Abstract
The mandatory nature of recommendations made by the National Institute for Health and Clinical Excellence (NICE) in the UK has highlighted inherent difficulties in the process of disinvestment in existing technologies to fund NICE-approved technologies. A lack of evidence on candidate technologies means that the process of disinvestment is subject to greater uncertainty than the investment process, and inefficiencies may occur as a result of the inverse evidence law.
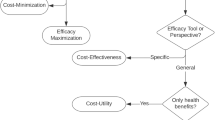
This article describes a potential disinvestment scenario and the options for the decision maker, including the conduct of value of information analyses. To illustrate the scenario, an economic evaluation of a disinvestment candidate (screening for amblyopia and strabismus) is presented. Only very limited data were available. The reference case analysis found that screening is not cost effective at currently accepted values of a QALY. However, a small utility decrement due to unilateral vision loss reduced the incremental cost per QALY gained, with screening expected to be extremely cost effective.
The discussion highlights the specific options to be considered by decision makers in light of the model-based evaluation. It is shown that the evaluation provides useful information to guide the disinvestment decision, providing a range of focused options with respect to the decision and the decision-making process.
A combination of explicit model-based evaluation, and pragmatic and generalizable approaches to interpreting uncertainty in the decision-making process is proposed, which should enable informed decisions around the disinvestment of technologies with weak evidence bases.
Similar content being viewed by others
References
House of Commons Health Committee, National Institute for Health and Clinical Excellence. First report of session 2007-08. Vol. I. Report, together with formal minutes, 10 January 2008, London: The Stationery Office [online]. Available from URL: http://www.parliament.the-stationery-office.co.uk/pa/cm200708/cmselect/cmhealth/27/27.pdf [Accessed 2008 Aug 28]
National Institute for Health and Clinical Excellence. Response to the Health Select Committee’s report on the National Institute for Health and Clinical Excellence [online]. Available from URL: http://www.nice.org.uk/media/F51/D0/HSC2007OfficialResponseFINAL.pdf [Accessed 2008 Aug 28]
Elshaug AG, Moss JR, Littlejohns P, et al. Identifying existing health care services that do not provide value for money. Med J Aust 2009; 190(5): 269–73
Chilcott J, Brennan A, Booth A, et al. The role of modelling in planning and prioritising clinical trials. Health Technol Assess 2003; 7(23): iii, 1-125
Eckermann S, Willan AR. Expected value of information and decision making in HTA. Health Econ 2007; 16(2): 195–209
Snowdon SK, Stewart-Brown SL. Preschool vision screening. Health Technol Assess 1997; 1(8): i–iv, 1-83
Carlton J, Karnon J, Czoski-Murray C, et al. The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation. Health Technol Assess 2008; 12(25): iii, xi–194
Pediatric Eye Disease Investigator Group. A randomized trial of atropine versus patching for treatment of moderate amblyopia in children. Arch Ophthalmol 2002; 120: 268–78
Repka MX, Cotter SA, Beck RW, et al. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology 2004; 111: 2076–85
Karnon J, McIntosh A, Dean J, et al. A prospective hazard and improvement analytic approach to predicting the effectiveness of medication error interventions. Saf Sci 2007; 45: 523–39
Karnon J, Czoski Murray C, Smith KJ, et al. A hybrid cohort individual sampling natural history model of age-related macular degeneration: assessing the cost-effectiveness of screening using probabilistic calibration. Med Decis Making. Epub 2009 Jan 6
Dobson V, Fulton AB, Sebris SL. Cycloplegic refractions of infants and young children: the axis of astigmatism. Invest Ophthalmol Vis Sci 1984; 25(1): 83–7
Abrahamsson M, Fabian G, Andersson AK, et al. A longitudinal study of a population based sample of astigmatic children: I. Refraction and amblyopia. Acta Ophthalmol 1990; 68(4): 428–34
Abrahamsson M, Fabian G, Sjostrand J. A longitudinal study of a population based sample of astigmatic children: II. The changeability of anisometropia. Acta Ophthalmol 1990; 68(4): 435–40
