Abstract
Purpose: The purpose of this study was to evaluate the clinical effectiveness of subcutaneous estradiol pellets in donor oocyte recipients with an inadequate endometrial response.
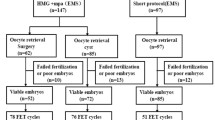
Methods: The subjects were 13 women with ovarian failure and a maximal endometrial thickness <10 mm on standard estrogen regimens, as demonstrated during mock and/or prior oocyte donation cycles. They underwent pellet implantation (100–250 mg of estradiol) 6–13 weeks before oocyte donation.
Results: Maximal (mean ± SD) endometrial thickness was 8.7±1.5 mm on standard regimens, in contrast to 11.7± 1.8 mm on pellets, while estradiol levels were 674±844 and 815±706 pg/ml, respectively. The estradiol:estrone ratio on pellets was >1. There was 1 pregnancy with early loss during 10 cycles on other estrogen regimens and 12 pregnancies during 19 cycles on pellets. The pregnancy and implantation rates were, respectively, 63 and 27% on pellets and 41 and 14% on standard regimens in historical controls.
Conclusions: We conclude that estradiol pellets after a single administration provide constant estradiol levels extending into the first trimester of pregnancy, a physiologic estradiol:estrone ratio, and a better endometrial response than standard estrogen regimens. Implantation and pregnancy rates are higher. This approach may be especially suitable for recipients with a poor endometrial response.
Similar content being viewed by others
References
Trounson A, Leeton JF, Besanko M, Wood C, Conti A: Pregnancy established in an infertile patient after transfer of a dontated embryo fertilized in vitro. Br Med J 1983;286:835–838
Leeton J, Trounson A, Wood C: The use of donor eggs and embryos in the management of human infertility. Aust NZ J Obstet Gynaecol 1984;24:265–270
Rosenwaks Z: Donor eggs: Their application in modern reproductive technologies. Fertil Steril 1987;47:895–909
Sauer MV, Paulson, RJ, Macaso TM, Francis-Hernandez M, Lobo RA: Establishment of a nonanonymous donor oocyte program: preliminary experience at the University of Southern California. Fertil Steril 1989;52:433–436
Kennard EA, Collins RL, Blankstein J, Schover LR, Kanoti G, Reiss J, Quigley MM: A program for matched, anonymous oocyte donation. Fertil Steril 1989;51:655–660
Navot D, Bergh PA, Williams M, Garrisi GJ, Guzman I, Sandler B, Fox J, Schreiner-Engel P, Hofmann GE, Grunfeld L: An insight into early reproductive processes through the in vivo model of ovum donation. J Clin Endocrinol Metab 1991;72:408–414
Flamigni C, Borini A, Violini F, Bianchi L, Serrao L: Oocyte donation: Comparison between recipients from different age groups. Hum Reprod 1993;8:2088–2092
Edwards RG: Why are agonadol and post-amenorrhoeic women so fertile after oocyte donation? Hum Reprod 1992;7:733–734
Asch RH: High pregnancy rates after oocyte and embryo donation. Hum Reprod 1992;7:734
Abdalla HI, Brooks AA, Johnson MR, Kirkland A, Thomas A, Studd JWW: Endometrial thickness: A predictor of implantation in ovum recipients? Hum Reprod 1994;9:363–365
Lutjen P, Trounson A, Leeton J, Findlay J, Wood C, Renou P: The establishment and maintenance of pregnancy using in vitro fertilization and embryo donation in a patient with primary ovarian failure. Nature 1984;307:174–175
Navot D, Laufer N, Kopolovic J, Rabinowitz R, Birkenfeld A, Lewin A, Granat M, Margalioth EJ, Schenker JG: Artificially induced endometrial cycles and establishment of pregnancies in the absence of ovaries. N Engl J Med 1986;314:806–811
Shushan A, Simon A, Reubinoff BE, Lewin A, Schenker JG, Laufer N: The use of vaginal tablets as a vehicle for steroid replacement in a donor oocyte program. Fertil Steril 1994;62:412–414
Feinman M, Sher G, Massaranni G, Vaught L, Andreyko J, Salem R, Zouves C, Dodge S: High fecundity rates in donor oocyte recipients and in-vitro fertilization surrogates using parenteral oestradiol valerate. Hum Reprod 1993;8:1145–1147
Kapetanakis E, Dmowski WP, Auletta F, Scommegna A: Endocrine and clinical effects of estradiol and testosterone pellets used in long-term replacement therapy. Int J Gynaecol Obstet 1982;20:387–399
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dmowski, W.P., Michalowska, J., Rana, N. et al. Subcutaneous estradiol pellets for endometrial preparation in donor oocyte recipients with a poor endometrial response. J Assist Reprod Genet 14, 139–144 (1997). https://doi.org/10.1007/BF02766129
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02766129