Abstract
Background
The association between antiretroviral adherence, healthcare utilization and medical costs has not been well studied.
Objective
To examine the relationship of adherence to antiretroviral medications to healthcare utilization and healthcare costs.
Methods
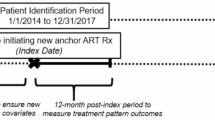
A retrospective cohort study was conducted using data from 325 previously antiretroviral medication-naive HIV-infected individuals initiating first antiretroviral therapy from 1997 through 2003. The setting was an inner-city safety net hospital and HIV clinic in the US. Adherence was assessed using pharmacy refill data. The average wholesale price was used for prescription costs. Healthcare utilization data and medical costs were obtained from the hospital billing database, and differences according to quartile of adherence were compared using analysis of variance (ANOVA). Multivariate logistic regression was used to assess predictors of higher annual medical costs. Sensitivity analyses were used to examine alternative anti-retroviral pricing schemes. The perspective was that of the healthcare provider, and costs were in year 2005 values.
Results
In 325 patients followed for a mean (± SD) 3.2 (1.9) years, better adherence was associated with lower healthcare utilization but higher total medical costs. Annual non-antiretroviral medical costs were $US7612 in the highest adherence quartile versus $US10 190 in the lowest adherence quartile. However, antiretroviral costs were significantly higher in the highest adherence quartile ($US17 513 vs $US8690), and therefore the total annual medical costs were also significantly higher in the highest versus lowest adherence quartile ($US25 125 vs $US18 880). In multivariate analysis, for every 10% increase in adherence, the odds of having annual medical costs in the highest versus lowest quartile increased by 87% (odds ratio 1.87; 95% CI 1.45, 2.40). In sensitivity analyses, very low antiretroviral prices (as seen in resource-limited settings) inverted this relationship — excellent adherence was cost saving.
Conclusion
Better adherence to antiretroviral medication was associated with decreased healthcare utilization and associated costs; however, because of the high cost of antiretroviral therapy, total medical costs were increased. Combination antiretroviral therapy is known to be cost effective; lower anti-retroviral costs may make it cost saving as well.





Similar content being viewed by others
References
Bozzette SA, Joyce G, McCaffrey DF, et al. Expenditures for the care of HIV-infected patients in the era of highly active antiretroviral therapy. N Engl J Med 2001 Mar 15; 344(11): 817–23
Yazdanpanah Y, Goldie SJ, Losina E, et al. Lifetime cost of HIV care in France during the era of highly active anti-retroviral therapy. Antivir Ther 2002 Dec; 7(4): 257–66
Chen RY, Accortt NA, Westfall AO, et al. Distribution of health care expenditures for HIV-infected patients. Clin Infect Dis 2006 Apr 1; 42(7): 1003–10
Schackman BR, Gebo KA, Walensky RP, et al. The lifetime cost of current human immunodeficiency virus care in the United States. Med Care 2006 Nov; 44(11): 990–7
Rietmeijer CA, Davidson AJ, Foster CT, et al. Cost of care for patients with human immunodeficiency virus infection: patterns of utilization and charges in a public health care system. Arch Intern Med 1993 Jan 25; 153(2): 219–25
Keiser P, Nassar N, Kvanli MB, et al. Long-term impact of highly active antiretroviral therapy on HIV-related health care costs. J Acquir Immune Defic Syndr 2001 May 1; 27(1): 14–9
Palella Jr FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 1998 Mar 26; 338(13): 853–60
Tramarin A, Campostrini S, Postma MJ, et al. A multicentre study of patient survival, disability, quality of life and cost of care: among patients with AIDS in northern Italy. Pharmacoeconomics 2004; 22(1): 43–53
Cleary SM, McIntyre D, Boulle AM. The cost-effectiveness of antiretroviral treatment in Khayelitsha, South Africa: a primary data analysis. Cost Eff Resour Alloc 2006; 4: 20
Freedberg KA, Losina E, Weinstein MC, et al. The cost effectiveness of combination antiretroviral therapy for HIV disease. N Engl J Med 2001 Mar 15; 344(11): 824–31
Miners AH, Sabin CA, Trueman P, et al. Assessing the cost-effectiveness of HAART for adults with HIV in England. HIV Med 2001 Jan; 2(1): 52–8
Sendi PP, Bucher HC, Harr T, et al. Cost effectiveness of highly active antiretroviral therapy in HIV-infected patients. Swiss HIV Cohort Study. AIDS 1999 Jun 18; 13(9): 1115–22
Badri M, Maartens G, Mandalia S, et al. Cost-effectiveness of highly active antiretroviral therapy in South Africa. PLoS Medicine 2006 Jan; 3(1): e4
Bangsberg DR, Perry S, Charlebois ED, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS 2001 Jun 15; 15(9): 1181–3
Hogg RS, Heath K, Bangsberg D, et al. Intermittent use of triple-combination therapy is predictive of mortality at baseline and after 1 year of follow-up. AIDS 2002 May 3; 16(7): 1051–8
Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000 Jul 4; 133(1): 21–30
Gabow P, Eisert S, Wright R. Denver Health: a model for the integration of a public hospital and community health centers. Ann Intern Med 2003 Jan 21; 138(2): 143–9
Gardner EM, Burman WJ, Maravi ME, et al. Selective drug taking during combination antiretroviral therapy in an unselected clinic population. J Acquir Immune Defic Syndr 2005 Nov 1; 40(3): 294–300
Gardner EM, Burman WJ, Maravi ME, et al. Durability of adherence to antiretroviral therapy on initial and subsequent regimens. AIDS Patient Care STDs 2006 Sep; 20(9): 628–36
Wood E, Hogg RS, Yip B, et al. Is there a baseline CD4 cell count that precludes a survival response to modern anti-retroviral therapy? AIDS 2003 Mar 28; 17(5): 711–20
Red book: pharmacy’s fundamental reference. Montvale (NJ): Thomson Healthcare, Inc., 2005
Industry data. Producer price index - PPI. Washington, DC: US Department of Labor, Bureau of Labor Statistics [online]. Available from URL: http://www.bls.gov/data/ [Accessed 2007 May 11]
Bangsberg DR, Kroetz DL, Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep 2007 May; 4(2): 65–72
Duncan DB. Multiple range and multiple F tests. Biometrics 1955; 11: 1–42
Gencarelli DM. Average wholesale price for prescription drugs: is there a more appropriate pricing mechanism? NHPF Issue Brief 2002 Jun 7; (775): 1–19
Public Health Services Act, 42 United States Code, Section 256b. Limitation on prices of drugs purchased by covered entities.
