Abstract
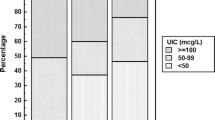
The aim of the present study is to evaluate the relationships between urinary iodine concentration (UIC) and the intake of milk and other foods, in a group of school children of the Veneto region, in North East Italy. A questionnaire, concerning the daily intake of milk, yoghurt, cheese and other animal foodstuffs, was distributed to 233 schoolchildren aged between 11 and 15 yr. The use of iodized salt was also investigated. UIC was measured in a casual urine sample of all children investigated. The iodine content of 28 samples of milk and of 13 samples of yoghurt, bought during the summer in shops of the same area, was measured. UIC values ranged between 25 and 436 μg/l, median value was 140 μg/l, mean value 149±78 μg/l. The median iodine content of milk and yoghurt were 278 μg/l and 216 μg/l, respectively. With regard to dietary habits, about 70% of the children took 200 ml of milk or more per day, which corresponds to a daily intake of iodine ranging between 50 and 100 μg a day. About 30% of schoolchildren used iodized salt. A highly significant correlation between UIC and milk intake was observed (p=0.0005), while the relationship was poor or absent in the case of both intake of other foodstuffs and use of iodized salt (p=0.38). In conclusion, the results of the study document the very important role of cows’ milk as a source of iodine in childhood in the Veneto region, Italy.
Similar content being viewed by others
References
Delange F, Dunn T, Glinoer D. Iodine deficiency in Europe. A continuing concern. New York: Plenum Press. 1993.
Lee SM, Lewis J, Buss DH, et al. Iodine in British foods and diets. Br J Nutr 1994, 72: 435–46.
WHO, UNICEF, ICCIDD. Indicators for assessing iodine deficiency disorders and their control through salt iodization. WHO/NUT/94.6. Geneva: WHO 1994.
Delange F, Van Onderbergen A, Shabana W, et al. Silent iodine prophylaxis in Western Europe only partly corrects iodine deficiency; the case of Belgium. Eur J Endocrinol 2000, 143: 189–96.
Szybinski Z, Delange F, Lewinski A, et al. A programme of iodine supplementation using only iodised household salt is efficientthe case of Poland. Eur J Endocrinol 2001, 144: 331–7.
Wiersinga WM, Pdoba J, Srbecky M, et al. A survey of iodine intake and thyroid volume in Dutch schoolchildren: reference values in an iodine-sufficient area and the effect of puberty. Eur J Endocrinol 2001, 144: 595–603.
Lamberg BA. Endemic goiter in Finland and changes during 30 years of iodine prophylaxis. Endocrinol Exp 1986, 20: 35–47.
Phillips DIW. Iodine, milk and the elimination of endemic goitre in Britain: the story of an accidental public health triumph. J Epidemiol Community Health 1997, 51: 391–3.
Rasmussen LB, Larsen EH, Ovesen L. Iodine content in drinking water and other beverages in Denmark. Eur J Clin Nutr 2000, 54: 57–60.
Busnardo B, Nacamulli D, Frigato, et al. Normal values for thyroid ultrasonography, goitre prevalence, and urinary iodine concentration in schoolchildren of the Veneto Region, Italy. J Endocrinol Invest 2003, 26: 991–6.
International Council for Control of Iodine Deficiency Disorders, United Nations Children’s Fund, World Health Organization. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. 2nd ed.: Geneva: World Health Organization; Unpublished document WHO/NHD/01.1. 2001.
WHO, UNICEF, ICCIDD. Recommended iodine levels in salt and guidelines for monitoring their adequacy and effectiveness. WHO/NUT/96.13. Geneva: WHO 1996.
Vilkki P. Iodine in the Finish diet and its relation to goitre incidence. Ann Acad Sci Fenn Ser A II Chem 1956, 71.
Varo P, Saari E, Paaso A, et al. Iodine in Finish foods. Int J Vitam Nutr Res 1982, 52: 80–9.
Lamberg BA. Iodine deficiency disorders and endemic goitre. Eur J Clin Nutr 1993, 47: 1–8.
Nelson M, Philips DIW. Seasonal variations in dietary iodine intake and thyrotoxicosis. Hum Nutr Appl Nutr 1985, 39A: 213–6.
Nelson M, Philips DI, Morris JA, et al. Urinary iodine excretion correlates with milk iodine content in seven British towns. J Epidemiol Community Health 1987, 42: 72–5.
Larsen SH, Knuthsen P, Hansen M. Seasonal and regional variations of iodine in Danish dairy products determined by inductively coupled plasma mass spectrometry. JAAS 1999, 14: 41–4.
Rasmussen LB, Ovesen L, Bulow I, et al. Dietary iodine intake and urinary iodine excretion in a Danish population: effect of geography, supplements and food choice. Br J Nutr 2002, 87: 61–9.
Als C, Helbling A, Peter K et al. Urinary iodine concentration follows a circadian rhythm: a study with 3023 spot urine samples in adults and children. J Clin Endocrinol Metab 2000, 85: 1367–9.
Als C, Haldimann M, Burgi E, et al. Swiss pilot of individual season fluctuations of urinary iodine concentration over two years: in age-dependency linked to the major source of dietary iodine? Eur J Clin Nutr 2003, 57: 636–46.
NCR. National Research Council. Nutrient requirements of dairy cattle. Sixth Revised Edition. Washington: National Academy Press. 1989, 32–3.
Underwood EJ, Suttle NF. The mineral nutrition of livestock. 3rd ed. New York: CABI Publishing. 1999, 343–73.
Underwood EJ. Trace elements in human and animal nutrition. London: Academic Press. 1977, 271-91.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Girelli, M.E., Coin, P., Mian, C. et al. Milk represents an important source of iodine in schoolchildren of the Veneto region, Italy. J Endocrinol Invest 27, 709–713 (2004). https://doi.org/10.1007/BF03347510
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03347510