Abstract
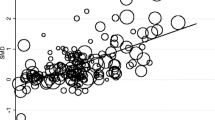
Cerebrospinal fluid 5-hydroxyindoleacetic acid (CSF 5-HIAA) was determined for elderly delirious patients during the acute stage and after a 1-year follow-up period, and the 5-HIAA levels were compared with age-equivalent controls. As compared with the controls, the 5-HIAA levels were significantly higher at the beginning of the index admission in patients with multi-infarct dementia and patients with no apparent CNS disease. The 5-HIAA levels were also higher in the latter subgroup in the 1-year sampling, but no other differences between delirious patients and controls were observed. The one-way procedure showed no differences between the subgroup means of delirious patients when divided according to the severity of cognitive decline or type of delirium in any of the samples. The 5-HIAA levels measured during the index admission correlated with the length of life after delirium suggesting that serotonergic dysfunction may have prognostic significance in delirious patients.
Similar content being viewed by others
References
American Psychiatric Association (1980) Diagnostic and statistical manual of mental disorders (3 rd ed.). APA: Washington, DC
Banks CM, Vojnik M (1978) Comparative simultaneous measurement of cerebrospinal fluid 5-hydroxyindoleacetic acid and blood serotonin levels in delirium tremens and clozapine-induced delirious reaction. J Neurol Neurosurg Psychiatry 41:420–424
Coccaro EF (1989) Central serotonin and impulsive aggression. Br J Psychiatry 155 [Suppl 8]:52–62
Duara R, Grady C, Haxby J, Sundaram M, Cutler NR, Heston L, Moore A, Schlageter N, Larson S, Rapoport SI (1986) Positron emission tomography in Alzheimer's disease. Neurology 36:879–887
Ferrarese C, Bassi S, Frattola L, Locatelli P, Piolti R, Trabucchi M (1986) Different patterns of CSF neurotransmitter metabolism in patients with left or right hemispheric stroke. Acta Neurol Scand 3:581–585
Folstein MF, Folstein SE, McHugh PR (1975) MlsMini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Gibson GE, Blass JP, Huang H-M, Freeman GB (1991) The cellular basis of delirium and its relevance to age-related disorders inculding Alzheimer's disease. Int Psychogeriatrics 2:373–395
Hoehn MM, Yahr MD (1967) Parkonsonism: onset, progression, and mortality. Neurology 17:427–442
Jolkkonen J, Lehtinen M, Soininen H, Sennef C, Riekkinen P (1987) Enhanced monoaminergic neurotransmission by desglycinamide-arginine-vasopressin in human subjects. Neurosci Lett 76:312–315
Koponen H, Riekkinen PJ (1993) A prospective study of delirium in elderly patients admitted to a psychiatric hospital. Psychol Med 23:103–109
Levkoff SE, Evans DA, Liptzin B, Cleary PD, Lipsitz LA, Wetle TT, Reilly CH, Pilgrim DM, Schor J, Rowe J (1992) Delirium. The occurrence and persistence of symptoms among elderly hospitalized patients. Arch Intern Med 152:334–340
Lindesay J, Macdonald A, Starke I (1990) Delirium in the elderly. Oxford University Press, Oxford
Lipowski ZJ (1980) Delirium: Acute brain failure in man. Charles C. Thomas, Springfield
Lipowski ZJ (1983) Transient cognitive disorders (delirium, acute confusional states) in the elderly. Am J Psychiatry 140:1426–1436
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer's disease. Neurology 34:939–944
Mesulam M-M (1986) Principles of behavioral neurology. F. A. Davis Company, Philadelphia
van Praag HM, de Haan S (1979) Central serotonin metabolism and frequency of depression. Psychiatry Press 1:219–224
Reinikainen KJ, Paljärvi L, Huuskonen M, Soininen H, Laakso M, Riekkinen PJ (1988) A post-mortem study of noradrenergic, serotonergic and GABAergic neurons in Alzheimer's disease. J Neurol Sci 84:101–116
Seeldrayers P, Messina D, Desmedt D, Dalesio O, Hildebrand J (1985) CSF levels of neurotransmitters in Alzheimer-type dementia. Effects of ergoloid mesylate. Acta Neurol Scand 71:411–414
Soininen H, McDonald E, Rekonen M, Riekkinen PJ (1981) Homovanillic acid and 5-hydroxyindoleacetic acid levels in cerebrospinal fluid of patients with senile dementia of Alzheimer type. Acta Neurol Scand 64:101–107
Trzepacz PT, Teague GB, Lipowski ZJ (1985) Delirium and other organic mental disorders in a general hospital. Gen Hosp Psychiatry 7:101–106
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Koponen, H.J., Lepola, U. & Leinonen, E. A long-term follow-up study of cerebrospinal fluid 5-hydroxyindoleacetic acid in delirium. Eur Arch Psychiatry Clin Nuerosci 244, 131–134 (1994). https://doi.org/10.1007/BF02191886
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02191886