Abstract
Background and objective
Pulmonary arterial hypertension (PAH) is a rare but life-threatening condition that is characterized by progressive elevation of pulmonary artery pressure and pulmonary vascular resistance, leading to right-sided heart failure and frequently death. Orally administered agents used for the treatment of symptomatic, moderate-to-severe PAH include sildenafil and the endothelin (ET) receptor antagonists (ERAs), bosentan and sitaxentan (sitaxsentan). Ambrisentan is a new oral ETA receptor-selective ERA, with higher ET receptor affinity than bosentan. Placebo-controlled, randomized clinical trials (RCTs) have demonstrated that ambrisentan (5 or 10mg/day) is safe and effective. To provide health economic data on the multiple oral PAH therapies currently available, a population-based cost-minimization analysis (CMA) was conducted for Canada.
Methods
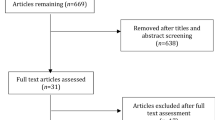
The primary requirement for a CMA is that all clinical outcomes be equivalent between comparator treatments. To provide such supporting data, a literature search was conducted for RCTs of oral agents used to treat symptomatic PAH. This was followed by application of direct and indirect statistical methods to support the hypothesis of clinical equivalence between the oral agents. Estimates for PAH prevalence, incidence and death rates were then used to build a population-based CMA model. The base-case analysis considered costs for drug therapy, outpatient pharmacy costs, medical consultations and visits, laboratory and diagnostic procedures and other healthcare-related resources. In addition, costs for secondary pharmacotherapy in cases where the primary agent had to be discontinued because of adverse effects were also included. The time horizon for evaluating pharmacotherapy was 3 years, all costs were in 2008 Canadian dollars ($Can) and the costs were discounted at a rate of 3% annually. The study perspective was the Canadian healthcare system.
Results
There were no double-blind RCTs comparing ambrisentan with any of the other oral agents. Therefore, an indirect comparison of placebo-controlled trials of PAH drugs had to be used to support the clinical equivalence. This included a calculation of standardized mean differences (SMD) between agents (vs placebo) and a meta-regression analysis on the primary and secondary trial endpoints. Keeping in mind the caveats associated with indirect trial comparisons, the data suggested similar clinical efficacy over 12–16 weeks between agents, as indicated by the identical magnitude of the SMD between the active agent and placebo and the non-significant differences between drugs as determined by the meta-regression analysis. The population-based model projected that the number of PAH patients clinically suitable for these drugs in Canada would be 931 in the first full-budget year (i.e. 2009) with an increase to 1114 by the third full year. The CMA revealed the following rank order of the least to most costly agent; sildenafil, ambrisentan, sitaxentan and bosentan. Sildenafil was the least costly, primarily because of the lower daily drug-acquisition cost. Of the three ERAs, ambrisentan would be associated with annual cost savings of $Can3.4 and $Can5.6 million when used as an alternative to sitaxentan or bosentan, respectively.
Conclusions
Ambrisentan is less costly than other available ERAs, including bosentan and sitaxentan, but is more costly than sildenafil. In PAH patients in whom an ERA is the preferred agent, ambrisentan may be the drug of choice because of its economic advantages and improved safety profile.










Similar content being viewed by others
References
McLaughlin VV, Presberg KW, Doyle RL, et al. Prognosis of pulmonary arterial hypertension: ACCP evidence based clinical practice guidelines. Chest 2004; 126: 78–92S
Gabbay E, Reed A, Williams TJ. Assessment and treatment of pulmonary arterial hypertension. Intern Med J 2007; 37: 38–48
D’Alonzo GE, Barst RJ, Ayers SM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective study. Ann Intern Med 1991; 115: 343–9
Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol with conventional therapy for pulmonary arterial hypertension. N Engl J Med 1996; 334: 296–301
Galiè N, Seeger W, Naeije R, et al. Comparative analysis of clinical trials and evidence based treatment algorithm in pulmonary arterial hypertension. J Am Coll Cardiol 2004; 43: 81–8S
McLaughlin VV, Shillington A, Risk S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation 2002; 106: 1477–82
Sitbon O, Humbert M, Jaïs X, et al. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation 2005; 111: 3105–11
Langleben D, Archer S, Granton J, et al. Canadian Cardiovascular Society and Canadian Thoracic Society position statement on pulmonary arterial hypertension. Can J Cardiol 2005; 21: 909–14
Thenappan T, Shah SJ, Rich S, et al. A USA-based registry for pulmonary arterial hypertension: 1982–2006. Eur Respir J 2007; 30: 1103–10
Torres F. Systematic review of randomized, double blind clinical trials of oral agents conducted in patients with pulmonary arterial hypertension. Int J Clin Pract 2007; 61: 1756–65
