Abstract
OBJECTIVE: To describe the association between hospital resource utilization and physicians’ knowledge of patient preferences for cardiopulmonary resuscitation (CPR) among seriously ill hospitalized adult patients.
DESIGN: Prospective cohort study.
SETTING: Five U.S. academic medical centers, 1989–1991.
PATIENTS: A sample of 2,636 patients with self- or surrogate interviews and matching physician interviews describing patient preferences for CPR, from a cohort of 4,301 patients with life-threatening illnesses enrolled in the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT).
MEASURES: Patient, surrogate, and physician reports of preferences for resuscitation, and resource use derived from the Therapeutic Intensity Scoring System and hospital length of stay, converted into 1990 dollars.
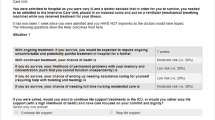
RESULTS: Nearly one-third of the patients preferred to forge resuscitation. Of the 2,636 paired physician—patient answers, nearly one-third did not agree about preferences for resuscitation. The physicians’ views of the patients’ preferences and those preferences themselves were both associated with resource use. Standardized adjusted hospital resource consumption, expressed as average cost in dollars during the enrollment hospitalization, was lowest when the physician agreed with the patient preference for a do-not-resuscitate order ($20,527), and highest when the patient did not have a preference and the physician believed the patient wanted resuscitation in the case of a cardiopulmonary arrest ($34,829) Hospital resource use was intermediate when patient—physician pairs evidenced either lack of agreement or communication, or awareness of options about resuscitation.
CONCLUSIONS: Both physician and patient preferences for CPR influence total hospital resource consumption. Physician misunderstanding of patient preferences to forgo CPR was associated with increased use of hospital resources, and could have led to a course of care at odds with patients’ expressed preferences in the event of cardiac arrest. Increasing physicians’ knowledge of patient preferences, and increasing communication to help patients understand that options foi medical care that include forgoing resuscitation efforts, might reduce hospital expenditures for the seriously ill.
Similar content being viewed by others
References
Presidents Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to forego life-sustaining treatment. Washington, DC: U.S. Government Printing Office, 1983.
The Hastings Center. Guidelines on the termination of life-sustaining treatment and the care of the dying. Bloomington, IN: Indiana University Press, 1987.
The Coordinating Council on Life-Sustaining Medical Treatment Decisions by the Court. Guidelines for state court decision making in authorizing or withholding life-sustaining medical treatment: a project of the national center for state courts. Williamsburg, VA: West Publishing Company, 1991.
Bedell SE, Delbanco TL. Choices about cardiopulmonary resuscitation in the hospital: when do physicians talk with patients? N Engl J Med. 1984;310:1089–93.
Bedell SE, Pelle D, Maher PL, Cleary PD. Do-not-resuscitate orders for critically ill patients in the hospital: how are they used and what is their impact? JAMA. 1986;256:233–7.
Lynn J, Teno J, Wenger N, et al. “Do not resuscitate orders” in seriously ill patients: expressed preferences or last rites [abstract]. Clin Res. 1992;40(2):347a.
Teno JM, Mor V, Fleishman J. Preferences of HIV-infected patients for aggressive versus palliative care [letter]. N Engl J Med. 1991;324:1140.
Uhlmann RF, Pearlman RA, Cain KC. Physicians’ and spouses’ predictions of elderly patients’ resuscitation preferences. J Gerontol. 1988;43:M115–21.
Seckler AB, Meier DE, Mulvihill M, Cammer Paris BE. Substituted judgment: how accurate are proxy predictions? Ann Intern Med. 1991;115:92–8.
Lynn J, Knaus WA. Background for SUPPORT. J Clin Epidemiol. 1990;43(suppl):1s-4s.
Murphy DJ, Knaus WA, Lynn J. Study population in SUPPORT: patients (as defined by disease categories and mortality projections), surrogates, and physicians. J Clin Epidemiol. 1990;43(suppl):11s-22s.
Knaus WA, Wagner DP. Draper AE, et al. APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–36.
Keene AR, Cullen DJ. Therapeutic intervention scoring system: update 1983. Crit Care Med. 1983;11:1–5.
Oye RK. Landefeld CS, Jaye RL. Outcomes in SUPPORT. J Clin Epidemiol. 1990:43(suppl)L83s-87s.
Carlson RW, Devich L, Frank RR. Development of a comprehensive supportive care team for the hopelessly ill on a university hospital medical service. JAMA. 1988;259:378–83.
Chambers CV, Diamond JJ, Perkel RL, Lasch LA. Relationship of advance directives to hospital charges in a Medicare population. Arch Intern Med. 1994;154:541–7.
Schneiderman LJ, Kronick R, Kaplan RM, Anderson JP, Langer RD. Effects of offering advance directives on medical treatments and costs. Ann Intern Med. 1992;117:599–606.
Teno J, Lynn J, Phillips RS, et al., for the SUPPORT Investigators. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? J Clin Ethics. 1994;5(1):23–30.
Murphy DJ, Murray AM, Robinson BE, Campion EW. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Intern Med. 1989;111:199–205.
George AL, Folk BP, Crecelius PL, Campbell WB. Pre-arrest morbidity and other correlates of survival after in-hospital cardiopulmonary arrest. Ann J Med. 1989;87:28–34.
Cohn EB, Lefevre F, Yarnold PR, Aaron MJ, Martin GJ. Predicting survival from in-hospital CPR: meta-analysis and validation of a prediction model. J Gen Intern Med. 1993;8:347–53.
Taffet GE, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. JAMA. 1988;260:2069–72.
Burns R, Graney MJ, Nichols LO. Prediction of in-hospital cardiopulmonary arrest. Arch Intern Med. 1989;149:1318–21.
Bedell SE, Delbanco TL, Cook EF, Epstein FH. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med. 1983;309:569–76.
Callahan D. Setting Limits: Medical Goals in an Aging Society. New York: Simon and Schuster, 1987.
Niemann JT. Cardiopulmonary resuscitation. N Engl J Med. 1992;327:1075–80.
Wennberg JE. Outcomes research, cost containment, and the fear of health care rationing. N Engl J Med. 1990;323:1202–4.
Singer PA, Lowy FH. Rationing, patient preferences, and cost of care at the end of life. Arch Intern Med. 1992;152:478–9.
Teno JM. Lynn J. Phillips RS, et al. Federal interventions regarding end of life decision making: lessons from the PSDA [abstract]. J Gen Intern Med. 1994;9(Apr suppl 2):99.
Author information
Authors and Affiliations
Consortia
Additional information
Supported by The Robert Wood Johnson Foundation’s Program on the Care of Critically-Ill Hospitalized Adults: SUPPORT—The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. The opinions and findings in this article are those of the authors and do not necessarily represent the views of the sponsors.
Rights and permissions
About this article
Cite this article
Teno, J.M., Hakim, R.B., Knaus, W.A. et al. Preferences for cardiopulmonary resuscitation. J Gen Intern Med 10, 179–186 (1995). https://doi.org/10.1007/BF02600252
Issue Date:
DOI: https://doi.org/10.1007/BF02600252