Abstract
Major thermal injury is associated with extreme hypermetabolism and catabolism as the principal metabolic manifestations encountered following successful resuscitation from the shock phase of the burn injury. Substrate and hormonal measurements, indirect calorimetry, and nitrogen balance are biochemical metabolic parameters which are useful and more readily available biochemical parameters worthy of serial assessment for the metabolic management of burn patients. However, the application of stable isotopes with gas chromatography/mass spectroscopy and more recently, new immunoassays for growth factors and cytokines has increased our understanding of the metabolic manifestations of severe trauma.
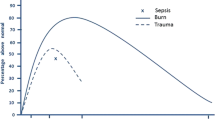
The metabolic response to injury in burn patients is biphasic wherein the initialebb phase is followed by a hypermetabolic and catabolicflow phase of injury. The increased oxygen consumption/metabolic rate is in part fuelled by evaporative heat loss from wounds of trauma victims, but likely also by a direct central effect of inflammation upon the hypothalamus. Although carbohydrates in the form of glucose appear to be an important fuel source following injury, a maximum of 5–6 mg/kg/min only is beneficial. Burn patients have accelerated gluconeogenesis, glucose oxidation, and plasma clearance of glucose. Additionally, considerable futile cycling of carbohydrate intermediates occurs which includes anaerobic lactate metabolism and Cori cycle activity arising from wound metabolism of glucose and other substrates. Similarly, accelerated lipolysis and futile fatty acid cycling occurs following burn injury. However, recent evidence suggests that lipids in the diet of burned and other injured patients serve not only as an energy source, but also as an important immunomodulator of prostaglandin metabolism and other immune responses.
Amino acid metabolism in burn patients is characterized by increased oxidation, urea synthesis, and protein breakdown which is prolonged and difficult to reduce with current nutritional therapy. However, the current goal of nutritional support is to optimize protein synthesis. Specific unique requirements may exist for supplemental glutamine and arginine following burn injury but further research is needed before enhanced branched chain amino acids supplements can be recommended for burn patients. Recent research investigations have revealed the importance of enteral feeding to enhance mucosal defense against gut bacteria and endotoxin. Similarly, research has demonstrated that many of the metabolic perturbations of burns and sepsis may be due, at least in part, to inflammatory cytokines. Investigation of their pathogenesis and mechanism of action both at a tissue and a cellular level offer important prospects for improved understanding and therapeutic control of the metabolic disorders of burn patients.
Résumé
Après récupération de la première phase de choc survient un hypercatabolisme majeur. Des paramètres de surveillance de l'évolution et d'évaluation de l'efficacité du traitement sont facilement disponibles: dosages hormonaux et de différents subtats, calorimétrie indirecte et bilan azoté devraient être dosés de façon régulière chez les brûlés. Notre compréhension des perturbations métaboliques chez le blessé et chez la grand brûlé s'est améliorée ces dernières années en raison de l'application de techniques isotopiques avec des dosages par la chromatographie gazeuse et la spectrophotométrie de masse et plus récemment encore les dosages immunologiques des facteurs de croissance et des cytokines. La réponse métabolique à l'agression chez le brûlé est biphasique. La phase initiale est descendante, suivie d'une phase ascendante d'hypercatabolisme. L'augmentation de la consommation en oxygène et du métabolisme est en partie provoquée par la perte en chaleur au niveau des plaies, mais aussi, par un effet direct central, liée à l'inflammation qui agit sur l'hypothalamus. Bien que des hydrates de carbone, sous forme de glucose, semblent être une source importante d'énergie après un traumatisme, l'apport de seulement 5–6 mg/kg/min est suffisant. La néoglucogénèse, l'oxydation du glucose et la clairance plasmatique du glucose du brûlé sont accélérées. Les cycles métaboliques des hydrates de carbone, y compris le métabolisme anaérobie des lactates et le cycle de Cori sont inefficaces. De même, la lipolyse est accélérée et le cycle des acides gras est inefficace. Cependant, il est évident que les lipides chez le brûlé et d'autres patients victimes du traumatisme ne sont pas seulement une source d'énergie mais aussi un immunomodulateur du métabolisme des prostaglandines et d'autres voies de réponse immune. Le métabolisme des acides aminés chez le brûlé est caractérisé par une oxydation, une synthèse d'urée et un catabolisme protéique accrus, phénomènes prolongés et difficiles à réduire avec les moyens actuels de nutrition artificielle. Le but du soutien nutritionnel est cependant d'optimiser la synthèse protéique. Des besoins spécifiques peuvent nécessiter une supplémentation en glutamine et arginine après brûlures mais d'autres recherches sont nécessaires avant de pouvoir dire qu'une supplémentation en acides aminés branchés peut être utile. La recherche moderne a démontré l'importance de l'alimentation entérale qui empêche la traversée de la barrière muqueuse par les germes et les endotoxines. De même, il a été démontré que beaucoup des perturbations métaboliques dans les suites de brûlures et dans les états septiques sont dues, du moins en partie, aux cytokines inflammatoires. L'analyse de leur pathogénèse et leur mécanisme d'action à la fois au niveau tissulaire et cellulaire offrent d'importantes perspectives pour améliorer la compréhension et le contrôle thérapeutique des désordres métaboliques du brûlé.
