Abstract
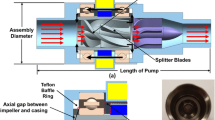
Thrombus formation and hemolysis are critical issues in the design of a long-term implantable LVAS (left ventricular assist system). The fluid dynamic characteristics of the blood flow are one of the main factors that cause thrombus formation and hemolysis. In this study, we optimized blood chamber geometry, port design, and fluid dynamics in our implantable LVAS to ensure minimization of shear-stress-related blood damage. A blood pump chamber (stroke volume, 65 ml) and an inflow and outflow port were designed with three-dimensional CAD (computer-aided-design) software (Pro-Engineering version 20) and estimated by FEM (fine-element method) computational fluid dynamic (CFD) analysis (Ansys version 5.5). We adopted three-dimensional distribution of CFD results for qualitative evaluation, and we also tried to estimate the normalized index of hemolysis (NIH) and time-series change of hematocrit from the results of CFD analysis as quantitative index of optimization for geometry of the blood pump chamber. With the use of this design, the blood pump geometry was optimized as the decrease of NIH from 2.72 g/1001 in the first model to 0.098 g/1001 in the second model, corresponding to the decrease in shear stress. The hematocrit also improved from 0.7% in the first model to 11.5% in the second model 2 years after implantation of the pump. Areas where flow stagnation was observed in the first model were free of stagnation in the second model. The results show that computer-aided design of the blood pump contributes to optimizing a blood pump chamber for reducing thrombus formation and hemolysis, and also contributes to reducing cost and time in developing the implantable LVAS.
Similar content being viewed by others
References
Okamoto E, Tomoda K, Yamamoto K, Mitamura Y, Mikami T. Development of a compact, highly efficient totally implantable motor-driven assist pump system. Artif Organs 1994;18:911–917
Okamoto S. Fluid dynamic. Tokyo: Morikita Publisher, 1996 (in Japanese)
Giersiepen M, Wurzinger LJ, Opitz R, Reul H. Estimation of shear stress-related blood damage in heart valve prostheses—in vitro comparison of 25 aortic valves. Int J Artif Organs 1990;13:300–306
Naito K, Mizuguchi K, Nose Y. The need for standardizing the index of hemolysis. Artif Organs 1994;18:7–10
Okamoto E, Shimanaka M, Suzuki S, Baba K, Mitamura Y. Remote monitoring system of patients with implantable VADs with personal handy-phone system (PHS). ASAIO J 1999;45:194–198
Mussivand T, Hum A, Holmes KS, Hendry PJ, Masters RG, Keon WJ. Remote monitoring of patients with implantable VADs using cellular technology. ASAIO J 1997;43:85
Woodard JC, Shaffer FD, Schaub RD, Lund LW, Borovetz HS. Optimal management of a ventricular assist system—contribution of flow visualization studies. J Am Soc Artif Intern Organs 1992;38:216–219
Meier D, Wernicke J-T, Orime Y, Takatani S, Tasai K, Damm G, Naito K, Mizuguchi K, Makinouchi K, Glueck J, Shimono T, Matsuda Y, Ohara Y, Kojima R, Noon GP, Debakey ME, Nose Y. Flow pattern analysis of the Baylor Total Artificial Heart. Artif Organs 1994;18:923–932
Mussivand T, Day KD, Naber BC. Fluid dynamic optimizations of a ventricular assist device using particle image velocimetry. J Am Soc Artif Intern Organs 1999;45:25–31
Okamoto E, Shimanaka M, Suzuki S, Baba K, Mitamura Y. Remote monitoring system of patients with implantable VADs with personal handy-phone system (PHS). Am Soc Intern Artif Organs 1999;45:194–198
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okamoto, E., Fukuoka, Si., Iwazawa, E. et al. Computer assisted design for the implantable left ventricular assist device (LVAD) blood pump using computational fluid dynamics (CFD) and computer-aided design and manufacturing (CAD/CAM). J Artif Organs 4, 205–213 (2001). https://doi.org/10.1007/BF02479895
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02479895