Abstract
Objectives
Although laparoscopic posterior fundoplication (LPF) i.e., Nissen or Toupet have the proven efficacy for controlling gastro-esophageal reflux surgically, there remain problems with postoperative dysphagia and gas bloat syndrome. To decrease some of these postoperative complications, laparoscopic anterior fundoplication (LAF) was introduced. The aim of this study was to conduct a meta-analysis and systematic review of randomized controlled trials (RCTs) to investigate the merits and drawbacks of LPF versus LAF for the treatment of gastro-esophageal reflux disease (GERD).
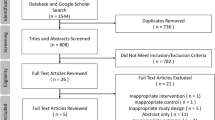
Data Sources, Study Selection, and Review Methods
A search of Medline, Embase, Science Citation Index, Current Contents, PubMed, ISI Web of Science, and the Cochrane Database identified all RCTs comparing different types of LPF and LAF published in the English Language between 1990 and 2013. The meta-analysis was prepared in accordance with the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) statement. Data was extracted and analyzed on ten variables which include dysphagia score, heartburn rate, redo operative rate, operative time, overall complications, rate of conversion to open, Visick grading of satisfaction, overall satisfaction, length of hospital stay, and postoperative 24-h pH scores.
Data Synthesis
Nine trials totaling 840 patients (anterior = 425, posterior = 415) were analyzed. There was a significant reduction in the odds ratio for dysphagia in the LAF group compared to the LPF group. Conversely, significant reduction in the odds ratio for heartburn was observed for LPF compared to LAF. Comparable effects were noted for both groups for other variables which include redo surgery, operating time, overall complications, conversion rate, Visick’s grading, patients’ satisfaction, length of hospital stay, and postoperative 24-h pH scores.
Conclusions
Based on this meta-analysis, LPF compared to LAF is associated with significant reduction in heartburn at the expense of higher dysphagia rate on a short- and medium-term basis. We therefore conclude that LPF is a better alternative to LAF for controlling GERD symptoms.












Similar content being viewed by others
References
Peters MJ, Mukhtar A, Yunus RM, Khan S, Pappalardo J, Memon B, Memon MA (2009) Meta-analysis of randomized clinical trials comparing open and laparoscopic anti-reflux surgery. Am J Gastroenterol 104(6):1548–1561
McKenzie D, Grayson T, Polk HC Jr (1996) The impact of omeprazole and laparoscopy upon hiatal hernia and reflux oesophagitis. J Am Coll Surg 183(4):413–418
Klaus A, Hinder RA, DeVault KR, Achem SR (2003) Bowel dysfunction after laparoscopic antireflux surgery: incidence, severity, and clinical course. Am J Med 114(1):6–9
Spechler SJ (1992) Comparision of medical and surgical therapy for complicated gastroesophageal reflux disease in veterans. The Department of Veterans Affairs Gastroesophageal Reflux Disease Study Group. N Engl J Med 326(12):786–792
Bais JE, Bartelsman JF, Bonjer HJ, Cuesta MA, Go PM, Klinkenberg-Knol EC, van Lanschot JJ, Nadorp JH, Smout AJ, van der Graaf Y, Gooszen HG (2000) Laparoscopic or conventional Nissen Fundoplication for gastro-oesophageal reflux disease: randomised clinical trial. The Netherlands Antireflux Surgery Study Group. Lancet 355(9199):170–174
Wills VL, Hunt DR (2001) Dysphagia after antireflux surgery. Br J Surg 88(4):486–499
Catarci M, Gentileschi P, Papi C, Carrara A, Marrese R, Gaspari AL, Grassi GB (2004) Evidence-based appraisal of antireflux fundoplication. Ann Surg 239(3):325–337
Bell RC, Hanna P, Powers B, Sabel J, Hruza D (1996) Clinical and manometric results of laparoscopic partial (Toupet) and complete (Rosetti-Nissen) fundoplication. Surg Endosc 10(7):724–728
