Abstract
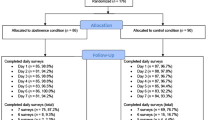
This study evaluated the effects of a putative activator of brain reward circuitry on outcomes in a 1 -y prospective comprehensive outpatient clinical program. As part of the Gene Narcotic Attenuation Program, Haveos (Synaptamine)™ was administered for the treatment of substance use disorder. Seventy-six patients (45 males and 31 females; mean age, 33 y [standard deviation, 7.0]) who had been given a diagnosis of serious substance use disorder were recruited. After exclusion of 15 patients who dropped out before the end of the study, self-reported craving decreased from program entrance to 12 wk (visual analog scale whereby 0 represents no craving and 5, the strongest craving) for 61 compliant patients (mean decrease, 2.85, 95% confidence interval [Cl], 2.65, 3.05); this improvement was significant (P < .001). Building up to relapse scores (each of 5 individual items and summary value) showed similar improvement after 1 y of treatment; the mean decrease in scores was significant for stress (t=3.3; P=.002), depression (t=4.0;P < .001), anger (t=4.4;P < .001), anxiety (t=4.5,P < .001), drug craving (t=5.4,P < .001), and summary building up to relapse (t=4.1;P < .001). Also, recovery score measures of energy level (t=8.4;P < .001) and ability to refrain from drug-seeking behavior (t=7.4;P < .001) showed significant mean increases from entry to 1 y. During the study, the alcoholic dropout rate was only 7% (4 of 57), which was significantly (Fisher’s exact test,P < .001) lower than the 73% (11 of 15) dropout rate reported for psychostimulant users. Although these results are significant, any interpretation must await the performance of rigorous double-blind studies.
Similar content being viewed by others
References
Office of National Drug Control Policy— 2004.The Economic Costs of Drug Abuse in the United States, 1992–2002. Washington, DC: Executive Office of the President (Publication No. 207303).
Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions.Arch Gen Psychiatry. 2004; 61: 807–816.
Blum K, Cull JG, Braverman ER, Comings DE. Reward deficiency syndrome.Am Scientist. 1996; 84: 132–145.
Gardner EL. Brain reward mechanisms. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, eds.Substance Abuse: A Comprehensive Textbook. Hagerstown, Md: Lippincott Williams & Wilkins; 1997: 51–58.
Blum K, Sheridan PJ, Wood RC, Braverman ER, Chen TJ, Comings DE. The D2 dopamine receptor gene as a determinant of reward deficiency syndrome.J Royal Soc Med. 1996; 89: 396–400.
Comings DE, Blum K. Reward deficiency syndrome: genetic aspects of behavioral disorders.Prog Brain Res. 2000; 126: 325–341.
Volkow ND, Wang GJ, Begleiter H, et al. High levels of dopamine D2 receptors in unaffected members of alcoholic families: possible protective factors.Arch Gen Psychiatry. 2006; 63: 999–1000.
Blum K, Sheridan PJ, Wood RC, Braverman ER, Chen TJ, Comings DE. Dopamine D2 receptor gene variants: association and linkage studies in impulsive-addictive-compulsive behavior.Pharmacogenetics. 1995; 5: 121–141.
Di Chiara G, Impereto A. Drugs abused by humans preferentially increase synaptic dopamine concentrations in the mesolimbic systems of freely moving rats.Proc Nat Acad Sci USA. 1988; 84: 1413–1416.
Blum K, Noble EP, Sheridan PJ, et al. Allelic association of human dopamine D2 receptor gene in alcoholism.JAMA. 1990; 263: 2055–2060.
Blum K, Noble EP, Volkow ND, Url G, Comings DE. First conference on reward deficiency syndrome: genetic antecedents and clinical pathways.Mol Psychiatry. 2001; 6(suppl): S1.
Bowirrat A, Oscar-Berman M. Relationship between dopaminergic neurotransmission, alcoholism, and reward deficiency syndrome.Am J Med Genet B Neuropsychiatr Genet. 2005; 132: 29–37.
Cheng HY, Laviolette SR, van der Kooy D, Penninger JM. DREAM ablation selectively alters THC place aversion and analgesia but leaves intact the motivational and analgesic effects of morphine.Eur J Neurosci. 2004; 19: 3033–3041.
Blum K, Chen TJH, Meshkin B, et al. Manipulation of catechol-O-methyl transferase (COMT) activity to influence the attenuation of substance seeking behavior, a subtype of reward deficiency syndrome (RDS), dependent upon gene polymorphisms: a hypothesis.Med Hyp. In press.
Manzardo AM, Penick EC. A theoretical argument for inherited thiamine insensitivity as one possible biological cause of familial alcoholism.Alcohol Clin Exp Res. 2006; 30: 1545–1550.
Kim KS, Lee KW, Lee KW, et al. Adenylyl cyclase type 5 (AC5) is an essential mediator of morphine action.Proc Natl Acad Sci USA. 2006; 103: 3908–3913.
Brandacher G, Winkler C, Aigner F, et al. Bariatric surgery cannot prevent tryptophan depletion due to chronic immune activation in morbidly obese patients.Obes Surg. 2006; 16: 541–548.
Linazaroso G, van Blercom N, Lasa A. Hypothesis: Parkinson’s disease, reward deficiency syndrome and addictive effects of levodopa.Neurologia. 2004; 19: 117–127.
Salmon AM, Evrard A, Damaj I, Changeux JP. Reduction of withdrawal signs after chronic nicotine exposure of alpha-calcitonin gene-related peptide knock-out mice.Neurosci Lett. 2004; 360: 73–76.
Simonin F, Valverde O, Smadja C, et al. Disruption of the kappa-opioid receptor gene in mice enhances sensitivity to chemical visceral pain, impairs pharmacological actions of the selective kappa-agonist U-50, 488H and attenuates morphine withdrawal. EMBO J. 1998; 17: 886–897.
