Abstract
Background: While drotrecogin alfa (activated) was shown to decrease absolute 28-day mortality by 6.1% in patients with severe sepsis in the Recombinant Human Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study, no mortality benefit was observed in the subset of patients with only one organ system failure. Consequently, some institutions restrict drotrecogin alfa (activated) use to patients with severe sepsis with ≥ organ system failures.
Objective: To measure the cost effectiveness of drotrecogin alfa (activated) for treatment of severe sepsis in relation to the number of organ system failures and determine the economic impact of restricting drotrecogin alfa (activated) use based on the number of organ system failures.
Perspective: Policy perspective specific to our 340-bed, level I trauma centre.
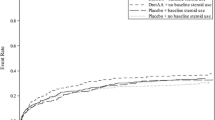
Methods: A Monte Carlo simulation analysis was conducted to evaluate a hypothetical cohort of 10 000 patients with severe sepsis in four scenarios restricting treatment with drotrecogin alfa (activated) to patients with ≥1, ≥2, ≥3 or ≥4 organ system failures. The primary outcomes of 28-day all-cause mortality and serious bleeding were obtained from the PROWESS study. Costs (year 2002 values) were obtained from institutional financial records and literature estimates. The incremental cost per life saved at 28 days with drotrecogin alfa (activated) plus best standard care versus best standard care alone (placebo) was calculated. The incidence of severe sepsis and number of drotrecogin alfa (activated) candidates were estimated through chart review, and projected annual institutional expenditures were derived according to these data.
Results: With increasing number of organ system failures, the proportion of lives saved with drotrecogin alfa (activated) increased, and consequently the ICER decreased. Restriction of drotrecogin alfa (activated) to patients with ≥4 organ system failures was the most cost-effective scenario (0.11 lives saved; $US56 727 per life saved). For the nine patients that would be treated annually by our institution under this policy, one life would be saved at a total additional cost of $US56 160 per year. Use of the drug in patients with ≥1 or ≥2 organ system failures would save the greatest number of lives per year (4–5); however, restricting drotrecogin alfa (activated) to patients with ≥ organ system failures would be the cheaper alternative (total additional cost $US356 022 vs $US462 204).
Conclusion: While restriction of drotrecogin alfa (activated) use to patients with sepsis with ≥4 organ system failures is the most cost-effective alternative, restriction to those with ≥2 organ system failures is the preferred alternative for our institution according to the number of lives saved and available financial resources.






Similar content being viewed by others
References
Sands KE, Bates DW, Lanken PN, et al. Epidemiology of sepsis syndrome in 8 academic medical centers; academic medical center consortium sepsis project working group. JAMA 1997; 278: 234–40
Angus DC, Wax RS. Epidemiology of sepsis: an update. Crit Care Med 2001; 29: S109–19
Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29 (7): 1303–10
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis: The ACCP/SCCM Consensus Conference Committee: American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101: 1644–55
Rangel-Frausto MS, Pittet D, Costigan M, et al. The natural history of the systemic inflammatory response syndrome (SIRS): a prospective study. JAMA 1995; 237: 117–23
Balk RA. Pathogenesis and management of multiple organ dysfunction or failure in severe sepsis and septic shock. Crit Care Clin 2000; 16: 337–52
Grinnell BW, Joyce D. Recombinant human activated protein C: a system modulator of vascular function for treatment of severe sepsis. Crit Care Med 2001; 29: S53–61
Esmon C. The protein C pathway. Crit Care Med 2000; 28 (9): S44–8
Yan SB, Dhainaut J. Activated protein C versus protein C in severe sepsis. Crit Care Med 2001; 29: S69–74
Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001; 344: 699–709
Xigris: drotrecogin alfa (activated): PV3420 AMP. Rockville (MD): Food and Drug Administration, 2001
