Abstract
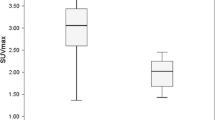
Tc-99m DTPA galaetosyl human serum albumin (Tc-99m GSA) hepatie seintigraphy was performed in two patients with patent ductus venosus before and after operation. To evaluate the portosystemic shunt flow, per-reatal portal scintigraphy with I-123 N-isopropyl-p-iodoamphetamine (IMP) was undergone in the same period. The portosystemic shunt indices (PSS index) were decreased from 67.9% to 7.3% in the patient 1, and from 77.3% to 22.7% in the patient 2, respectively. Quantitative indices of Tc-99m GSA hepatic scintigraphy improved dramatically in both patients. Under microscopic examination, nearly all the hepatic cells showed signs of severe fatty degeneration. After the operation, the severe fatty degeneration was alleviated and all the hepatic cells appeared normal. I-123 IMP per-rectal portal scintigraphy and Tc-99m GSA hepatic scintigraphy were useful in evaluating the quantitative shunt flow of the persistent ductus venosus and its hepatic functional reserve.
Similar content being viewed by others
References
Loberant N, Barak M, Gaitini D, Herskovits M, Ben-Elisha M, Roguin N. closure of the ductus venosus in neonates: findings on real-time gray-scale, color-flow Doppler, and duplex Doppler sonography.AJR 159: 1083–1085, 1992.
Adams FH. Fetal circulation and alteration at birth.In: Moss AJ, Adams FH, Emmanouilides GC. Heart disease in infants, children and adolescents, 2nd edn. Williams and Wilkins Co., Baltimore, pp. 11–17, 1978.
Barksy MF, Rankin RN, Wall WJ, Ghent CN, Garcia B. Patent ductus venosus: problems in assessment and management.Can J Surg 32: 271–275, 1989.
Ohnishi K, Hatano H, Nakayama T, Kohno K, Okuda K. An unusual portal-systemic shunt, most likely through a patient ductus venosus. A case report.Gastroenterology 85: 962–965, 1983.
Mitchell IM, Pollock JC, Gibson AA. Patent ductus venosus.Pediatr Cardiol 12: 181–183, 1991.
Uchino T, Endo F, Ikeda S, Shiraki K, Sera Y, Matsuda I. Three brothers with progressive hepatic dysfunction and severe hepatic steatosis due to a patient ductus venosus.Gastroenterology 110: 1964–1968, 1996.
Shimomura T, Tomiguchi S, Kojima A, Hara M, Nakashima R, Gyama Y, et al. I-ISS IMP per-rectal portal seintigraphy for evaluation of the portal hemodynamics after hepatic embolization.Kumamoto Medical Journal 44 (3): 77–90, 1993.
Maisawa S, Takasago Y, Oyake Y, Maeta H, Pujiwara T. Patent ductus venosus with hypoplastic right hepatoportal system in a young child born with asymmetric intra-uterine growth retardation.Eur J Pediatr 151: 569–571, 1992.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kira, T., Ikeda, S., Sera, Y. et al. Evaluation of persistence of ductus venosus with Tc-99m DTPA galactosyl human serum albumin liver scintigraphy and I-123 iodoamphetamine per-rectal portal scintigraphy. Ann Nucl Med 14, 213–216 (2000). https://doi.org/10.1007/BF02987862
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02987862