O’Reilly MJ, Mullins SG, Saye WB, Pinto SE, Falkner PT (1996) Laparoscopic posterior partial fundoplication: analysis of 100 consecutive cases. Laparoendosc Surg 6(3):141–150
Watson A, Jenkinson LR, Ball CS, Barlow AP, Norris TL (1991) A more physiological alternative to total fundoplication for the surgical correction of resistant gastro-oesophageal reflux. Br J Surg 78(9):1088–1094
Watson A, Spychal RT, Brown MG, Peck N, Callander N (1995) Laparoscopic ‘physiological’ antireflux procedure: preliminary results of a prospective symptomatic and objective study. Br J Surg 82(5):651–656
Rice S, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG (2006) Laparoscopic anterior 180 degrees partial fundoplication: five-year results and beyond. Arch Surg 141(3):271–275
Watson DI, Jamieson GG, Pike GK, Davies N, Richardson M, Devitt PG (1999) Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg 86(1):123–130
Hagedorn C, Jönson C, Lönroth H, Ruth M, Thune A, Lundell L (2003) Efficacy of an anterior as compared with a posterior laparoscopic partial fundoplication: results of a randomized, controlled clinical trial. Ann Surg 238(2):189–196
Watson DI, Jamieson GG, Lally C, Archer S, Bessell JR, Booth M, Cade R, Cullingford G, Devitt PG, Fletcher DR, Hurley J, Kiroff G, Martin CJ, Martin IJ, Nathanson LK, Windsor JA, International Society for Diseases of the Esophagus-Australasian Section (2004) Multicenter, prospective, double-blind, randomized trial of laparoscopic nissen vs anterior 90 degrees partial fundoplication. Arch Surg 139(11):1160–1167
Chrysos E, Athanasakis E, Pechlivanides G, Tzortzinis A, Mantides A, Xynos E (2004) The effect of total and anterior partial fundoplication on antireflux mechanisms of the gastroesophageal junction. Am J Surg 188(1):39–44
Baigrie RJ, Cullis SN, Ndhluni AJ, Cariem A (2005) Randomized double-blind trial of laparoscopic Nissen fundoplication versus anterior partial fundoplication. Br J Surg 92(7):819–823
Spence GM, Watson DI, Jamiesion GG, Lally CJ, Devitt PG (2006) Single center prospective randomized trial of laparoscopic Nissen versus anterior 90 degrees fundoplication. J Gastrointest Surg 10(5):698–705
Khan M, Smythe A, Globe J, Stoddard CJ, Ackroyd R (2010) Randomized controlled trial of laparoscopic anterior versus posterior fundoplication for gastro-oesophageal reflux disease. ANZ J Surg 80(7–8):500–505
Raue W, Ordemann J, Jacobi CA, Menenakos C, Buchholz A, Hartmann J (2011) Nissen versus Dor fundoplication for treatment of gastroesophageal reflux disease: a blinded randomized clinical trial. Dig Surg 28(1):80–86
Cao Z, Cai W, Qin M, Zhao H, Yue P, Li Y (2012) Randomized clinical trial of laparoscopic anterior 180° partial versus 360° Nissen fundoplication: 5 year results. Dis Esophagus 25(2):114–120
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF (1999) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. International Society for Diseases of the Esophagus-Australasian Section. Lancet 354(9193):1896–1900
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):1–34
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12
Liu IM, Agresti A (1996) Mantel-Haenszel-type inference for cumulative odds ratios with a stratified ordinal response. Biometrics 52(4):1223–1234
Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F (2000) Methods for meta-analysis in medical research. Wiley, Chichester
Hedges LV, Olkin I (1985) Statistical methods for meta analysis. Academic Press, Orlando
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J (2006) Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11(2):193–206
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):13
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Foundation for Statistical computing (2008) R: A language and environment for statistical computing [computer program] Version 2.8.0. Foundation for Statistical computing, Vienna
