Abstract
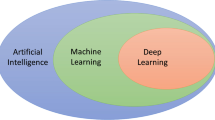
Artificial intelligence (AI) and deep learning have multiple potential uses in aiding the musculoskeletal radiologist in the radiological evaluation of orthopedic implants. These include identification of implants, characterization of implants according to anatomic type, identification of specific implant models, and evaluation of implants for positioning and complications. In addition, natural language processing (NLP) can aid in the acquisition of clinical information from the medical record that can help with tasks like prepopulating radiology reports. Several proof-of-concept works have been published in the literature describing the application of deep learning toward these various tasks, with performance comparable to that of expert musculoskeletal radiologists. Although much work remains to bring these proof-of-concept algorithms into clinical deployment, AI has tremendous potential toward automating these tasks, thereby augmenting the musculoskeletal radiologist.







Similar content being viewed by others
References
Gyftopoulos S, Lin D, Knoll F, Doshi AM, Rodrigues TC, Recht MP. Artificial intelligence in musculoskeletal imaging: current status and future directions. Am J Roentgenol. American Roentgen Ray Society; 2019 [cited 2021 Mar 17]. p. 506–13. Available from: https://pubmed.ncbi.nlm.nih.gov/31166761/.
Knoll F, Murrell T, Sriram A, Yakubova N, Zbontar J, Rabbat M, et al. Advancing machine learning for MR image reconstruction with an open competition: overview of the 2019 fastMRI challenge. Magn Reson Med. John Wiley and Sons Inc.; 2020 [cited 2021 Mar 17];84:3054–70. Available from: https://pubmed.ncbi.nlm.nih.gov/32506658/.
Bien N, Rajpurkar P, Ball RL, Irvin J, Park A, Jones E, et al. Deep-learning-assisted diagnosis for knee magnetic resonance imaging: development and retrospective validation of MRNet. PLoS Med. PLoS Med; 2018 [cited 2020 Jun 23];15:e1002699. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30481176.
Urakawa T, Tanaka Y, Goto S, Matsuzawa H, Watanabe K, Endo N. Detecting intertrochanteric hip fractures with orthopedist-level accuracy using a deep convolutional neural network. Skeletal Radiol. 2018 [cited 2018 Aug 13]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/29955910.
Lindsey R, Daluiski A, Chopra S, Lachapelle A, Mozer M, Sicular S, et al. Deep neural network improves fracture detection by clinicians. Proc Natl Acad Sci. 2018 [cited 2019 Nov 9];115:11591–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30348771.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg. 2007 [cited 2020 Jan 14];89:780–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17403800.
Wilson N, Broatch J, Jehn M, Davis C. National projections of time, cost and failure in implantable device identification: consideration of unique device identification use. Healthc (Amsterdam, Netherlands). 2015 [cited 2018 May 30];3:196–201. Available from: http://linkinghub.elsevier.com/retrieve/pii/S2213076415000408.
TraumaCad – Education. [cited 2021 Jul 9]. Available from: https://www.traumacad.com/#spine.
Real Intelligence | Smith & Nephew – US Professional. [cited 2021 Jul 9]. Available from: https://www.smith-nephew.com/professional/products/robotics/real-intelligence/.
P L. Deep convolutional neural networks for endotracheal tube position and X-ray image classification: challenges and opportunities. J Digit Imaging. J Digit Imaging; 2017 [cited 2021 Jul 9];30:460–8. Available from: https://pubmed.ncbi.nlm.nih.gov/28600640/.
Yi PH, Kim TK, Wei J, Shin J, Hui FK, Sair HI, et al. Automated semantic labeling of pediatric musculoskeletal radiographs using deep learning. Pediatr Radiol. 2019 [cited 2019 Dec 15];49:1066–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31041454.
CT C, TY H, TY L, CC C, CC C, CC C, et al. Application of a deep learning algorithm for detection and visualization of hip fractures on plain pelvic radiographs. Eur Radiol. Eur Radiol; 2019 [cited 2021 Jul 9];29:5469–77. Available from: https://pubmed.ncbi.nlm.nih.gov/30937588/.
RW F, SK F. Effectiveness of deep learning algorithms to determine laterality in radiographs. J Digit Imaging. J Digit Imaging; 2019 [cited 2021 Jul 9];32:656–64. Available from: https://pubmed.ncbi.nlm.nih.gov/31065828/.
Kitamura G. Hanging protocol optimization of lumbar spine radiographs with machine learning. Skeletal Radiol. Springer Science and Business Media Deutschland GmbH; 2021 [cited 2021 Mar 17]; Available from: https://pubmed.ncbi.nlm.nih.gov/33590305/.
Kitamura G. Deep learning evaluation of pelvic radiographs for position, hardware presence, and fracture detection. Eur J Radiol. Elsevier Ireland Ltd; 2020 [cited 2021 Mar 17];130. Available from: https://pubmed.ncbi.nlm.nih.gov/32623269/.
