Abstract
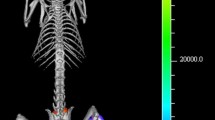
Although in vivo magnetic resonance imaging (MRI) is rapidly becoming a recognised tool in experimental pharmacological research, at the best of our knowledge, scarce application in the field of antibacterial drug research has been reported so far. In this last field, animal models of bacterial infections are used to test the efficacy of novel compounds. In this paper we have explored the potential usefulness of MRI in monitoring the chronological evolution of experimental bacterial infections and the effect of different therapeutic treatments. A murine model of thigh infection induced byStaphylococcus aureus has been used and the efficacy of vancomycin and imipenem/cilastatin has been tested. Three groups of infected animals were studied by microbiology, histology and MRI methods. The results obtained show that in vivo MRI data are highly consistent with microbiological and histological data, allowing, similarly to these commonly used techniques, the efficacy of different antibacterial treatments to be quantified. Our findings suggest that MRI could be used to assess the efficacy of new chemical entities in antibacterial pharmacological research. The advantages of MRI, as a non invasive technique, in comparison with commonly used microbiological and histological methods are discussed.
Similar content being viewed by others
References
Rudin M, Beckmann N, Mir A, Sauter A. In vivo magnetic resonance imaging and spectroscopy in pharmacological research: assessment of morphological, physiological and metabolic effects of drugs. Eur J Pharm Sci 1995;3:255–64.
Rudin M, Briner U, Doepfner W. Quantitative magnetic resonance imaging of estradiol-induced pituitary hyperplasia in rats. Magn Reson Med 1998;7:285–91.
Umemura K, Zierhut W, Rudin M, Novosel D, Robertson E, Pederson B, Hof RP. Effect of Spirapil on left ventricular hypertrophy due to volume overload in rats. J Cardiovasc Pharmacol 1992;19:375–81.
Cook NS, Zerwes HG, Pally C, Rudin M, Hof RP. Spirapril and cilazapril inhibit neointimal lesion development but cause no detectable inhibition of lumen narrowing after carotid artery balloon catheter injury in the rat. Blood Press 1993;2:311–22.
Beckmann N, Bruttel K, Mir A, Rudin M. Noninvasive 3D MR microscopy as a tool in pharmacological research: application to a model of rheumatoid arthritis. Magn Reson Imag 1995;3(7):1013–7.
Minematsu K, Fisher M, Li L, Sotak CH. Diffusion and perfusion magnetic resonance imaging studies to evaluate a non-competitiveN-Methyl-d-Aspartate antagonist and reperfusion in experimental stroke in rats. Stroke 1993;24:2074–81.
Minematsu K, Fisher M, Li L, Davis MA, Knapp AG, Cotter RE, McBurney RN, Sotak CH. Effects of a novel NMDA antagonist on experimental stroke rapidly and quantitatively assessed by diffusion-weighted MRI. Neurology 1993;43:397–403.
Tatlisumak T, Carano RAD, Takano K, Opgenorth TJ, Sotak CH, Fisher M. A novel endothelin antagonist, A-127722, attenuates ischemic lesion size in rats with temporary middle cerebral artery occlusion-A diffusion and perfusion study. Stroke 1998;29:850–8.
Acred P, The Selbie or Thigh Lesion Tests, Experimental Models in Antimicrobial Chemotherapy, vol. I. London: Academic Press, 1986.
Eng RH, Cherubin CE, Smith SM, Buccini F, Harris R. In-vitro and in-vivo activity of cefpirone (HR 810) against methicillin-susceptible and-resistantStaphylococcus aureus andStreptococcus faecalis. J Antimicrob Chemoth 1989;23:373–81.
Shirkhoda A, Ali-Reza A, Bis KG, Makris J, Irwin RB, Shetty AN. MR Imaging of myositis ossificans: variable patterns at different stages. J Magn Reson Imag 1995;5:287–92.
National Committee for Clinical Laboratory Standard. Methods for dilution anti-microbial susceptibility tests for bacteria that grow aerobically. 4th ed. Villanova, Pa: Approved Standard M7-A4. National Committee of Clinical Laboratory Standards, 1997.
Marzola P, Da Pra A, Sbarbati A, Osculati F. A PC-based workstation for processing and analysis of MRI data, MAG*MA. in press.
Craig WA. Interrelationship between pharmacokinetics and pharmacodinamics in determing dose regimens for broad spectrum cephalosporins. Diagn Microbiol Inf Dis 1995;22:89–96.
Selbie FR, O'Grady F: A measurable tubercolous lesion in the thigh of the mouse. Br J Exp Pathol 1954;35:556–65.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marzola, P., Nicolato, E., Di Modugno, E. et al. Comparison between MRI, microbiology and histology in evaluation of antibiotics in a murine model of thigh infection. MAGMA 9, 21–28 (1999). https://doi.org/10.1007/BF02634589
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02634589