Lumley T (2011) The rmeta Package Version 2.14. http://cran.rproject.org/web/packages/rmeta/index.html (Accessed April 22, 2011)
Anderson JA, Myers JC, Watson DI, Gabb M, Mathew G, Jamieson GG (1998) Concurrent fluoroscopy and manometry reveal differences in laparoscopic Nissen and anterior fundoplication. Dig Dis Sci 43(4):847–853
Hagedorn C, Lönroth H, Rydberg L, Ruth M, Lundell L (2002) Long-term efficacy of total (Nissen-Rossetti) and posterior partial (Toupet) fundoplication: results of a randomized clinical trial. J Gastrointest Surg 6(4):540–545
Mardani J, Lundell L, Engstrom C (2011) Total or posterior partial fundoplication in the treatment of GERD. Results of a randomized trial after 2 decades of follow-up. Ann Surg 253:875–878
Broeders JAJL, Mauritz FA, Ahmed Ali U, Draaisma WA, Ruurda JP, Gooszen HG, Smout AJPM, Broeders IAMJ, Hazebrock EJ (2010) Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Brit J Surg 97(9):1318–1330
Ludemann R, Watson DI, Jamieson GG, Game PA, Devitt PG (2005) Five-year follow-up of a randomized clinical trial of laparoscopic total versus anterior 180 degrees fundoplication. Br J Surg 92(2):240–243
Cai W, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG (2008) Ten-year clinical outcome of a prospective randomized clinical trial of laparoscopic Nissen versus anterior 180 (degrees) partial fundoplication. Br J Surg 95(12):1501–1505
Broeders JA, Broeders EA, Watson DI, Devin PG, Holloway RH, Jamieson GG (2013) Objective outcomes 14 years after laparoscopic anterior 180-degree partial versus Nissen fundoplication. Results from a randomized trial. Ann Surg 258(2):233–239
Nijjar RS, Watson DI, Archer S, Bessell JR, Booth M, Cade R, Cullingford GL, Devitt PG, Flecher DR, Hurley J, Kiroff G, Martin IJG, Nathanson LK, Windsor JA, for the International Society for the Diseases of the Esophagus-Australasian Section (2010) Five-year follow-up of multicenter, double-blind randomized clinical trial of laparoscopic Nissen vs anterior 90o partial fundoplication. Arch Surg 145:552–557
Engström C, Lönroth H, Mardani J, Lundell L (2007) An anterior or posterior approach to partial fundoplication? Long-term results of a randomized trial. World J Surg 31(6):1215–1221. doi:10.1007/s00268-007-9004-8
Fein M, Bueter M, Thalheimer A, Pachmayr V, Heimbucher J, Freys SM, Fuchs KH (2008) Less reflux recurrence following Nissen fundoplication: results of laparoscopic antireflux surgery after 10 years. Chirurg 79(8):759–764
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Stern JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemol 54:1046–1055
Ioannidis JP, Lau J (1998) Can quality of clinical trials and meta-analyses be quantified? Lancet 352:590–591
Ng TT, McGory ML, Ko CY, Maggard MA (2006) Meta-analysis in surgery: methods and limitations. Arch Surg 141:1125–1130
Smith GD, Egger M (1998) Incommunicable knowledge? Interpreting and applying the results of clinical trials and meta-analyses. J Clin Epidemiol 51:289–295
Ioannidis JP, Patsopoulos NA, Evangelou E (2007) Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335:914–916
Doubilet P, Weinstein MC, McNeal BJ (1986) Use and misuse of the term “cost-effectiveness” in medicine. N Engl J Med 314:253–256
Ludemann R, Watson DI, Jamieson GG (2003) Influence of follow-up methodology and completeness on apparent clinical outcome of fundoplication. Am J Surg 186(2):143–147
Acknowledgements
None.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Memon, M.A., Subramanya, M.S., Hossain, M.B. et al. Laparoscopic Anterior Versus Posterior Fundoplication for Gastro-esophageal Reflux Disease: A Meta-analysis and Systematic Review. World J Surg 39, 981–996 (2015). https://doi.org/10.1007/s00268-014-2889-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2889-0