Roberts KA. Best practices in the development of clinical practice guidelines. J Healthc Qual 1998; 20: 16–20
Vanscoy G, Devlin JW, Ponzillo J, et al. Implementing guidelines for drotrecogin alfa (activated): three perspectives. Pharmacy Ther 2002; 27: 1–15
Oxman AD, Guyatt GH. A consumer’s guide to subgroup analysis. Ann Intern Med 1992; 116: 78–84
Bootman JL, Harrison DL. Pharmacoeconomics and therapeutic drug monitoring. Pharm World Sci 1997; 19: 178–81
Grabowski H. The effect of pharmacoeconomics on company research and development decisions. Pharmacoeconomics 1997; 11 (5): 389–97
Schulman KA, Linas BP. Pharmacoeconomics: state of the art in 1997. Annu Rev Public Health 1997; 18: 529–48
Revicki DA, Luce BR. Methods of pharmacoeconomic evaluation of new medical treatments in psychiatry. Psychopharmacol Bull 1995; 31: 57–65
Angus DC, Linde-Zwirble WT, Clermont G, et al. Cost effectiveness of drotrecogin alfa (activated) (Xigris) in severe sepsis [abstract]. Crit Care Med 2001; 30 (2): 493
Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification. Crit Care Med 1985; 13: 818–29
Manus BJ, Lee H, Doig CJ, et al. An economic evaluation of activated protein C treatment for severe sepsis. N Engl J Med 2002; 347: 993–1000
Crystal Ball 2000 [computer program]. Denver (CO): Decisioneering, Inc., 2000
DATA 3.5 [computer program]. Williamstown (MA): TreeAge Software, Inc, 2001
Munoz E, Margolis IB, Wise L. Surgonomics: the cost of gastrointestinal hemorrhage, the identifier concept. Am J Gastroenterol 1985 Feb; 80: 139–42
Doubilet P, Begg CB, Weinstein MC, et al. Probabilistic sensitivity analysis using Monte Carlo simulation: a practical approach. Med Decis Making 1985 Summer; 5: 157–77
Doubilet P, McNeil BJ. Clinical decisionmaking. Med Care 1985; 23: 648–62
Kuzma JW. Basic statistics for the health sciences. 3rd ed. California: Mayfield Publishing Company, 1998
Kanji S, Betancourt M, Kruse JA, et al. Validating the use of an ICD-9 based search strategy to identify patients with severe sepsis who may be candidates for drotrecogin alfa (activated) therapy [abstract]. Pharmacotherapy 2002; 22: 407
Szucs TD, Mantovani LG. The perspective of a pharmacoeconomic study: targeting for audiences. Pharmacol Res 1997; 35: 471–5
Massel D. Potential cost effectiveness of tissue plasminogen activator among patients previously treated with streptokinase. Can J Cardiol 1999; 15: 173–9
Russell MW, Huse DM, Miller JD, et al. Cost effectiveness of HMG-CoA reductase inhibition in Canada. Can J Clin Pharmacol 2001; 8: 9–16
Detsky AS, Naglie IG. A clinician’s guide to cost-effectiveness analysis. Ann Intern Med 1990 Jul 15; 113 (2): 147–54
McIntosh E, Donaldson C, Ryan M. Recent advances in the methods of cost-benefit analysis in healthcare: matching the art to the science. Pharmacoeconomics 1999; 15 (4): 357–67
Johannesson M. At what coronary risk level is it cost-effective to initiate cholesterol lowering drug treatment in primary prevention? Fur Heart J 2001 Jun; 22: 919–25
Angus DC, Laterre PF, Helterbrand J, et al. The effects of drotrecogin alfa (activated) on long-term survival after severe sepsis [abstract]. Chest 2002; 122 (4 Suppl.): 51S
Angus DC, Vincent JL, Artigas A, et al. The effect of recombinant human activated protein C (rhAPC) on organ dysfunction and functional recovery in severe sepsis [abstract]. Crit Care Med 2000; 28 Suppl.: A48
Baltussen R, Leidl R, Ament A. Real world designs in economic evaluation: bridging the gap between clinical research and policy-making. Pharmacoeconomics 1999 Nov; 16 (5 Pt 1): 449–58
Sanchez LA. Applied pharmacoeconomics: evaluation and use of pharmacoeconomic data from the literature. Am J Health Syst Pharm 1999; 56: 1630–8
Acknowledgements
The authors have no conflicts of interest directly relevant to the content of this study and no funding from pharmaceutical companies was used in completing the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Betancourt, M., McKinnon, P.S., Massanari, R.M. et al. An evaluation of the cost effectiveness of drotrecogin alfa (activated) relative to the number of organ system failures. Pharmacoeconomic 21, 1331–1340 (2003). https://doi.org/10.1007/BF03262331
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03262331