Abstract
Background
Exenatide (Byetta®) and insulin glargine (Lantus®) are antidiabetic agents that are typically used after lack of response to an oral antidiabetic agent(s). Although previous research has examined the impact of these medications on glycaemic control, there is little information about the relative costs associated with the medications.
Objective
To compare costs among patients with type 2 diabetes mellitus treated with exenatide or insulin glargine from a US third-party payer perspective.
Methods
Data from a large, national administrative claims database were used in this study. The intent-to-treat (ITT) cohort included adults who were diagnosed with type 2 diabetes and initiated therapy with either exenatide (n = 4090) or insulin glargine (n = 1660). In addition, included patients were required to have no diagnoses of type 1 diabetes, to have received at least two prescriptions for an oral antidiabetic agent in the 6 months prior to first use of either exenatide or insulin glargine and to have continuous insurance coverage from 6 months before, to 12 months after, initiation on ITT medication.
Annual total medical costs and total diabetes-related medical costs, in $US, year 2007 values, were estimated using stepwise multivariate regressions. Major cost components were also examined using either stepwise multivariate regressions or a two-part model that controlled for the probability of using the service. Smearing estimates were used to transform estimated log costs into costs. The analysis controlled for the potential impact of patient demographics, general health, prior resource use, co-morbidities and complications, and timing of treatment initiation.
Results
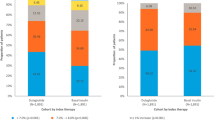
Compared with insulin glargine, initiation of exenatide was associated with significantly lower total direct medical costs ($US19 293 vs $US23 782; p < 0.0001), inpatient costs ($US4121 vs $US7532; p < 0.0001), outpatient costs ($US9501 vs $US12 885; p < 0.0001), emergency department (ED) costs ($US82 vs $US131; p < 0.0001), total diabetes-related medical costs ($US7833 vs $US8536; p < 0.0001), diabetes-related inpatient costs ($US2172 vs $US3538; p <0.0001) and diabetes-related outpatient costs ($US2739 vs $US3249; p < 0.0001). Initiation of exenatide was associated with significantly higher total overall drug costs ($US6885 vs $US5936; p < 0.0001) and diabetes-related drug costs ($US3160 vs $US2422; p < 0.0001).
Conclusions
Compared with the use of insulin glargine, use of exenatide was associated with significantly lower annual total direct medical costs and significantly lower total diabetes-related medical costs, despite higher total drug costs and higher diabetes-related drug costs. In addition, exenatide was associated with significantly lower total inpatient, outpatient, ED, and diabetes-related inpatient and outpatient costs.



Similar content being viewed by others
References
American Diabetes Association. Economic costs of diabetes in the US in 2007 [published erratum appears in Diabetes Care 2008; 31 (6): 1271]. Diabetes Care 2008; 31: 596–615
American Diabetes Association. Standards of medical care in diabetes: 2008. Diabetes Care 2008; 31Suppl. 1: S12–54
Edwards KL, Alvarez C, Irons BK, et al. Third-line agent selection for patients with type 2 diabetes mellitus uncontrolled with sulfonylureas and metformin. Pharma-cotherapy 2008; 28(4): 506–21
Gerich JE. Insulin glargine: long acting basal insulin analog for improved metabolic control. Curr Med Res Opin 2004; 20: 31–7
BNET. Aventis Pharmaceuticals’ LANTUS® (insulin glargine [rDNA origin] injection) approved by FDA for treatment of diabetes. Market Wire [online]. Available from URL: http://findarticles.com/p/articles/mi_pwwi/is_200004/ai_ mark09008855 [Accessed 2008 Sep 23]
US Food and Drug Administration. CDER drug and biologic approvals for calendar year 2005 [online]. Available from URL: http://www.fda.gov/cder/rdmt/InternetNDA 05.htm [Accessed 2008 Sep 23]
Barclay L. Exenatide approved for type 2 diabetes: an expert interview with John B. Buse. Medscape Today [online]. Available fromURL: http://www.medscape.com/viewarticle/504227 [Accessed 2008 Sep 23]
Nielsen LL, Okerson T, Holcombe J, et al. Effects of ex-enatide on diabetes, obesity, cardiovascular risk factors, and hepatic biomarkers in patients with type 2 diabetes. J Diab Sci Tech 2008; 2: 255–60
Stonehouse AH, Maggs DG. Emerging therapies for type 2 diabetes. Curr Drug Ther 2007; 2: 151–60
Degn KB, Brock B, Juhl CB, et al. Effect of intravenous infusion of exenatide (synthetic exendin-4) on glucose-dependent insulin secretion and counterregulation during hypoglycemia. Diabetes 2004; 53: 2397–403
Nauck MA, Heimesaat MM, Behle K, et al. Effects of glu-cagon-like peptide 1 on counterregulatory hormone responses, cognitive functions, and insulin secretion during hyperinsulinemic, stepped hypoglycemic clamp experiments in healthy volunteers. J Clin Endocrinol Metab 2002; 87: 1239–46
Cvetkovic RS, Plosker GL. Exenatide: a review of its use in patients with type 2 diabetes mellitus (as an adjunct to metformin and/or a sulfonylurea). Drugs 2007; 67: 935–54
Kolterman OG, Kim DD, Shen L, et al. Pharmacokinetics, pharmacodynamics, and safety of exenatide in patients with type 2 diabetes mellitus. Am J Health Syst Pharm 2005; 62: 173–81
Heine RJ, Van Gaal LF, Johns D, et al. Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes. Annals Int Med 2005; 143: 559–69