Park MH. Advances in diagnosis and treatment in patients with pulmonary arterial hypertension. Catheter Cardiovasc Interv 2008; 71: 205–13
Rubin L, Badesch DB, Barst RJ, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med 2002; 346: 896–903
Barst RJ, Langleben D, Frost A, et al. Sitaxsentan therapy for pulmonary arterial hypertension. Am J Respir Crit Care Med 2004; 169: 441–47
Galiè N, Ghofrani HA, Torbicki A, et al. Sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med 2005; 353: 2148–57
Naeije R, Huez S. Expert opinion on available options treating pulmonary arterial hypertension. Expert Opin Pharmacother 2007; 8: 2247–65
Barst RJ. A review of pulmonary arterial hypertension: role of ambrisentan. Vasc Health Risk Manag 2007; 3: 11–22
Galiè N, Olschewski H, Oudiz RJ, et al. Ambrisentan for the treatment of pulmonary arterial hypertension: results of the ambrisentan in pulmonary arterial hypertension, randomized, double-blind, placebo-controlled, multicenter, efficacy (ARIES) study 1 and 2. Circulation 2008; 117: 3010–9
Oudiz RJ. Long term ambrisentan therapy provides sustained benefit in patients with pulmonary arterial hypertension [abstract]. Chest 2007; 132: 474s
Torres F. Ambrisentan improved multiple scales of the SF-36 health survey in patients with pulmonary arterial hypertension [abstract]. Chest 2007; 132: 634s
McGoon MD, Frost AE, Oudiz RJ, et al. Ambrisentan therapy in patients with pulmonary arterial hypertension who discontinued bosentan or sitaxsentan due to liver function test abnormalities. Chest 2009; 135: 122–9
Drummond MF, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programs. Oxford: Oxford University Press, 1987
Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med 2006; 173: 1023–30
Peacock AJ, Murphy NF, McMurray JJ, et al. An epidemiological study of pulmonary arterial hypertension. Eur Respir J 2007; 30: 104–9
Badesch DB, Abman SH, Simonneau G, et al. Medical therapy for pulmonary arterial hypertension: updated ACCP evidence-based clinical practice guidelines. Chest 2007; 131: 1917–28
Statistics Canada. Quarterly demographic estimates: July to September 2007 [online]. Available from URL: http://dsp-psd.pwgsc.gc.ca/collection_2007/statcan/91-002-X/91-002-XIE2007003.pdf [Accessed 2008 Jun 21]
Barst RJ, Langleben D, Badesch D, et al. Treatment of pulmonary arterial hypertension with the selective endothelin-A receptor antagonist sitaxsentan. J Am Coll Cardiol 2006; 47: 2049–56
Simonneau G, Rubin LJ, Galiè N, et al. Addition of sildenafil to long-term intravenous epoprostenol therapy in patients with pulmonary arterial hypertension: a randomized trial. Ann Intern Med 2008; 149: 521–30
Einarson TR, Granton JT, Vincente C, et al. Cost effectiveness of treprostinil versus epoprostenol in patients with pulmonary arterial hypertension: a Canadian analysis. Can Resp J 2005; 12: 419–25
Olschewski H, Galiè N, Kramer M, et al. Ambrisentan improves exercise capacity and time to clinical worsening in patients with pulmonary arterial hypertension: results of the ARIES-2 study [abstract]. 102nd International Conference of the American Thoracic Society; 2006 May 19–24; San Diego (CA)
Channick RN, Simonneau G, Sitbon O, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomized placebo-controlled study. Lancet 2001; 358: 1119–23
Galiè N, Beghetti M, Gatzoulis MA, et al. Bosentan therapy in patient with Eisenmenger syndrome: a multicenter, double-blind, randomized, placebo-controlled study. Circulation 2006; 114: 48–54
Lewis GD, Shah R, Shahzad K, et al. Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation 2007; 116: 1555–62
Wlodarczyk JH, Cleland LG, Keogh AM, et al. Public funding of bosentan for the treatment of pulmonary artery hypertension in Australia: cost effectiveness and risk sharing. Pharmacoeconomics 2006; 24: 903–15
Highland KB, Strange C, Mazur J, et al. Treatment of pulmonary arterial hypertension: a preliminary decision analysis. Chest 2003; 124: 2087–92
Wilkins MR, Paul GA, Strange JW, et al. Sildenafil versus endothelin receptor antagonist for pulmonary hypertension study. Am J Respir Crit Care Med 2005; 171: 1292–7
Acknowledgements
This study was funded by GlaxoSmithKline Canada Inc. George Dranitsaris has acted as consultant to GlaxoSmithKline Canada Inc. to develop this cost-minimization model. GlaxoSmithKline did not contribute in any way to the methodology employed or to the interpretation of the results. Sanjay Mehta has received consulting and speaking fees from pharmaceutical firms (Actelion Pharmaceuticals, Encysive, GlaxoSmithKline, Northern Therapeutics, Pfizer), and clinical investigator fees from pharmaceutical firms (Actelion, Encysive, Lilly, Pfizer, United Therapeutics) that own, market and distribute pharmacological agents for the treatment of pulmonary hypertension. George Dranitsaris had full access to all the data in the study and had the responsibility for the final decision to submit the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dranitsaris, G., Mehta, S. Oral therapies for the treatment of pulmonary arterial hypertension. Appl Health Econ Health Policy 7, 43–59 (2009). https://doi.org/10.1007/BF03256141
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256141