Dobson V, Sebris SL. Longitudinal study of acuity and stereopsis in infants with or at-risk for esotropia. Invest Ophthalmol Vis Sci 1989; 30(6): 1146–58
Townshend AM, Holmes JM, Evans LS. Depth of anisometropic amblyopia and difference in refraction. Am J Ophthalmol 1993; 116(4): 431–6
Donahue SP. The relationship between anisometropia, patient age, and the development of amblyopia. Trans Am Ophthalmol Soc 2005; 103: 313–36
Ingram RM, Gill LE, Goldacre MJ. Emmetropisation and accommodation in hypermetropic children before they show signs of squint: a preliminary analysis. Bull Soc Belg Ophtalmol 1994; 253: 41–56
Ingram RM, Walker C, Wilson JM, et al. Prediction of amblyopia and squint by means of refraction at age 1 year. Br J Ophthalmol 1986; 70: 12–5
Williams C, Harrad RA, Harvey I, et al. Screening for amblyopia in preschool children: results of a population-based, randomised controlled trial. ALSPAC Study Team. Ophthal Epidemiol 2001; 8(5): 279–95
Stayte M, Reeves B, Wortham C, et al. Ocular and vision defects in preschool children. Br J Ophthalmol 1993; 77: 228–32
Schmidt P, Maguire M, Dobson V, et al. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision In Preschoolers Study. Ophthalmology 2004; 111(4): 637–50
Stewart CE, Moseley MJ, Stephens DA, et al., on behalf of the MOTAS cooperative. The treatment dose response in amblyopia therapy: results from the monitored occlusion treatment of amblyopia study (MOTAS). Invest Ophthalmol Vis Sci 2005; 45: 3048–54
Rahi J, Logan S, Timms C, et al. Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. Lancet 2002; 360(9333): 597–602
Meads C, Moore D. The clinical effectiveness and cost utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation. Health Technol Assess 2001; 7(9): 1–98
Brown MM, Brown GC, Sharma S, et al. Quality of life associated with unilateral and bilateral good vision. Ophthalmology 2001; 108: 643–8
Rahi JS, Cumberland PM, Peckham CS. Does amblyopia affect educational, health, and social outcomes? Findings from 1958 British birth cohort. BMJ 2006; 332: 820–5
Rubin GS, Munoz B, Bandeen-Roche K, et al. Monocular versus binocular visual acuity as measures of vision impairment and predictors of visual disability. Invest Ophthalmol Vis Sci 2000; 41(11): 3327–34
Kandel GL, Grattan PE, Bedell HE. Are the dominant eyes of amblyopes normal? Am J Optometry Physiol Optics 1980; 57(1): 1–6
Bruce A, Hurst M, Abbott H, et al. The incidence of refractive error and anomalies of binocular vision in infants. Br Orthoptic J 1991; 48: 32–5
Graham PA. Epidemiology of strabismus. Br J Ophthalmol 1974; 58(3): 224–31
Hopkisson B, Clarke JR, Oelman BJ. Residual amblyopia in recruits to the British Army. BMJ 1982; 285(6346): 940
Williams C, Horwood J, Northstone K, et al. The timing of patching treatment and a child’s well-being. Br J Ophthalmol 2006; 90: 670–1
Karnon J. Planning the efficient allocation of research funds: an adapted application of a non-parametric Bayesian value of information analysis. Health Pol 2002; 61(3): 329–47
NICE guide to the methods of health technology appraisal. London: NICE, 2004
Nutbeam D. How does evidence influence public health policy? Tackling health inequalities in England. Health Promot J Aust 2003; 14: 154–58
Koopmanschap MA, Rutten FFH, van Ineveld BM, et al. The friction cost method for estimating the indirect costs of disease. J Health Econ 1995; 14: 171–89
Weinstein MC, O’Brien B, Hornberger J, et al. Principles of good practice for decision analytic modeling in healthcare evaluation: report of the ISPOR Task Force on Good Research Practices-Modeling Studies. Value Health 2003; 6(1): 9–17
Philips Z, Bojke L, Sculpher M, et al. Good practice guidelines for decision-analytic modelling in health technology assessment: a review and consolidation of quality assessment. Pharmacoeconomics 2006; 24(4): 355–71
Acknowledgements
The case study reported in this article was funded by a project grant from the Health Technology Assessment programme (04/32/05). There are no known conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Karnon, J., Carlton, J., Czoski-Murray, C. et al. Informing disinvestment through cost-effectiveness modelling. Appl Health Econ Health Policy 7, 1–9 (2009). https://doi.org/10.1007/BF03256137
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256137