Barnett AH, Burger J, Johns D, et al. Tolerability and efficacy of exenatide and titrated insulin glargine in adult patients with type 2 diabetes previously uncontrolled with metformin or a sulfonylurea: a multinational, randomized, open-label, two-period, crossover noninferiority trial. Clin Ther 2007; 29: 2333–48
Yu AP, Wu EQ, Birnbaum HG, et al. Short-term economic impact of body weight change among patients with type 2 diabetes treated with antidiabetic agents: analysis using claims, laboratory, and medical record data. Curr Med Res Opin 2007; 23(9): 2157–69
Bray GA, Bellanger T. Epidemiology, trends, and morbidities of obesity and the metabolic syndrome. Endocrine 2006; 29: 109–17
Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003; 289: 76–9
Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin North Am 2003; 32: 805–22
Williamson DF, Thompson TJ, Thun M, et al. Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care 2000; 23: 1499–504
Heine RJ, Van Gaal LF, Johns D, et al. Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med 2005; 143(8): 559–69
Miller DR, Gardner JA, Hendricks AM, et al. Health care resource utilization and expenditures associated with the use of insulin glargine. Clin Ther 2007; 29(3): 478–87
Warren E, Weatherley-Jones E, Chilcott J, et al. Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine. Health Technol Assess 2004 Nov; 8(45): 1–57
Suntsov YI, Dedov II, Komarova VP, et al. Pharmacoeco-nomic aspects of use of insulin glargine in treatment of diabetes mellitus type 2 (dm t2) in Russia [abstract]. Value Health 2004; 7: 738
Goodall G, Jendle JH, Valentine WJ, et al. Biphasic insulin aspart 70/30 vs insulin glargine in insulin naïve type 2 diabetes patients: modelling the long-term health economic implications in a Swedish setting. Int J Clin Pract 2008 Jun; 62(6): 869–76
Janka HU, Hügy B. Economic evaluation of the treatment of type 2 diabetes with insulin glargine based on the LAPTOP trial. Eur J Health Econ 2008 May; 9(2): 165–70
Leichter S. Is the use of insulin analogues cost-effective? Adv Ther 2008 Jul-Aug; 25(4): 285–99
Ray JA, Valentine WJ, Roze S, et al. Insulin therapy in type 2 diabetes patients failing oral agents: cost-effectiveness of biphasic insulin aspart 70/30 vs insulin glargine in the US. Diabetes Obes Metab 2007 Jan; 9(1): 103–13
Lechleitner M, Roden M, Haehling E, et al. Insulin glargine in combination with oral antidiabetic drugs as a cost- equivalent alternative to conventional insulin therapy in type 2 diabetes mellitus. Wien Klin Wochenschr 2005 Sep; 117(17): 593–8
Valentine WJ, Palmer AJ, Lammert M, et al. Long-term clinical and cost outcomes of treatment with biphasic insulin aspart 30/70 versus insulin glargine in insulin naïve type 2 diabetes patients: cost-effectiveness analysis in the UK setting. Curr Med Res Opin 2005 Dec; 21(12): 2063–71
Wu EQ, Birnbaum HG, Zhang HF, et al. Health care costs of adults treated for attention-deficit/hyperactivity disorder who received alternative drug therapies. J Manag Care Pharm 2007; 13: 561–9
Pelletier EM, Smith PJ, Boye KS, et al. Direct medical costs for type 2 diabetes mellitus complications in the US commercial payer setting: a resource for economic research. Appl Health Econ Health Policy 2008; 6(2-3); 103–12
Finkelstein EA, Bray JW, Chen H, et al. Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes Care 2003; 26: 415–20
D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: the Charlson comorbidity index. Meth-ods Inf Med 1993; 32: 382–7
Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc 1983; 78(383): 605–10
Diehr P, Yanez D, Ash A, et al. Methods for analyzing health care utilization and costs. Annu Rev Public Health 1999; 20: 125–44
Duan N, Manning WG, Morris CN, et al. A comparison of alternative models for the demand for medical care. J Bus Econ Stat 1983; 1: 115–26
Ray JA, Boye KS, Yurgin N, et al. Exenatide versus insulin glargine in patients with type 2 diabetes in the UK: a model of long-term clinical and cost outcomes. Curr Med Res Opin 2007 Mar; 23(3): 609–22
Oglesby AK, Secnik K, Barron J, et al. The association between diabetes related medical costs and glycemic control: a retrospective analysis. Cost Eff Resour Alloc 2006; 4: 1
Shetty S, Secnik K, Oglesby AK. Relationship of glycemic control to total diabetes-related costs for managed care health plan members with type 2 diabetes. J Manag Care Pharm 2005; 11(7): 559–64
Ayanian JZ, Hauptman PJ, Guadagnoli E, et al. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med 1994 Oct 27; 331(17): 1136–42
i3. Data assets: better data matters [online]. Available from URL: http://www.i3global.com/DataAssets/ [Accessed 2008 Sep 23]
Acknowledgements
Funding for this study was provided by Eli Lilly and Company.
Eli Lilly and Company provided funding for conducting the study to HealthMetrics Outcomes Research, of which Maureen J. Lage is an employee. Derek Misurski and Kristina S. Boye are employees and shareholders of Eli Lilly and Company, and were compensated for work on this project. Rosalind Fabunmi was an employee of Amylin Pharmaceuticals at the time this work was carried out and has stock options with Amylin Pharmaceuticals. Employees of Lilly and Amylin reviewed the manuscript prior to submission for publication.
The authors gratefully acknowledge the assistance of Patricia Platt in help with drafting the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Misurski, D., Lage, M.J., Fabunmi, R. et al. A comparison of costs among patients with type 2 diabetes mellitus who initiated therapy with exenatide or insulin glargine. Appl Health Econ Health Policy 7, 245–254 (2009). https://doi.org/10.1007/BF03256158
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256158