Resumen
La lesión térmica mayor está relacionada con grados extremos de hipermetabolismo y catabolismo como las manifestaciones metabólicas principales que ocurren una vez cumplida exitosamente la resucitación de la fase de shock. Las determinaciones de sustratos y niveles hormonales, la calorimetría indirecta y el balance de nitrógeno son parámetros metabólicos de carácter bioquímico que son útiles y fácilmente disponibles, los cuales merecen estudios seriados para el manejo metabólico de los pacientes quemados. Sin embargo, la aplicación de isótopos estables con cromatografía de gas/espectrometría de masa y, más recientemente, nuevas inmunodeterminaciones para factores de crecimiento y citocinas, ha incrementado nuestro conocimiento y comprensión de las manifestaciones metabólicas del trauma severo.
La respuesta metabólica en los pacientes quemados es bifásica, en tanto que lafase ebb inicial es seguida de unafase flow hipermetabólica y catabólica. El aumento en el consumo de oxígeno/tasa metabólica se debe en parte a la pérdida evaporativa de calor a partir de las heridas de las víctimas de trauma, pero posiblemente también a un efecto central de la inflamación sobre el hipotálamo. Aunque los carbohidratos en forma de glucosa parecen ser una fuente energética importante, sólo hasta un máximo de 5–6 mg/kg/min son de beneficio. Los pacientes quemados exhiben aceleradas ratas de gluconeogénesis, oxidación de glucosa y depuración plasmática de glucosa. Además, se presenta considerable ciclaje futil de intermediarios de carbohidratos, lo cual incluye metabolismo anaeróbico de lactato y actividad del ciclo de Cori originados en el metabolismo de la glucosa y de otros sustratos a nivel de la herida. También se presenta lipolisis acelerada y ciclaje futil de ácidos grasos. Sin embargo, evidencias recientes sugieren que los lípidos en la dieta de los pacientes con quemaduras y otras formas de trauma sirven no sólo como fuentes energéticas, sino también como un factor importante de modulación del metabolismo de las prostaglandinas y de otras respuestas inmunitarias.
El metabolismo de aminoácidos en el paciente quemado se caracteriza por una oxidación incrementada, síntesis de urea y degradación proteica prolongada y difícil de controlar mediante la terapia nutricional actual. Sin embargo, el propósito actual del soporte nutricional es optimizar la síntesis proteica. Pueden existir requerimientos específicos de glutamina arginina suplementarias en las quemaduras, pero se requieren investigaciones adicionales antes de poder recomendar suplementos enriquecidos con aminoácidos racémicos en los pacientes quemados. Recientes investigaciones han revelado la importancia de la alimentación enteral para estimular las defensas de la mucosa intestinal contra bacterias y endotoxinas. También hay investigaciones que han demostrado que muchas de las alteraciones metabólicas de las quemaduras y las sepsis pueden ser debidas, por lo menos en parte, a las citocinas inflamatorias. La investigación de su patogénesis y mecanismo de acción, tanto al nivel tisular como celular, ofrece perspectivas importantes de una mejor comprensión y de superior control terapéutico de las alteraciones metabólicas de los pacientes quemados.
