Objective
To assess current practices and attitudes toward teaching humanistic and psychosocial aspects of care in internal medicine residency programs.
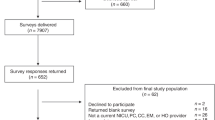
Design and participants: Survey questionnaires were sent to residency directors at all 434 internal medicine residency programs accredited in 1985–1986. Response rate for two mailings was 71%.
Measurements and main results: 78% of residency directors and 70% of department chairpersons bad high or moderately high levels of commitment to teaching bumanistic/psychosocial aspects of care, but only 44% of responding programs offered mandatory training, and only 18% offered elective training in these areas. Obstacles to expanded teaching of the bumanistic/psychosocial aspects rated high or moderately high by residency directors included insufficient curriculum time (51%), lack of trained faculty (44%), and pressures to reduce both training costs (40%) and patient-care costs (37%).
Conclusions: Most of the training that does occur in the humanistic/psychosocial aspects of care probably happens informally via mentoring and role modeling. Appeals to expand teaching in these areas raise questions regarding what to include in medical training and the proper scope of internal medicine. Sustainable change will depend on the politics of resource distribution and the influence of general internal medicine and primary care on traditional training.
Similar content being viewed by others
References
Bok D. Needed: a new way to train doctors. Harvard Magazine, 1984; May-June: 32–43, 70–1.
Culliton BJ. Medical education under fire. Science. 1984;236:419–20.
Engel GL. The biopsychosocial model and the education of health professionals. Ann N Y Acad Sci. 1978;310:169–81.
Karpf M, Levey GS. Divisions of general internal medicine: accomplishments and needs. Ann Intern Med. 1985;103:456–7.
Regier DA, Goldberg ID, Taube CA. The de facto U.S. mental health services system. Arch Gen Psychiatry. 1978;35:685–93.
Thompson TL. Psychiatry in primary care medicine. In: Cavenar J, ed. Psychiatry. Vol. 2. Philadelphia: J.B. Lippincott Co., 1985:1–10.
Thompson TL, Thomas MR. Teaching psychiatry to primary care internists. Gen Hosp Psychiatry. 1985;7:210–3.
Bird J, Cohen-Cole SA, Boker J, Freeman A. Teaching psychiatry to non-psychiatrists I: the application of educational methodology. Gen Hosp Psychiatry. 1983;5:247–53.
Cohen-Cole SA, Boker J, Bird J, Freeman A. Psychiatric education for primary care: a pilot study of needs of residents. J Med Educ. 1982;57:931–6.
Houpt JL, Orleans CS, George LK, Brodie KH. The role of psychiatric and behavioral factors in the practice of medicine. Am J Psychiatry. 1980;137:37–47.
Smith GR, Monson RA, Ray DC. Psychiatric consultation in somatization disorder: a randomized controlled study. N Engl J Med. 1986;314:1407–13.
Cummings NA, VandenBos GR. The twenty year Kaiser Permanente experience with psychotherapy and medical utilization. Health Policy Q. 1981;2:150–74.
Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36.
Cavanaugh SV, Kennedy S. A successful psychiatric training program for medical residents. Gen Hosp Psychiatry. 1986;8:73–9.
Cohen-Cole SA, Bird J. Teaching psychiatry to nonpsychiatrists II: a model curriculum. Gen Hosp Psychiatry. 1984;6:1–11.
Brown JT, Harris RT. The medical psychiatric unit and psychosocial education of internists. Psychosomatics. 1985;26:231–8.
Koran LM, Barnes LA. The Stanford comprehensive medical unit: integrating psychiatric and medical care. In: Kuldau J, ed. New directions for mental health services: treatment for psychosomatic problems. San Francisco: Jossey-Bass, 1982:61–73.
Fink PJ. Psychiatry and primary care: can a working relationship develop? Gen Hosp Psychiatry. 1985;7:205–9.
Duffy DL, Hamerman D, Cohen MA. Communication skills of house officers. Ann Intern Med. 1980;93:354–7.
Friedman RH, Pozen JT. The academic viability of general internal medicine. Ann Intern Med. 1985;103:439–44.
Eisenberg JM. The internist as gatekeeper. Ann Intern Med. 1985;102:537–43.
Strain JJ, Pincus HA, Gise LH, Houpt J. Mental health education in three primary care specialties. J Med Educ. 1986;61:958–66.
Bennett SE, Goodson JD, Izen JE, et al. Comparing ambulatory care practices of primary care and traditional medicine residents. Med Care. 1985;23:816–22.
Daley J, Harrington JT. The characteristics of training in ambulatory medicine in U.S. residents. J Med Educ. 1985;60:355–66.
Committee on Evaluation in General Internal Medicine, American Board of Internal Medicine. Clinical competence in internal medicine. Ann Intern Med. 1979;90:402–11.
Subcommittee on Evaluation of Humanistic Qualities in the Internist, American Board of Internal Medicine. Evaluation of humanistic qualities in the internist. Ann Intern Med. 1983;99:720–4.
American Medical Association. Directory of residency training programs. Chicago: 1985.
Linn LS, Brook RH, Clark VA, Fink A, Kosecoff J. Evaluation of ambulatory care training by graduates of internal medicine residencies. J Med Educ. 1986;61:293–302.
Perkoff G. Teaching clinical medicine in the ambulatory setting. N Engl J Med. 1986;314:27–31.
Basson MD. How can we train doctors to be more humanistic? In: Basson MD, ed. Progress in clinical and biological research, Vol. 38: ethics, humanism and medicine. New York: Alan R. Liss, Inc., 1980;67–8.
Mattews DA, Voytovich AE. An appraisal of goals for residency training in internal medicine. J Med Educ. 1985;60:536–44.
Doran GA. Scientism vs. humanism in medical education. Soc Sci Med. 1983;17:1831–5.
Kosecoff J, Fink A, Brook RH, et al. General medical care and the education of internists in university hospitals: an evaluation of the teaching hospital general medicine group practice program. Ann Intern Med. 1985;102:250–7.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Merkel, W.T., Margolis, R.B. & Smith, R.C. Teaching humanistic and psychosocial aspects of care. J Gen Intern Med 5, 34–41 (1990). https://doi.org/10.1007/BF02602307
Issue Date:
DOI: https://doi.org/10.1007/BF02602307