Abstract
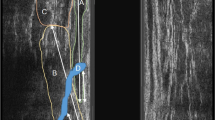
PURPOSE: Traumatic sphincter disruption frequently is associated with a rectovaginal fistula, but the effect of a persistent sphincter defect on the outcome of rectovaginal fistula repair is poorly documented. We analyzed the outcome of rectovaginal fistula repairs based on preoperative sphincter status. PATIENTS AND METHODS: We identified 52 women who underwent 62 repairs of simple obstetrical rectovaginal fistulas between 1992 and 1995. Fourteen patients (27 percent) had preoperative endoanal ultrasound studies and 25 (48 percent) had anal manometry studies. Follow-up was by mailed questionnaire in 36 patients (69 percent) and by telephone interview in 12 (23 percent), for a total response rate of 92 percent. Median age was 30.5 (range, 18–70) years, and median follow-up was 15 (range, 0.5–123) months. Twenty-five patients (48 percent) complained of varying degrees of fecal incontinence before surgery. There were 27 endorectal advancement flaps and 35 sphincteroplasties (28 with and 8 without levatoroplasty). RESULTS: Success rates were 41 percent with endorectal advancement flaps and 80 percent with sphincteroplasties (96 percent success with and 33 percent without levatoroplasty;P=0.0001). Endorectal advancement flap was successful in 50 percent of patients with normal sphincter function but in only 33 percent of patients with abnormal sphincter function(P=not significant). For sphincteroplasties, success rates were 73vs. 84 percent for normal and abnormal sphincter function, respectively (P=not significant). Results were better after sphincteroplastiesvs. endorectal advancement flaps in patients with sphincter defects identified by endoanal ultrasound (88vs. 33 percent;P=not significant) and by manometry (86vs. 33 percent;P = not significant). Poor results correlated with prior surgery in patients undergoing endorectal advancement flaps (45 percentvs. 25 percent;P = not significant) but not sphincteroplasties (80vs. 75 percent;P = not significant). CONCLUSIONS: All patients with rectovaginal fistula should undergo preoperative evaluation for occult sphincter defects by endoanal ultrasound or anal manometry or both procedures. Local tissues are inadequate for endorectal advancement flap repairs in patients with sphincter defects and a history of previous repairs. Patients with clinical or anatomic sphincter defects should be treated by sphincteroplasty with levatoroplasty.
Similar content being viewed by others
References
Venkatesh KS, Ramanujam PS, Larson DM, Haywood MA. Anorectal complications of vaginal delivery. Dis Colon Rectum 1989;32:1039–41.
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med 1993;329:1905–11.
Leigh RJ, Turnberg LA. Fecal incontinence: the unvoiced symptom. Lancet 1982;1:1349–51.
Lowry AC, Thorson AG, Rothenberger DA, Goldberg SM. Repair of simple rectovaginal fistulas: influence of previous repairs. Dis Colon Rectum 1988;31:676–8.
Rothenberger DA, Christenson CE, Balcos EG,et al. Endorectal advancement flap for treatment of simple rectovaginal fistula. Dis Colon Rectum 1982;25:297–300.
Rothenberger DA. Anal incontinence. In: Cameron JL, ed. Current surgical therapy. Toronto: BC Decker, 1989.
McRae HM, McLeod RS, Cohen Z, Stern H, and Reznick R. Treatment of rectovaginal fistulas that has failed previous repair attempts. Dis Colon Rectum, 1995;38:921–5.
Goligher JC. Surgery of the anus, rectum and colon. 5th ed. London: Bailliere Tindall, 1984.
Senatore PJ. Anovaginal fistulae. Surg Clin North Am 1994;74:1361–75.
Khanduja KS, Yamashita HJ, Wise WE Jr, Aguilar PS, Hartmann RF. Delayed repair of obstetric injuries of the anorectum and vagina: a stratified surgical approach. Dis Colon Rectum 1994;37:344–9.
Belt RL Jr, Belt RL. Repair of anorectal vaginal fistula utilizing segmental advancement of the internal sphincter muscle. Dis Colon Rectum 1969;12:99–104.
Mengert WF, Fish SA. Anterior rectal wall advancement: technique for repair of complete perineal laceration and rectovaginal fistula. Obstet Gynecol 1955;5:262–7.
Russell TR, Gallagher DM. Low rectovaginal fistulas. Approach and treatment. Am J Surg 1977;134:13–8.
Hilsabeck JR. Transanal advancement of the anterior rectal wall for vaginal fistulas involving the lower rectum. Dis Colon Rectum 1980;23:236–41.
Hoexter B, Labow SB, Moseson MD. Transanal rectovaginal fistula repair. Dis Colon Rectum 1985;28:572–5.
Jones IT, Fazio VW, Jagelman DG. The use of transanal rectal advancement flaps in the management of fistulas involving the anorectum. Dis Colon Rectum 1987;30:919–23.
Wise WE Jr, Aguilar PS, Padmanabhan A, Meesig DM, Arnold MW, Stewart WR. Surgical treatment of low rectovaginal fistulas. Dis Colon Rectum 1991;34:271–4.
Kodner IJ, Mazor A, Shemesh EI, Fry RD, Fleshman JW, Birnbaum EH. Endorectal advancement flap repair of rectovaginal and other complicated anorectal fistulas. Surgery 1993;114:682–9; discussion 6:89–90.
Mazier WP, Senagore AJ, Schiesel EC. Operative repair of anovaginal and rectovaginal fistulas. Dis Colon Rectum 1995;38:4–6.
Watson SJ, Phillips RK. Non-inflammatory rectovaginal fistula. Br J Surg 1995;82:1641–3.
Athanasiadis S, Oladeinde I, Kuprian A, Keller B. Endorectal advancement flap-plastyvs. transperineal closure in surgical treatment of rectovaginal fistula: a prospective long-term study of 88 patients. Chirurg 1995;66:493–502.
Author information
Authors and Affiliations
Additional information
Read at the Minnesota Surgical Society, May 3, 1996, at the meeting of The American Society of Colon and Rectal Surgeons, Seattle, Washington, June 9 to 14, 1996, and at the Tripartite Meeting, July 8 to 10, 1996.
About this article
Cite this article
Tsang, C.B.S., Madoff, R.D., Wong, W.D. et al. Anal sphincter integrity and function influences outcome in rectovaginal fistula repair. Dis Colon Rectum 41, 1141–1146 (1998). https://doi.org/10.1007/BF02239436
Issue Date:
DOI: https://doi.org/10.1007/BF02239436