Abstract
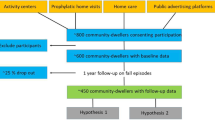
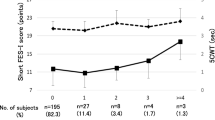
Background and aims: Identification of the risk of falls in a cohort of interest is a prerequisite for a targeted fall prevention study. Motor tasks are widely used as baseline assessment in such studies, but there are only a few well-evaluated tests of motor performance to predict falls prospectively. This study was conducted to find out if the potential of the maximum step length (MSL) test can predict future falls in non-disabled older persons. Methods: A modified version of the MSL test was used for baseline assessment in 56 community-dwelling, non-disabled elderly persons (mean age 67.7 yrs, SD 6 yrs; 57% women). During a follow-up of 1 year, falls were recorded in a daily calendar. Results: During the follow-up, 30 persons (54%) fell, with no gender difference in reporting of falls between men and women. The adjusted mean valid step length and adjusted maximum valid step length were predictive of future falls with a sensitivity/specificity of 77%/62% and 70%/69%, respectively. Combining MSL test results with fall history increased sensitivity to 93% and 90%, respectively, but decreased specificity to 54% and 58%, respectively. Conclusions: The MSL test is a feasible tool, with low requirements in space, predicting future falls in community-dwelling older persons. In combination with history of falls, the sensitivity of the test increased considerably.
Similar content being viewed by others
References
Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA 2007; 297: 77–86.
National Institute for Clinical Excellence (NICE). Clinical practice guideline for the assessment and prevention of falls in older people. 2004 [cited]; Available from: http://www.nice.org.uk/page.aspx?o=CG021
Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing 2004; 33: 122–30
Wyatt JC, Altman D. Prognostic models: clinically useful or quickly forgotten? BMJ 1995; 311: 1539–41.
Guideline for the Prevention of Falls in Older Persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc 2001; 49: 664–72.
Chiu AY, Au-Yeung SS, Lo SK. A comparison of four functional tests in discriminating fallers from non-fallers in older people. Disabil Rehabil 2003; 25: 45–50.
Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002; 83: 1566–71.
Rose D, Jones C, Lucchese N. Predicting the probability of falls in community-residing older adults using the 8-foot Up-and-Go: a new measure of functional mobility. J Aging Phys Act 2002; 10: 466–76.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000; 80: 896–903.
Okumiya K, Matsubayashi K, Nakamura T, et al. The timed “up & go” test is a useful predictor of falls in community-dwelling older people [letter; comment]. J Am Geriatr Soc 1998; 46: 928–30.
Lin MR, Hwang HF, Hu MH, Wu HD, Wang YW, Huang FC. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc 2004; 52: 1343–8.
Raiche M, Hebert R, Prince F, Corriveau H. Screening older adults at risk of falling with the Tinetti balance scale. Lancet 2000; 356: 1001–2.
Topper AK, Maki BE, Holliday PJ. Are activity-based assessments of balance and gait in the elderly predictive of risk of falling and/or type of fall? J Am Geriatr Soc 1993; 41: 479–87.
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc 1997; 45: 735–8.
Bogl-Thorbahn L, Newton R. Use of the Berg Balance Test to predict falls in elderly persons. Phys Ther 1996; 76: 576–85.
Horak FB, Nashner LM, Diener HC. Postural strategies associated with somatosensory and vestibular loss. Exp Brain Res 1990; 82: 167–77.
Medell JL, Alexander N. A clinical measure of maximal and rapid stepping in older women. J Gerontol 2000; 55A: M429–33.
Lindemann U, Bäurle C, Muche R, Nikolaus Th, Becker C. Age-related differences in balance, strength and motor function. Eur J Ger 2003; 5: 15–22.
Cho B, Scarpace D, Alexander NB. Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adults. J Am Geriatr Soc 2004; 52: 1168–73.
Kessler J, Calabrese P, Kalbe E, Berger F. Ein neues Screening Verfahren zur Unterstützung der Demenzdiagnostik. Psycho 2000; 26: 343–7.
Holbrook M, Skilbeck CE. An activities index for use in stroke patients. Age Ageing 1983; 12: 166–70.
Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc 2005; 53: 1618–26.
Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ 2004; 329: 168–9.
Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing 2007; 36: 130–9.
Gulich M, Zeitler HP. [The walking-counting test. A simple test for assessing the risk of falling]. Dtsch Med Wochenschr 2000; 125: 245–8.
Streiner DL. Diagnosing tests: using and misusing diagnostic and screening tests. J Pers Assess 2003; 81: 209–19.
Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. atInterventions for preventing falls in elderly people. Cochrane Database Syst Rev 2003: CD000340.
Bergland A, Jarnlo GB, Laake K. Predictors of falls in the elderly by location. Aging Clin Exp Res 2003; 15: 43–50.
Hill K, Schwarz J, Flicker L, Carroll S. Falls among healthy, community-dwelling, older women: a prospective study of frequency, circumstances, consequences and prediction accuracy. Aust NZ J Public Health 1999; 23: 41–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindemann, U., Lundin-Olsson, L., Hauer, K. et al. Maximum step length as a potential screening tool for falls in non-disabled older adults living in the community. Aging Clin Exp Res 20, 394–399 (2008). https://doi.org/10.1007/BF03325143
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03325143