted intervention: Springer, 2015; p. 234–241.
Lin T-Y, Maire M, Belongie S, Hays J, Perona P, Ramanan D, Dollár P, Zitnick CL (2014) Microsoft coco: Common objects in context. Springer, European conference on computer vision, pp 740–755
Zhang R, Tian Z, Shen C, You M, Yan Y. Mask encoding for single shot instance segmentation. Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition2020; p. 10226–10235.
Wu Y, Kirillov A, Massa F, Lo W-Y, Girshick R. Detectron2 (2019). 2019.
Bhangu A, Nepogodiev D, Lal N, Bowley DM (2012) Meta-analysis of predictive factors and outcomes for failure of non-operative management of blunt splenic trauma. Injury 43(9):1337–1346
Dreizin D, Yu T, Motley K, Li G, Morrison JJ, Liang Y. Blunt splenic injury: assessment of follow-up CT utility using quantitative volumetry. Frontiers in radiology 2022:23.
Dreizin D, Chen T, Liang Y, Zhou Y, Paes F, Wang Y, Yuille AL, Roth P, Champ K, Li G. Added value of deep learning-based liver parenchymal CT volumetry for predicting major arterial injury after blunt hepatic trauma: a decision tree analysis. Abdominal Radiology 2021:1–11.
Dreizin D, Zhou Y, Fu S, Wang Y, Li G, Champ K, Siegel E, Wang Z, Chen T, Yuille AL (2020) A multiscale deep learning method for quantitative visualization of traumatic hemoperitoneum at CT: assessment of feasibility and comparison with subjective categorical estimation. Radiology Artificial Intelligence 2(6):e190220
Dreizin D, Zhou Y, Chen T, Li G, Yuille AL, McLenithan A, Morrison JJ (2020) Deep learning-based quantitative visualization and measurement of extraperitoneal hematoma volumes in patients with pelvic fractures: potential role in personalized forecasting and decision support. J Trauma Acute Care Surg 88(3):425–433
Dreizin D, Zhou Y, Zhang Y, Tirada N, Yuille AL (2020) Performance of a deep learning algorithm for automated segmentation and quantification of traumatic pelvic hematomas on CT. J Digit Imaging 33(1):243–251
Dreizin D, Nixon B, Hu J, Albert B, Yan C, Yang G, Chen H, Liang Y, Kim N, Jeudy J. A pilot study of deep learning-based CT volumetry for traumatic hemothorax. Emergency Radiology 2022:1–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. biometrics 1977:159–174.
Morell-Hofert D, Primavesi F, Fodor M, Gassner E, Kranebitter V, Braunwarth E, Haselbacher M, Nitsche UP, Schmid S, Blauth M (2020) Validation of the revised 2018 AAST-OIS classification and the CT severity index for prediction of operative management and survival in patients with blunt spleen and liver injuries. Eur Radiol 30(12):6570–6581
Jeavons C, Hacking C, Beenen LF, Gunn ML (2018) A review of split-bolus single-pass CT in the assessment of trauma patients. Emerg Radiol 25(4):367–374
Beenen LF, Sierink JC, Kolkman S, Nio CY, Saltzherr TP, Dijkgraaf MG, Goslings JC (2015) Split bolus technique in polytrauma: a prospective study on scan protocols for trauma analysis. Acta Radiol 56(7):873–880
Lopez JM Jr, McGonagill PW, Gross JL, Hoth JJ, Chang MC, Parker K, Requarth JA, Miller PR (2015) Subcapsular hematoma in blunt splenic injury: a significant predictor of failure of nonoperative management. J Trauma Acute Care Surg 79(6):957–960
Scatamacchia SA, Raptopoulos V, Fink MP, Silva WE (1989) Splenic trauma in adults: impact of CT grading on management. Radiology 171(3):725–729
Rowell SE, Biffl WL, Brasel K, Moore EE, Albrecht RA, DeMoya M, Namias N, Schreiber MA, Cohen MJ, Shatz DV (2017) Western Trauma Association Critical Decisions in Trauma: Management of adult blunt splenic trauma—2016 updates. J Trauma Acute Care Surg 82(4):787–793
Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, Moore EE, Reva V, Bing C, Bala M, Fugazzola P (2017) Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 12(1):1–26
Boscak A, Shanmuganathan K (2012) Splenic trauma: what is new? Radiologic Clinics 50(1):105–122
Lee JT, Slade E, Uyeda J, Steenburg SD, Chong ST, Tsai R, Raptis D, Linnau KF, Chinapuvvula NR, Dattwyler MP (2021) American Society of Emergency Radiology multicenter blunt splenic trauma study: CT and clinical findings. Radiology 299(1):122
Funding
NIH K08 EB027141-01A1 (PI: David Dreizin, MD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mathias Unberath is the co-last author.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, H., Unberath, M. & Dreizin, D. Toward automated interpretable AAST grading for blunt splenic injury. Emerg Radiol 30, 41–50 (2023). https://doi.org/10.1007/s10140-022-02099-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-022-02099-1