Steinbrook R. Thailand and the compulsory licensing of efavirenz. N Engl J Med 2007 Feb 8; 356(6): 544–6
Acurcio Fde A, Puig-Junoy J, Bonolo Pde F, et al. Cost-effectiveness of initial adherence to antiretroviral therapy among HIV infected patients in Belo Horizonte, Brazil [in Spanish]. Rev Esp Salud Publica 2006 Jan-Feb; 80(1): 41–54
Purdum AG, Johnson KA, Globe DR. Comparing total health care costs and treatment patterns of HIV patients in a managed care setting. AIDS Care 2004 Aug; 16(6): 767–80
Nachega J, Hislop M, Omer S, et al. Effect of adherence to NNRTI-based ART on health care costs in a private sector HIV/AIDS management program in southern Africa. [abstract no. 548]. 14th Conference on Retroviruses and Opportunistic Infections; 2007 Feb 25–28; Los Angeles (CA)
White TJ, Vanderplas A, Chang E, et al. The costs of non-adherence to oral antihyperglycemic medication in individuals with diabetes mellitus and concomitant diabetes mellitus and cardiovascular disease in a managed care environment. Dis Manage Health Outcomes 2004; 12(3): 181–8
Cantrell CR, Eaddy MT, Shah MB, et al. Methods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomes. Med Care 2006 Apr; 44(4): 300–3
White TJ, Vanderplas A, Ory C, et al. Economic impact of patient adherence with antidepressant therapy within a managed care organization. Dis Manage Health Outcomes 2003; 11(12): 817–22
Wood E, Hogg RS, Yip B, et al. Effect of medication adherence on survival of HIV-infected adults who start highly active antiretroviral therapy when the CD4+cell count is 0.200 to 0.350 × 10(9) cells/L. Ann Intern Med 2003 Nov 18; 139(10): 810–6
Mannheimer SB, Matts J, Telzak E, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care 2005 Jan; 17(1): 10–22
Kumarasamy N. Generic antiretroviral drugs: will they be the answer to HIV in the developing world? Lancet 2004 Jul 3–9; 364(9428): 3–4
Kumarasamy N, Vallabhaneni S, Flanigan TP, et al. Rapid viral load suppression following generic highly active antiretroviral therapy in Southern Indian HIV-infected patients. AIDS 2005 Mar 24; 19(6): 625–7
Laurent C, Kouanfack C, Koulla-Shiro S, et al. Effectiveness and safety of a generic fixed-dose combination of nevirapine, stavudine, and lamivudine in HIV-1-infected adults in Cameroon: open-label multicentre trial. Lancet 2004 Jul 3–9; 364(9428): 29–34
Sansom SL, Anthony MN, Garland WH, et al. The costs of HIV antiretroviral therapy adherence programs and impact on health care utilization. AIDS Patient Care STDs 2008 Feb; 22(2): 131–8
Press N, Tyndall MW, Wood E, et al. Virologic and im-munologic response, clinical progression, and highly active antiretroviral therapy adherence. J Acquir Immune Defic Syndr 2002 Dec 15; 31 Suppl. 3: S112–7
Goldie SJ, Paltiel AD, Weinstein MC, et al. Projecting the cost-effectiveness of adherence interventions in persons with human immunodeficiency virus infection. Am J Med 2003 Dec 1; 115(8): 632–41
Acknowledgements
This study was presented in part at the 13th Conference on Retroviruses and Opportunistic Infections, Denver, CO, USA, 5–8 February 2006, poster no. 536.
This research was supported in part through the Bristol-Myers Squibb Virology Fellows Research Program, the Centers for Disease Control and Prevention grant U62/CCU806243, Adolescent and Adult Spectrum of Disease and Supplement to HIV/AIDS Surveillance. Dr Gardner is supported through the National Institute of Allergy and Infectious Diseases (NIAID) K01 AI067063. Dr Davidson is supported through a Health Resources and Services Administration (HRSA) grant (1 D12 HP 00054 PI: deGruy) for Academic Administrative Units in Primary Care.
The study design, data collection, data analysis, data interpretation, manuscript preparation and decision for submission were under the sole authority of the authors and decisions were made independently from the funders. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gardner, E.M., Maravi, M.E., Rietmeijer, C. et al. The association of adherence to antiretroviral therapy with healthcare utilization and costs for medical care. Appl Health Econ Health Policy 6, 145–155 (2008). https://doi.org/10.1007/BF03256129
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256129