Yi PH, Wei J, Kim TK, Sair HI, Hui FK, Hager GD, et al. Automated detection & classification of knee arthroplasty using deep learning. Knee. 2019;27 [cited 2020 Jan 29]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31883760.
Yi PH, Kim TK, Wei J, Li X, Hager GD, Sair HI, et al. Automated detection and classification of shoulder arthroplasty models using deep learning. Skeletal Radiol. 2020; Available from: https://doi.org/10.1007/s00256-020-03463-3.
Bilbrey JA, Ramirez EF, Brandi-Lozano J, Sivaraman C, Short J, Lewis ID, et al. Improving radiograph analysis throughput through transfer learning and object detection. J Med Artif Intell. AME Publishing Company; 2020 [cited 2021 Mar 17];3:9–9. Available from: http://jmai.amegroups.com/article/view/5655/html.
IMPLANT ATLAS — Hip & Knee Book. [cited 2019 Dec 15]. Available from: https://hipandkneebook.com/hip-implants.
Branovacki G. Ortho Atlas – Hip Arthroplasty – U.S. Femoral Implants 1938–2008. Ortho Atlas Publishing, Inc.; 2008. Available from: https://www.orthoatlas.com/.
Levine BR, Springer BD, Golladay GJ. Highlights of the 2019 American Joint Replacement Registry Annual Report. Arthroplast Today. Elsevier Inc.; 2020 [cited 2021 Mar 17];6:998–1000. Available from: https://pubmed.ncbi.nlm.nih.gov/33385041/.
Patel R, Thong EHE, Batta V, Bharath AA, Francis D, Howard J. Automated identification of orthopedic implants in radiographs using deep learning. Radiol Artif Intell. Radiological Society of North America ; 2021 [cited 2021 Mar 17];e200183. Available from: http://pubs.rsna.org/doi/10.1148/ryai.2021200183.
Karnuta JM, Luu BC, Roth AL, Haeberle HS, Chen AF, Iorio R, et al. Artificial intelligence to identify arthroplasty implants from radiographs of the knee. J Arthroplasty. Churchill Livingstone Inc.; 2020 [cited 2021 Mar 17];36. Available from: https://pubmed.ncbi.nlm.nih.gov/33160805/.
Karnuta JM, Haeberle HS, Luu BC, Roth AL, Molloy RM, Nystrom LM, et al. Artificial intelligence to identify arthroplasty implants from radiographs of the hip. J Arthroplasty. Churchill Livingstone Inc.; 2020 [cited 2021 Mar 17]; Available from: https://pubmed.ncbi.nlm.nih.gov/33281020/.
Borjali A, Chen AF, Muratoglu OK, Morid MA, Varadarajan KM. Detecting total hip replacement prosthesis design on plain radiographs using deep convolutional neural network. J Orthop Res. John Wiley & Sons, Ltd; 2020 [cited 2020 Feb 4];38:jor.24617. Available from: https://arxiv.org/abs/1911.12387.
Borjali A, Chen AF, Bedair HS, Melnic CM, Muratoglu OK, Morid MA, et al. Comparing the performance of a deep convolutional neural network with orthopaedic surgeons on the identification of total hip prosthesis design from plain radiographs. Med Phys. Wiley; 2021 [cited 2021 Mar 17]; Available from: https://pubmed.ncbi.nlm.nih.gov/33411949/.
Murphy M, Killen C, Burnham R, Sarvari F, Wu K, Brown N. Artificial intelligence accurately identifies total hip arthroplasty implants: a tool for revision surgery. HIP Int. SAGE Publications Ltd; 2021 [cited 2021 Mar 17]; Available from: https://pubmed.ncbi.nlm.nih.gov/33412939/.
Yang H-S, Kim K-R, Kim S, Park J-Y. Deep learning application in spinal implant identification. Spine (Phila Pa 1976). Ovid Technologies (Wolters Kluwer Health); 2021 [cited 2021 Mar 17];46:E318–24. Available from: https://pubmed.ncbi.nlm.nih.gov/33534442/.
Huang KT, Silva MA, See AP, Wu KC, Gallerani T, Zaidi HA, et al. A computer vision approach to identifying the manufacturer and model of anterior cervical spinal hardware. J Neurosurg Spine. 2019 [cited 2019 Dec 15];1–7. Available from: https://thejns.org/view/journals/j-neurosurg-spine/aop/article-10.3171-2019.6.SPINE19463.xml.
Rouzrokh P, Wyles CC, Philbrick KA, Ramazanian T, Weston AD, Cai JC, et al. A deep learning tool for automated radiographic measurement of acetabular component inclination and version after total hip arthroplasty. J Arthroplasty. Elsevier B.V.; 2021 [cited 2021 Mar 17]; Available from: https://pubmed.ncbi.nlm.nih.gov/33678445/.
