Abstract
Background
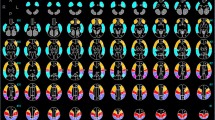
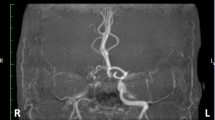
We evaluated the cerebral hemodynamics in childhood moyamoya disease patients before and after surgery to assess both surgical indication and the effect of revascularization using single photon emission computed tomography (SPECT) study with N-isopropyl-p-l23I-iodoamphetamine (IMP). We compared results of quantitative and semi-quantitative SPECT studies to determine parameters by the semi-quantitative method to define severe hemodynamic ischemia.
Methods
There were 14 pediatric patients with moyamoya disease who suffered transient ischemic attacks (TIAs) in the anterior circulation. Before and after surgical revascularization by STA-MCA bypass and encephalomyosynangiosis (EMS), quantitative IMP-SPECT studies using the autoradiographic method (IMP-ARG method) were performed. Resting regional cerebral blood flow (rCBF) and regional vascular reserve (rVR) were measured in bilateral cortical territories (ROI) and cerebellum. Semi-quantitative parameters were calculated from the ratio of ROI counts to the dominant cerebellar counts (ROI/Ce ratio) at resting and acetazolamide-activated conditions.
Results
Before surgery, the mean resting rCBF and rVR in bilateral ACA and MCA territories were less than 40 m//100 g/min and less than 10%, respectively, indicating severe hemodynamic ischemia. Except for the ACA territories, both the mean resting rCBF and mean rVR values in the entire cortex increased significantly after surgery (p < 0.05). By semi-quantitative studies, before surgery, the mean resting and acetazolamide-activated ROI/Ce ratios in bilateral ACA and MCA territories were less than 0.90 and 0.80, respectively. The mean resting and acetazolamide-activated ROI/Ce ratios increased significantly in the MCA territory after surgery. Severe hemodynamic ischemia, which categorized by the quantitative thresholds (resting rCBF < 40 m//100 g/min and rVR < 10%) was diagnosed by the semi-quantitative thresholds (resting ROI/ Ce ratio < 0.90 and acetazolamide-activated ROI/Ce ratio < 0.85), the sensitivity and specificity of which were 87.5% and 90.9%, respectively.
Conclusions
The cerebral hemodynamics in childhood moyamoya disease was improved entirely after surgery. Severe hemodynamic cerebral ischemia was diagnosed by not only quantitative but also semi-quantitative IMP-SPECT studies.
Similar content being viewed by others
References
Suzuki J, Takaku A. Cerebrovascular ‘Moyamoya’ disease. Disease showing abnormal net-like vessels in base of brain.Arch Neurol 1969; 20:288–299.
Kurokawa T, Tomita S, Ueda K. Prognosis of occlusive disease of the circle of Willis in children.Pediatr Neurol 1985; 1:274–277.
Fukuyama Y, Umezu R. Clinical cerebral angiographic evaluations of idiopathic progressive occlusive disease of the circle of Willis in children.Brain Dev 1985; 7:21–37.
Imaizumi T, Hayashi K, Saito K. Long term outcomes of pediatric moyamoya disease monitored to adulthood.Pediatr Neurol 1998; 18:321–325.
Yonas H, Smith HA, Durham SR, Pentheny SL, Johnson DW, Holly A, et al. Increased stroke risk predicted by compromised cerebral blood flow reactivity.J Neurosurg 1993; 79:483–489.
Goto Y, Yonekawa Y. Worldwide distribution of moyamoya disease.Neurol Med Chir (Tokyo) 1992; 32:883–886.
Yonekawa Y, Handa H, Okuno T. Moyamoya disease: diagnosis, treatment, and recent achievements. In: Barnett HJM, Mohr JP, Stein BM, Yatsu FM, eds.Stroke: Patho-physiology, Diagnosis, and Management. 2nd ed. New York, NY; Churchill Livingstone, Inc., 1992: 721–747.
Fukui M. Current state of study on moyamoya disease in Japan.Surg Neurol 1997; 47:138–143.
Karasawa J, Kikuchi H, Furuse S, Kawamura J, Sasaki T. Treatment of Moyamoya disease with STA-MCA anastomosis.J Neurosurg 1978; 49:679–688.
Karasawa J, Touho H, Ohonishi H, Miyamoto S, Kikuchi H. Cerebral revascularization using omental transplantation for childhood moyamoya disease.J Neurosurg 1993; 79:192–196.
Karasawa J, Kikuchi H, Furuse S, Sasaki T, Yoshida Y, Ohnishi H, et al. A surgical treatment of ’Moyamoya disease’: ’Encephalo-myo-synangiosis’.Neurol Med Chir 1997; 17 (Part 1):29–37.
Ishikawa T, Houkin K, Kamiyama H, Abe H. Effects of surgical revascularization on outcome of patients with pediatrie moyamoya disease.Stroke 1997; 28:1170–1173.
Ikezaki K, Matsushima T, Kuwabara Y, Suzuki S, Nomura T, Fukui M. Cerebral circulation and oxygen metabolism in childhood Moyamoya disease: a perioperative positron emission tomography study.J Neurosurg 1994; 81:843–850.
Kuwabara Y, Ichiya Y, Otsuka H, Takahara T, Gunasekera R, Hasuo K, et al. Cerebral hemodynamic change in the child and the adult with Moyamoya disease.Stroke 1990; 21:272–277.
