Abstract
Introduction
BMI and hernia defect size are strongly associated with outcomes after open ventral hernia repair (OVHR). The impact of abdominal subcutaneous fat (SQV), intra-abdominal volume (IAV), hernia volume (HV), and ratio of HV to intra-abdominal volume (HV:IAV, representing visceral eventration) is less clearly elucidated. This study examines the interaction of multiple markers of adiposity and hernia size in OVHR.
Methods
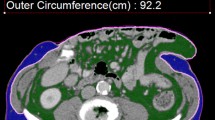
OVHR with preoperative CT scans were identified. 3D volumetric software measured HV, SQV, IAV, and HV:IAV was calculated. A principal component analysis was performed to create new component variables for collinear variables. Hernia PC was composed primarily of hernia dimensions, EAV (extra-abdominal volume PC) included SQV and BMI, and IAV PC included IAV.
Results
A total of 1178 OVHR patients had a preoperative CT scan. Their demographics included a mean age of 58.5 ± 12.4 years, BMI of 34.2 ± 7.7 kg/m2, and 57.8% were female. The mean defect area was 150.8 ± 136.7 cm2, and 66.0% were recurrent, Patients had mean SQV of 6719.4 ± 3563.9 cm3, HV of 966.9 ± 1303.5 cm3, IAV of 4250.2 ± 2118.1 cm3, and a HV:IAV of 0.29 ± 0.46. In multivariate analysis, Hernia PC was associated with panniculectomy (OR 1.52, CI 1.37–1.69) and component separation (OR 1.34, CI 1.21–1.49) and was negatively associated with fascial closure (OR 0.78, CI 0.69–0.88). Hernia PC was also associated with reoperation, readmission, and development of wound complications (OR 1.18, CI 1.08–1.30; OR 1.15, CI 1.04–1.27; OR 1.28, CI 1.16–1.41, respectively). EAV PC was associated with performance of a panniculectomy (OR 1.33, CI 1.20–1.48), readmission (OR 1.18, CI 1.06–1.32), and wound complications (OR 1.41, CI 1.27–1.57). IAV PC was not associated with adverse outcomes.
Conclusion
Values of hernia area, volume, IAV, HV:IAV, BMI, and SQV are collinear markers of patient obesity and hernia proportions. They are distinct enough to be represented by three principal component variables, indicating more nuanced discrete influences on variability of surgical outcomes other than BMI.
Similar content being viewed by others
References
Pearson DG, Carbonell AM (2018) Obesity and abdominal wall reconstruction. Plast Reconstr Surg 142(3 Suppl):30S–35S. https://doi.org/10.1097/PRS.0000000000004845
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238(3):391–400. https://doi.org/10.1097/01.sla.0000086662.49499.ab
Cox TC, Blair LJ, Huntington CR et al (2016) The cost of preventable comorbidities on wound complications in open ventral hernia repair. J Surg Res 206(1):214–222. https://doi.org/10.1016/j.jss.2016.08.009
Lambert DM, Marceau S, Forse RA (2005) Intra-abdominal pressure in the morbidly obese. Obes Surg 15(9):1225–1232. https://doi.org/10.1381/096089205774512546
Sugerman H, Windsor A, Bessos M, Wolfe L (1997) Intra-abdominal pressure, sagittal abdominal diameter and obesity comorbidity. J Intern Med 241(1):71–79
Agnew SP, Small W, Wang E, Smith LJ, Hadad I, Dumanian GA (2010) Prospective measurements of intra-abdominal volume and pulmonary function after repair of massive ventral hernias with the components separation technique. Ann Surg 251(5):981–988. https://doi.org/10.1097/SLA.0b013e3181d7707b
Gaidukov KM, Raibuzhis EN, Hussain A et al (2013) Effect of intra-abdominal pressure on respiratory function in patients undergoing ventral hernia repair. World J Crit Care Med 2(2):9. https://doi.org/10.5492/wjccm.v2.i2.9
Blatnik JA, Krpata DM, Pesa NL et al (2012) Predicting severe postoperative respiratory complications following abdominal wall reconstruction. Plast Reconstr Surg 130(4):836–841. https://doi.org/10.1097/PRS.0b013e318262f160
Blair LJ, Ross SW, Huntington CR et al (2015) Computed tomographic measurements predict component separation in ventral hernia repair. J Surg Res 199(2):420–427. https://doi.org/10.1016/j.jss.2015.06.033
