Abstract
OBJECTIVES: To identify strategies involved in the diagnosis and treatment plans of primary care problems that are uncertain and complex.
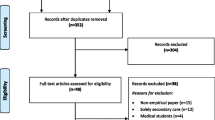
METHODS: In this exploratory study we observed primary care physicians encountering standardized patients who portrayed typical primary care problems involving uncertainty and complexity. First, we analyzed 10 tapes of nine physicians with a range of clinical experience (first-year residents through faculty physicians) interacting with four standardized patient cases (headache, back pain, hypertension, and abdominal pain). We analyzed the 10 tapes to determine the regular occurrence of physician behavior patterns that we later described as strategies. Then, using a written questionnaire, 19 general internal medicine faculty physicians from our hospital and from an affiliated hospital rated the perceived importance of these strategies for clinical practice in general. Finally, we checked the incidence of the strategies: (1) across a range of six cases (headache, back pain, hypertension, abdominal pain, fatigue, and well-adult care) using six first-year residents (a total of 19 encounters), and (2) across different levels of clinical experience using the standardized patient case of headache involving eight physicians (first-year residents through faculty physicians).
RESULTS: Nine strategies were identified, and each was rated as important to primary care clinical practice. The strategies were: (1) defines the context of the diagnosis and explains the signs and symptoms as part of the expected spectrum of the disease; (2) eliminates alternative diagnoses by dealing with patient fears, giving reasons in the context of the patient’s belief system; (3) describes the prognosis in terms of the likely course of the disease and expectations of treatment; (4) negotiates key problems or issues that are important to both patient and physician; (5) negotiates the plan and ensures patient understands, and is willing and able to comply, given his/her particular context; (6) keeps diagnostic options open by making provisional diagnoses while keeping alternatives in mind; (7) is circumspect and takes action to minimize the possibility of missing other critical diagnoses; (8) plays for time by allowing signs and symptoms to develop to help clarify the diagnosis; and (9) plans for contingencies by providing appropriate if/then statements concerning situations requiring further action. The strategies were used in each of the six cases, and by physicians with all levels of clinical experience.
CONCLUSIONS: The nine strategies led to the generation of a construct we termed “strategic medical management,” which refers to the management (diagnosis and proposed treatment) of uncertain and complex medical problems in primary care. The construct provides a more elaborated framework in which to view clinical decision making and integrates recent ideas concerning doctor-patient communication into this process. Strategic medical management appears to be based on tacit knowledge that is seldom explicity articulated or taught. It has potential implications for enhancing instruction and assessment in medical education.
Similar content being viewed by others
References
Mathers N, Hodgkin P. The gatekeeper and the wizard: a fairy tale. BMJ. 1989;298:172–3.
Kahneman DL, Slovic P, Tversky A, eds. Judgment Under Uncertainty: Heuristics and Biases. New York, NY: Cambridge University Press; 1982.
Neufeld VR, Norman GR, eds. Assessing Clinical Competence. New York. NY: Springer Publishing Co: 1985.
Kassirer JP, Gorry GA. Clinical problem solving: a behavioral analysis. Ann Intern Med. 1978;89:245–55.
Nardone DA. Johnson GJ, Faryna A, Coulehan JL, Parrino TA. A model for the diagnostic medical interview: nonverbal, verbal, and cognitive assessments. J Gen Intern Med. 1992;7:437–42.
Day RP. Hewson MG, Kindy P, Van Kirk J. Evaluation of resident performance in an outpatient internal medicine clinic using standardized patients. J Gen Intern Med. 1993;8:193–8.
Schmidt HG. Norman GR, Boshuizen HPA. A cognitive perspective on medical expertise: theory and implications. Acad Med. 1990;65:611–21.
Shulman LS. The wisdom of practice: managing complexity in medicine and teaching. In: Berliner DC, Rosenshine B, eds. Talks for Teachers: A Festschrift for N Gage. New York, NY: Random House: 1987.
Steinberg RJ, Wagner RK. Individual differences in practical knowledge and its acquisition. In: Ackerman PL, Sternberg R, Glaser R, eds. Learning and Individual Differences. New York, NY: WW Freeman and Co; 1989.
Schon D. The Reflective Practitioner: How Professionals Think in Action. New York, NY: Basic Books; 1983.
Schon DA. Educating the Reflective Practitioner: Toward a New Design of Teaching and Learning in the Professions. San Francisco, Calif: Jossey-Bass Publishers; 1987.
Crabtree BE, Miller WL, eds. Doing Qualitative Research: Research Methods for Primary Care. Beverly Hills, Calif: Sage Publishers; 1992:3.
Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, Calif: Sage Publishers: 1985.
Kleinman A. The Illness Narratives: Suffering, Healing, and the Human Condition. New York, NY: Basic Books; 1988.
Waitzkin H. The Politics of Medical Encounters: How Patients and Doctors Deal with Social Problems. New Haven. Conn: Yale University Press; 1991.
Latham PM. Reflections. J Gen Intern Med. 1994;9:44.
Author information
Authors and Affiliations
Additional information
Received from the Department of Medicine, University of Wisconsin, Madison.
Supported by the U.S. Department of Health and Human Services residency training grant D29-PE-15218.
Rights and permissions
About this article
Cite this article
Hewson, M.G., Kindy, P.J., Van Kirk, J. et al. Strategies for managing uncertainty and complexity. J Gen Intern Med 11, 481–485 (1996). https://doi.org/10.1007/BF02599044
Issue Date:
DOI: https://doi.org/10.1007/BF02599044