Ponce G, Jimenez-Arriero MA, Rubio G, et al. The A1 allele of the DRD2 gene (Taq1 A polymorphisms) is associated with antisocial personality in a sample of alcohol-dependent patients.Eur Psychiatry. 2003; 18: 356–360.
Werme M, Hermanson E, Carmine A, et al. Decreased ethanol preference and wheel running in Nurr1-deficient mice.Eur J Neurosci. 2003; 17: 2418–2424.
Goldman D, Urbanek M, Guenther D, Robin R, Long JC. Linkage and association of a functional DRD2 variant [Ser311Cys] and DRD2 markers to alcoholism, substance abuse and schizophrenia in Southwestern American Indians.Am J Med Genet. 1997; 74: 386–394.
Blum K, Chen TJ, Meshkin B, et al. Genotrim™, a DNA-customized nutrigenomic product, targets genetic factors of obesity: hypothesizing a dopamine-glucose correlation demonstrating reward deficiency syndrome (RDS).Med Hypotheses. 2007; 68: 844–852.
Goldman D, Urbanek M, Guenther D, Robin R, Long JC. A functionally deficient DRD2 variant [Ser311Cys] is not linked to alcoholism and substance abuse.Alcohol. 1998; 16: 47–52.
Green AI, Zimmet SV, Strous RD, Schildkraut JJ. Clozapine for comorbid substance use disorder and schizophrenia: do patients with schizophrenia have a reward-deficiency syndrome that can be ameliorated by clozapine?Harv Rev Psychiatry. 1999; 6: 287–296.
Blum K, Briggs AH, Trachtenberg MC, Delallo L, Wallace JE. Enkephalinase inhibition: regulation of ethanol intake in genetically predisposed mice.Alcohol. 1987; 4: 449–456.
Defrance JJ, Hymel C, Trachtenberg MC, et al. Enhancement of attention processing by Kantrol in healthy humans: a pilot study.Clin Electroencephalogr. 1997; 28: 68–75.
Blum K, Trachtenberg MC, Ramsay JC. Improvement of inpatient treatment of the alcoholic as a function of neurotransmitter restoration: a pilot study.Int J Addict. 1988; 23: 991–998.
Blum K, Trachtenberg MC, Elliott CE, et al. Enkephalinase inhibition and precursor amino acid loading improve inpatient treatment of alcohol and polydrug abusers: double-blind placebocontrolled study of the nutritional adjunct SAAVE.Alcohol. 1988; 5: 481–493.
Blum K, Allison D, Trachtenberg MC, et al. Reduction of both drug hunger and withdrawal against advice rate of cocaine abusers in a 30-day inpatient treatment program by the neuronutrient Tropamine.Curr Ther Res. 1988; 43: 1204–1214.
Brown RJ, Blum K, Trachtenberg MC. Neurodynamics of relapse prevention: a neuronutrient approach to outpatient DUI offenders.J Psychoactive Drugs. 1990; 22: 173–187.
Cold JA. NeuRecover-SA in the treatment of cocaine withdrawal and craving: a pilot study.Clin Drug Invest. 1996; 12: 1–7.
Blum K, Briggs AH, Elston SF, DeLallo L, Sheridan PJ, Sar M. Reduced leucine-enkephalin-like immunoreactive substance in hamster basal ganglia after long-term ethanol exposure.Science. 1982; 216: 1425–1427.
Spanagel R, Herz A, Bals-Kubik R, Shippenberg TS. Beta-endorphin-induced locomotor stimulation and reinforcement are associated with an increase in dopamine release in the nucleus accumbens.Psychopharmacology (Berl). 1991; 104: 51–56.
Seizinger BR, Hollt V, Herz A. Effects of chronic ethanol treatment on the in vitro biosynthesis of pro-opiomelanocortin and its posttranslational processing to beta-endorphin in the intermediate lobe of the rat pituitary.J Neurochem. 1984; 43: 607–613.
Hollt V, Haarmann I, Herz A. Long-term treatment of rats with morphine reduces the activity of messenger ribonucleic acid coding for the beta-endorphin/ACTH precursor in the intermediate pituitary.J Neurochem. 1981; 37: 619–626.
Schulz R, Wuster M, Duka T, Herz A. Acute and chronic ethanol treatment changes endorphin levels in brain and pituitary.Psychopharmacology (Berl). 1980; 68: 221–227.
Harrison PA, Hoffman NG.Cator Report: Adult Outpatient Treatment Perspective on Admission and Outcome. St. Paul: St. Paul Ramsey Clinic; 1988.
Simpson DD, Joe GW, Fletcher B, et al. A national evaluation of treatment outcomes for cocaine dependence.Arch Gen Psychiatry. 1999; 56: 507–514.
Blum K, Chen TJH, Downs BW, et al. Synaptamine™ (SG8839): an amino-acid enkephalinase inhibition nutraceutical, improves recovery of alcoholics, a subtype of reward deficiency syndrome (RDS).Trends in Applied Sciences Research. In press.
Blum K, Meshkin B, Downs BW. DNA based customized “gene therapy” utilizing a genoscore: a hypothesized paradigm shift of a novel approach to the diagnosis, stratification, prognosis and treatment of inflammatory processes in the human.Med Hypotheses. 2006; 66: 1008–1018.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, T.J.H., Blum, K., Waite, R.L. et al. Gene Narcotic Attenuation Program attenuates substance use disorder, a clinical subtype of reward deficiency syndrome. Adv Therapy 24, 402–414 (2007). https://doi.org/10.1007/BF02849910
Issue Date:
DOI: https://doi.org/10.1007/BF02849910