Taki W, Yonekawa Y, Kobayashi A, Ishikawa M, Kikuchi H, Nishizawa S, et al. Cerebral circulation and oxygen metabolism in moyamoya disease of ischemie type in children.Child Nerve Syst 1988; 4:259–262.
Iida H, Itoh H, Nakazawa M, Hatazawa J, Nishimura H, Ohnishi Y, et al. Quantitative mapping of regional cerebral blood flow using iodine-123-IMP and SPECT.J Nucl Med 1994; 35:2019–2030.
Iida H, Akutsu T, Keigo E, Fukuda H, Inoue T, Itoh H, et al. A multicenter validation of regional cerebral flow quantification using123I iodoamphetamine and single photon emission computed tomography.J Cereb Blood Flow Metab 1996; 16:781–793.
Nakagawara J, Takeda R, Suematsu K, Nakamura J. Quantification of regional cerebral blood flow and vascular reserve in childhood Moyamoya disease using123IIMP-ARG method.Clin Neurol Neurosurg 1997; 99:96–99.
Ichihara T, Ogawa K, Motomura N, Kubo A, Hashimoto S. Compton scatter compensation using triple-energy window method for single- and dual-isotope SPECT.J Nucl Med 1993; 34:2216–2221.
Iida H, Narita Y, Kado H, Kashikura A, Sugawara S, Shoji Y, et al. Effects of scatter and attenuation correction on quantitative assessment of regional cerebral blood flow with SPECT.J Nucl Med 1998; 39; 181–189.
Holeman BL, Zimmerman RE, Schapiro JR, Kaplan ML, Jones AG, Hill TC. Biodistribution and dosimetry of N-isopropyl-p-l23I-iodoamphetamine in the primate.J Nucl Med 1983; 24:922–931.
Lieberman LM. The effect of radiation on the retina of the dog. PhD Dissertation, Univ. of Michigan, Ann Arbor, 1970.
Merrian GR Jr, Focht EF. A clinical study of radiation cataracts and relationship to dose.Am J Roentgen 1957; 77:759–785.
Babak AA, Michael B, Brian FH, Kanno I. A fully automatic multimodality image registration algorithm.J Comput Assist Tomogr 1995; 19:615–623.
Teves ST, Mitchell KD, Habboush IH. Three-dimensional image alignment, registration and fusion.Quart J Nucl Med 1998; 42:83–92.
Matsushima T, Fujiwara S, Nagata S, Fujii K, Fukui M, Kitamura K, et al. Surgical treatment for pediatric patients with Moyamoya disease by indirect revascularization procedures (EDAS, EMS, EMAS).Acta Neurochir 1989; 98:135–140.
Miyamoto S, Kikuchi H, Karasawa J, Nagata I, Yamazoe N, Akiyama Y. Pitfalls in surgical treatment of moyamoya disease: operative techniques for refractory cases.J Neurosurg 1998; 68:537–543.
Houkin K, Kamiyama H, Takahashi A, Kuroda S, Abe H. Combined revascularization surgery for childhood moyamoya disease: STA-MCA and encephalo-duro-arterio-myo-synangiosis (EDAMS): technical note.Child’s Nerv Syst 1997; 13:24–29.
Nariai T, Suzuki R, Matsushima Y, Ichimura K, Hirakawa K, Ishii K, et al. Surgically induced angiogenesis to compensate for hemodynamic cerebral ischemia.Stroke 1994; 25:1014–1021.
Mackenzie ET, Farrar JK, Fitch W, Graham DI, Gregory PC, Harper AM. Effects of hemorrhagic hypotension on the cerebral circulation. 1. Cerebral blood flow and pial arteri-olar caliber.Stroke 1979; 10:711–718.
Olsen J. Quantitative evaluation of normal and pathologic cerebral blood flow regulation to perfusion pressure.Arch Neurol 1973; 28:143–149.
Wood JH, Polyzoidis KS, Epstein CM, Gibby GL, Tindall GT. Quantitative EEG alterations after isovolemic hemodilu-tional augmentation of cerebral perfusion in stroke patients.Neurology 1984; 34:764–768.
Lassen NA, Friberg L, Rizzi D, Jensen JJ. Effect of aceta-zolamide on cerebral blood flow and brain tissue oxygenation.Postgrad Med J 1987; 63:185–187.
Lenzi GL, Frackowiak RSJ, Jones T. Cerebral oxygen metabolism and blood flow in human cerebral ischemic infarction.J Cereb Blood Flow Metab 1982; 2:321–335.
Martin WRW, Raichle ME. Cerebellar blood flow and metabolism in cerebral hemispheric infarction.Ann Neurol 1983; 14:168–176.
Yamauchi H, Fukuyama H, Kimura J. Hemodynamic and metabolic changes in crossed cerebellar hypoperfusion.Stroke 1992; 23:855–859.
Bogousslavsky J, Regli F. Vertebrobasilar transient ischemic attacks in internal carotid occlusion or tight stenosis.Arch Neurol 1985; 42:64–68.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Saito, N., Nakagawara, J., Nakamura, H. et al. Assessment of cerebral hemodynamics in childhood moyamoya disease using a quantitative and a semiquantitative IMP-SPECT study. Ann Nucl Med 18, 323–331 (2004). https://doi.org/10.1007/BF02984471
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02984471