Abstract
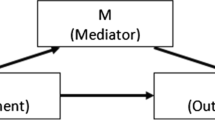
To secure the role of behavioral medicine in health care, researchers continue to improve the quality of their outcome studies. Despite the availability of guidelines for designing high quality clinical trials, however, we have noted two, unfortunately common, flaws in behavioral medicine outcome research that undermine these efforts. The first issue is that researchers recruit medical patients whose scores on psychological target measures are not elevated at pretest. Data are presented from quantitative reviews of cardiovascular and cancer populations to illustrate the impact of this protocol decision. It is demonstrated how magnitude of change and corresponding statistical power are greatly reduced when patients with few problems are enrolled. The second issue pertains to the failure of researchers to measure psychological change when the actual model to be tested is a mediational model such that successful treatment of psychological distress is presumed to account for good long-term health outcomes. Such lack of attention to protocol design can result in misinterpretation of obtained effects and can lead to premature dismissal of psychological treatment opportunities for physical disease. We suggest how these flaws can be avoided in the protocol design stage.
Similar content being viewed by others
References
Davidson KW, Goldstein M, Kaplan RM et al.: Evidence-based behavioral medicine: What is it and how do we achieve it?Annals of Behavioral Medicine. 2003,426:161–171.
Jacob RG, Chesney MA, Williams DM, Ding Y, Shapiro AP: Relaxation therapy for hypertension: Design effects and treatment effects.Annals of Behavioral Medicine. 1991,13:5–17.
Linden W, Chambers LA: Clinical effectiveness of non-drug therapies for hypertension: A meta-analysis.Annals Behavioral Medicine. 1994,16:35–45.
Nakao M, Yano E, Nomura S, Kuboki T: Blood pressure lowering effects of biofeedback treatment in hypertension: A meta-analysis of randomized controlled trials.Hypertension Research. 2003,26:37–46.
Chobanian AV, Bakris GL, Black HR, et al.: The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JNC VII.The Journal of the American Medical Association. 2003,289:2560–2571.
Linden W, Moseley JV: The efficacy of behavioral treatments for hypertension.Applied Psychophysiology and Biofeedback. 2006,31:51–63.
Linden W, Lenz JW, Con AH: Individualized stress management for primary hyper-tension: A controlled trial.Archives of Internal Medicine. 2001,161:1071–1080.
Cohen J:Statistical Power Analysis for the Behavioral Sciences (Rev. Ed.). New York: Academic, 1977.
Cohen J: A power primer.Psychological Bulletin. 1992,112:155–159.
McNair DM, Lorr M, Droppleman LF:Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service, 1971.
Frasure-Smith N, Prince R: The ischemic heart disease life stress monitoring Program: Impact on mortality.Psychosomatic Medicine. 1985,47:431–445.
Frasure-Smith N: In-hospital symptoms of psychological stress as predictors of long-term outcome after acute myocardial infarction in men.American Journal of Cardiology. 1991,67:121–127.
Baron RM, Kenny DA: The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations.Journal of Personality and Social Psychology. 1986,51:1173–1182.
Jones DA, West RR: Psychological rehabilitation after myocardial infarction: Multicentre randomized controlled trial.British Medical Journal. 1996,313:1517–1521.
Dusseldorp E, Van Elderen T, Maes S, Meulman J, Kraail V: A meta-analysis of psycho-educational programs for coronary heart disease patients.Health Psychology. 1999,18:506–519.
Hogan BE, Linden W, Najarian B: Social support interventions: do they work?Clinical Psychology Review. 2002,22:381–440.
Author information
Authors and Affiliations
Corresponding author
Additional information
We greatly appreciate the financial support provided to the authors while writing this article. The Canadian Institutes of Health Research provided operating funds to Wolfgang Linden, and the Social Sciences and Humanities Research Council of Canada supported Jillian R. Satin with a personnel award. Our colleagues Dr. Greg Miller and Dr. Joanne Stephen provided most helpful feedback on an earlier draft of this article.
About this article
Cite this article
Linden, W., Satin, J.R. Avoidable pitfalls in behavioral medicine outcome research. ann. behav. med. 33, 143–147 (2007). https://doi.org/10.1007/BF02879895
Issue Date:
DOI: https://doi.org/10.1007/BF02879895