Fujii T, Tsutsumi S, Matsumoto A et al (2010) Thickness of subcutaneous fat as a strong risk factor for wound infections in elective colorectal surgery: impact of prediction using preoperative CT. Dig Surg 27(4):331–335. https://doi.org/10.1159/000297521
Wormer BA, Walters AL, Bradley JF 3rd et al (2013) Does ventral hernia defect length, width, or area predict postoperative quality of life? Answers from a prospective, international study. J Surg Res 184(1):169–177. https://doi.org/10.1016/j.jss.2013.04.034
Franklin BR, Patel KM, Nahabedian MY, Baldassari LE, Cohen EI, Bhanot P (2013) Predicting abdominal closure after component separation for complex ventral hernias: maximizing the use of preoperative computed tomography. Ann Plast Surg 71(3):261–265. https://doi.org/10.1097/SAP.0b013e3182773915
Winters H, Knaapen L, Buyne OR et al (2019) Pre-operative CT scan measurements for predicting complications in patients undergoing complex ventral hernia repair using the component separation technique. Hernia. https://doi.org/10.1007/s10029-019-01899-8
Xu Z, Asman AJ, Baucom RB, Abramson RG, Poulose BK, Landman BA (2015) Quantitative CT imaging of ventral hernias: preliminary validation of an anatomical labeling protocol. PLoS ONE 10(10):e0141671. https://doi.org/10.1371/journal.pone.0141671
Anderson KM, Lindler TU, Lamberton GR, Baron PW, Ojogho OK, Baldwin DD (2008) Laparoscopic donor nephrectomy: effect of perirenal fat upon donor operative time. J Endourol 22(10):2269–2274. https://doi.org/10.1089/end.2008.9725
Aquina CT, Rickles AS, Probst CP et al (2015) Visceral obesity, not elevated BMI, is strongly associated with incisional hernia after colorectal surgery. Dis Colon Rectum 58(2):220–227. https://doi.org/10.1097/DCR.0000000000000261
Balentine CJ, Marshall C, Robinson C et al (2010) Validating quantitative obesity measurements in colorectal cancer patients. J Surg Res 164(1):18–22. https://doi.org/10.1016/j.jss.2010.05.048
Rickles AS, Iannuzzi JC, Mironov O et al (2013) Visceral obesity and colorectal cancer: are we missing the boat with BMI? J Gastrointest Surg 17(1):133–143. https://doi.org/10.1007/s11605-012-2045-9
Azar FK, Crawford TC, Poruk KE et al (2017) Ventral hernia repair in patients with abdominal loss of domain: an observational study of one institution’s experience. Hernia 21(2):245–252. https://doi.org/10.1007/s10029-017-1576-0
Parker SG, Halligan S, Blackburn S et al (2019) What exactly is meant by “Loss of Domain” for ventral hernia? Systematic review of definitions. World J Surg 43(2):396–404. https://doi.org/10.1007/s00268-018-4783-7
Demerath EW, Reed D, Rogers N et al (2008) Visceral adiposity and its anatomical distribution as predictors of the metabolic syndrome and cardiometabolic risk factor levels. Am J Clin Nutr 88(5):1263–1271. https://doi.org/10.3945/ajcn.2008.26546
Shimizu A, Tani M, Kawai M et al (2011) Influence of visceral obesity for postoperative pulmonary complications after pancreaticoduodenectomy. J Gastrointest Surg 15(8):1401–1410. https://doi.org/10.1007/s11605-011-1436-7
Maloney SR, Schlosser KA, Prasad T et al (2019) Twelve years of component separation technique (CST) in abdominal wall reconstruction (AWR). Surgery. (in press)
Funding
This research has no direct funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Paul D Colavita MD is a speaker with Allergan. Vedra A Augenstein MD is a speaker with Allergan, Intuitive, Acelity, WL Gore. B Todd Heniford MD is a speaker with Allergan, and in advisory committee for WL Gore.Kathryn A Schlosser MD, Sean R Maloney MD, and Tanushree Prasad MA have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlosser, K.A., Maloney, S.R., Prasad, T. et al. Three-dimensional hernia analysis: the impact of size on surgical outcomes. Surg Endosc 34, 1795–1801 (2020). https://doi.org/10.1007/s00464-019-06931-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06931-7