Zusammenfassung
Hintergrund
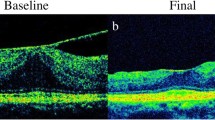
Macular pucker (MP) oder epiretinale Gliose führt zu Visus(ver)minderung und Metamorphopsien. Dies ist wegen Makulaelevation oder-distorsion durch Membranbildung in der vitreoretinalen Grenzschicht mit traktilen Elementen bedingt. Das zeitweise vorhandene zystoide Makulaödem kommt durch Verziehung der tight junctions und somit Störungen der Blut/Retina-Schranke sowie des Pigmentepithel-Pumpenmechanismus zustande.
Patienten und Methode
Es wurden bei 57 Patienten 58 Operationen durchgeführt. Es wurde zwischen „idiopathischem“ und „sekundärem“ MP unterschieden. Im Falle eines ausreichenden Materialgewinnes wurde eine histologische und histochemische Ausarbeitung veranlasst. Wir führten eine Pars plana Vitrektomie (PPV) mit komplettem oder teilweisem Peeling der zentralen Membran, eventuell kombiniert mit Kataraktoperation, durch.
Ergebnisse
Es kam in 73% der Fälle zum Visusanstieg, in 20% zur Visusverminderung, in 7% der Fälle blieb der Visus unverändert. Die postoperativen Komplikationen schliessen Kataraktentwicklung, Amotio retinae, Membranrezidiv, Aderhautamotio, subretinale Fibröse und Makulaforamen ein.
Der höchsterreichte postoperative Visus war zwischen dem 3. und 6. postoperativen Monat zu erheben.
Diskussion
Durch die PPV kam es in den meisten Fällen zum Visusanstieg. Das subjektive Empfinden war aufgrund der fehlenden Metamorphopsien auch bei niedrigen Visuswerten deutlich besser. Es zeigte sich deutlicher Zellreichtum in der Histologie der Membranen bei sekundärem Pucker. Aufgrund der hohen Kataraktentwicklungsrate nach PPV geben wir dem kombinierten praeoprativen Vorgehen (PPV mit Kataraktoperation) den Vorzug.
Summary
Background
Macular Pucker (MP) or epiretinal Gliosis leads to loss of vision accompanied by metamorphopsia. This is because of macula elevation or distortion through epimacular membranes with tractable elements. The occasionally observed oedema, with ist cystoid character, is based on the distortion and dysfunction of tight junctions with disturbances in blood/retina barrier and epithelial pump function.
Patients and methods
58 operations were carried out on 57 patients who were separated into two groups with idiopathic and secondary MP. We performed a pars plana vitrectomy (PPV) with complete or partial peeling of central membrane eventually in combination with a cataract operation. After that the surgically removed material was studied using histologic and histochemic methods.
Results
In 73% of the cases, we had an improvement in postoperative vision. It decreased in 20% of the cases and in 7% remained unchanged. The postoperative complications were cataract development, retinal detachment, recurrence of epimacular membrane, postoperative sclerosis, macular hole and chorioidal detachment.
The best result in visual acuity was achieved 3 to 6 months postoperatively.
Discussion
— Vision improved in most eyes after surgical removal of epiretinal membrane
-
After removal of membrane, in absence of metamorphosis, even in cases with less improvement in vision, patients felt subjectively much better
-
The histology of membrane in secondary MP, was obviously rich in cell number specially fibrocytes
Similar content being viewed by others
Literatur
Chaudhury P, Chen W, Hunt Rc (1997) Production of plateletderived growth factor by interleukin-1 beta and transforming growth factor-beta-stimulated retinal pigment epithelial cells leads to contraction of collagen gels. Invest Ophthalmol Vis Sci 38: 824–933
Clarkson JG, Gree WR, Massof D (1977) A histological review of 168 cases of preretinal membrane. Am J Ophthalmol 84: 1–17
Foos RY (1978) Nonvascular proliferative extraretinal retinopathies. Am J Ophtalmol 86: 723–725
Gass JDM (1987) Stereoscopic atlas of macular diseases: Diagnosis and treatment. The CV Mosby, St. Louis
Kampik A, Green WR, Michels RG, Nase PK (1980) Ultrastructural features of progressive idopathic epiretinal membrane removed by vitreous surgery. Am J Ophthalmol 90: 797–809
Kleiner H (1954) Primäre Netzhautfältelung im Maculabereich. Graefes Arch Klin Exp Ophthalmol 155: 350–358
Laqua H, Machemer R (1975) Clinical-pathological correlation in massive preretinal proliferation. Am J Ophthalmol 80: 913–929
Maumenee AE (1967) Further advances in the study of the macula. Arch Ophthalmol 78: 151–165
Michels RG (1982) A clinical and histopathologic study of epiretinal membranes Affecting the macula and removed by vitreous surgery. Trans Am Ophthalmol Soc 80: 580–656
Rice TA, de Bustros S, Michels RG, Thompson JT, DeBanne SM, Rowland DY (1986) Prognostic factors in vitrectomy for epiretinal membranes of the macula. Ophthalmology 93: 602–610
Roth AM, Foos RY (1971) Surface wrinkling retinopathy in eyes enucleated at atopsy. Trans Am Acad Ophtalmol Otolarngol 75: 1047–1058, 1071
Sidd RJ, Fine St, Owens SL, Patz A (1982) Idiopathic preretinal gliosis. Am J Ophthalmol 94: 44–48
Singh AK, Michels RG, Glaser MB (1986a) Scierai indentation following cryotherapy and repeat cryotherapy enhance release of viable pigment epithelial cells. Retina 6: 176–178
Singh AK, Glaser BM, Lemor M, Michels RG (1986b) Gravity dependent distribution of retina pigment epithelial cells dispersed into the vitreous cavity. Retina 6: 77–80
Smiddy WE, Michels RG, Glaser BM, De Bustros S (1988) Vitrectomy for macular traction caused by incomplete vitreous seperation: Arch Ophthalmol 106: 624–628
Smith-Thomas L, Richardson P, Parsons MA, Rennie IG, Benson M, MacNeil S (1996) Additive effect of extracellular matrix proteins and platelet derived mitogens on human retinal pigment epithelial cell prolieration and contraction. Curr Eye Res 15: 739–748
Spitznas M, Leuenberger R (1977) Die primäre epiretinale Gliose. Klin Monatsbl Augenheilkd 171: 410–420
Schönfeld CL (1997) Expression der Metaloproteinase Stromelysin in humanem retinalen Pigmentepithel (RPE). Der Ophthalmologe 94: 629–933
Trese MT, Chandler DB, Machemer R (1983) Macular pucker. I. Prognocstic criteria. Graefes Arch Cin Exp Ophthalmol 221: 12–15 (1983)
Wise GN (1975) Relationship of idiopathic preretinal macular fibrosis to posterior Vitreous detachment. Am J Ophthalmol 79: 358–362
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Abri, A., Stolba, U., Krebs, I. et al. Retrospektive Studie von 57 Fällen mit Macular pucker. Spektrum Augeheilkd 14, 259–261 (2000). https://doi.org/10.1007/BF03162828
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03162828