Cho BH, Kaji D, Cheung ZB, Ye IB, Tang R, Ahn A, et al. Automated measurement of lumbar lordosis on radiographs using machine learning and computer vision. Glob spine J. SAGE Publications Ltd; 2020 [cited 2021 Mar 17];10:611–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32677567.
Zheng Q, Shellikeri S, Huang H, Hwang M, Sze RW. Deep learning measurement of leg length discrepancy in children based on radiographs. Radiology. Radiological Society of North America Inc.; 2020 [cited 2021 Mar 17];296:152–8. Available from: https://pubmed.ncbi.nlm.nih.gov/32315267/.
Radlink Surgical System - Radlink, Inc.. [cited 2021 Jul 9]. Available from: https://radlink.com/radlink-surgical-system/.
Shah RF, Bini SA, Martinez AM, Pedoia V, Vail TP. Incremental inputs improve the automated detection of implant loosening using machine-learning algorithms. Bone Jt J. British Editorial Society of Bone and Joint Surgery; 2020 [cited 2021 Mar 17];102-B:101–6. Available from: https://pubmed.ncbi.nlm.nih.gov/32475275/.
Rouzrokh P, Ramazanian T, Wyles CC, Philbrick KA, Cai JC, Taunton MJ, et al. Deep learning artificial intelligence model for assessment of hip dislocation risk following primary total hip arthroplasty from postoperative radiographs. J Arthroplasty. Elsevier B.V.; 2021 [cited 2021 Mar 17]; Available from: https://pubmed.ncbi.nlm.nih.gov/33663890/.
Gwam CU, Mistry JB, Mohamed NS, Thomas M, Bigart KC, Mont MA, et al. Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty. 2017 [cited 2018 Oct 2];32:2088–92. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28336249.
Delanois RE, Mistry JB, Gwam CU, Mohamed NS, Choksi US, Mont MA. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017 [cited 2018 Oct 2];32:2663–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28456561.
Shah RP, Plummer DR, Moric M, Sporer SM, Levine BR, Della Valle CJ. Diagnosing infection in the setting of periprosthetic fractures. J Arthroplasty. 2016 [cited 2020 Jan 15];31:140–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27067465.
Yi PH, Cross MB, Moric M, Sporer SM, Berger RA, Della Valle CJ. The 2013 Frank Stinchfield award: diagnosis of infection in the early postoperative period after total hip arthroplasty. Clin Orthop Relat Res. 2014;472:424–9 [cited 2015 Feb 18]. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3890203&tool=pmcentrez&rendertype=abstract.
Yi PH, Cross MB, Moric M, Levine BR, Sporer SM, Paprosky WG, et al. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res. 2015;473:498–505 [cited 2018 Jan 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25171935.
Shohat N, Bauer T, Buttaro M, Budhiparama N, Cashman J, Della Valle CJ, et al. Hip and knee section, what is the definition of a periprosthetic joint infection (PJI) of the knee and the hip? Can the same criteria be used for both joints?: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty. 2019 [cited 2019 Feb 18];34:S325–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30343971.
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, et al. The 2018 Definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018 [cited 2019 Feb 18];33:1309–1314.e2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29551303.
Tibbo ME, Wyles CC, Fu S, Sohn S, Lewallen DG, Berry DJ, et al. Use of natural language processing tools to identify and classify periprosthetic femur fractures. Churchill Livingstone Inc.; 2019 [cited 2020 Jan 15];34:2216–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31416741.
Wyles CC, Tibbo ME, Fu S, Wang Y, Sohn S, Kremers WK, et al. Use of natural language processing algorithms to identify common data elements in operative notes for total hip arthroplasty. J Bone Jt Surg - Am Vol. Lippincott Williams and Wilkins; 2019 [cited 2021 Mar 17];101:1931–8. Available from: https://pubmed.ncbi.nlm.nih.gov/31567670/.
Fu S, Wyles CC, Osmon DR, Carvour ML, Sagheb E, Ramazanian T, et al. Automated detection of periprosthetic joint infections and data elements using natural language processing. J Arthroplasty. Churchill Livingstone Inc.; 2021 [cited 2021 Mar 17];36:688–92. Available from: https://pubmed.ncbi.nlm.nih.gov/32854996/.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Statement
Artificial intelligence has tremendous potential to automate the radiological evaluation of orthopedic implants, thereby augmenting the musculoskeletal radiologist in daily practice.
Most Important Concepts
• Artificial intelligence (AI) and deep learning can automate radiologic tasks, such as identification of specific implant models, with high accuracies and speeds.
• AI can also be used to extract clinical information from text data, such as clinical notes, to aid in tasks like prepopulating radiology reports with clinical information.
• Although several papers have been published on the use of AI for implant evaluation, these are still proof-of-concept works that need clinical validation.
Rights and permissions
About this article
Cite this article
Yi, P.H., Mutasa, S. & Fritz, J. AI MSK clinical applications: orthopedic implants. Skeletal Radiol 51, 305–313 (2022). https://doi.org/10.1007/s00256-021-03879-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03879-5