Similar content being viewed by others
References
Tredget, T.E., Shankowsky, H.A., Taerum, T., Moysa, G.L., Alton, J.D.M.: The role of inhalation injury in burn trauma: A Canadian experience. Ann. Surg. (in press)
Department of Health, Education, and Welfare: Reports of the Epidemiology and Surveillance of Injuries, Atlanta, Centers for Disease Control, 1982 (DHEW publication No. (HSM) 73–10001)
Feller, I., Tholen, D., Cornell, R.G.: Improvements in burn care 1965 to 1979. J.A.M.A.244:2074, 1980
Deitch, E.D.: The management of burns. N. Engl. J. Med.313:1389, 1985
Gump, G.E., Kinney, J.M.: Energy balance and weight loss in burned patients. Arch. Surg.103:442, 1971
Long, C.L., Spencer, J.L., Kinney, J.M.: Carbohydrate metabolism in man: Effect of elective operations and major trauma. J. Appl. Physiol.31:110, 1971
Soroff, H.S., Pearson, E., Artz, C.P.: An estimation of the nitrogen requirements for equilibrium in burned patients. Surg. Gynecol. Obstet.112:159, 1961
Saffle, J.R., Medina, E., Raymond, J., Westenskow, D., Kravitz, M., Warden, G.D.: Use of indirect calorimetry in the nutritional management of burned patients. J. Trauma25:32, 1985
Eccles, R.C., Swinamer, D.L., Jones, R.L., King, E.E.: Validation of a compact system for measuring gas exchange. Crit. Care Med.14:807, 1986
Phang, P.T., Rich, T., Ronco, J.: A validation and comparison study of two metabolic monitors. J.P.E.N. J. Parenter. Enteral. Nutr.14:259, 1990
Matthews, D.E., Bier, D.M.: Stable isotope methods for nutritional investigation. Annu. Rev. Nutr.3:309, 1983
Allsop, J.R., Wolfe, R.R., Burke, J.F.: Tracer priming the bicarbonate pool. J. Appl. Physiol.45:137, 1978
Young, V.R.: Stable isotopes in nutrition research. Fed. Proc.41:2677, 1982
Fong, Y., Moldawer, L.L., Shires, G.T., Lowry, S.F.: The biologic characteristics of cytokines and their implication in surgical injury. Surg. Gynecol. Obstet.170:363, 1990
Cuthbertson, D.P.: The disturbance of metabolism produced by bony and non-bony injury, with notes on certain abnormal conditions of bone. Biochem. J.24:1244, 1930
Cunningham, J.J., Hegarty, M.T., Meara, P.A., Burke, J.F.: Measured and predicted calorie requirements of adults during recovery from severe burn trauma. Am. J. Clin. Nutr.49:404, 1989
Ireton, C.S., Turner, W.W., Hunt, J.L., Baxter, C.: Evaluation of energy expenditures in burn patients. J. Am. Diet. Assoc.86:331, 1986
Burke, J.F., Quinby, W.C., Bondoc, C.C., Sheehy, E.M., Moreno, H.C.: The contribution of a bacterially isolated environment to the prevention of infection in seriously burned patients. Ann. Surg.186:377, 1987
Zawacki, B.E., Spitzer, K.W., Mason, A.D. Jr., Johns, L.A.: Does increased evaporative water loss cause hypermetabolism in burned patients? J. Appl. Physiol.38:593, 1975
Kupper, T.S., Deitch, E.A., Baker, C.C., Wong, W.: The human burn wound as a primary source of interleukin-1 activity. Surgery100:409, 1986
Ford, H.R., Hoffman, R.A., Wing, E.J.: Characterization of wound cytokine in the sponge matrix model. Arch. Surg.124:1422, 1989
Walter, J.S., Meyers, P., Krueger, J.M.: Microinjection of interleukin-1 into brain: Separation of sleep and fever responses. Physiol. Behav.44:555, 1988
Dinarello, C.A., Cannon, J.G., Wolff, S.M.: New concepts on the pathogenesis of fever. Rev. Infect. Dis.10:168, 1988
Allard, J.P., Jeejheebhoy, K.N., Whitwell, J., Pashutiniski, L., Peters, W.J.: Factors influencing energy expenditure in patients with burns. J. Trauma28:199, 1988
Goodwin, C.W.: Metabolism and nutrition in the thermally injured patient. Crit. Care Clin.1:97, 1985
Aulick, L.H., Wilmore, D.W.: Increased peripheral amino acid release following thermal injury. Ann. Surg.188:778, 1978
Perlmutter, D., Goldberger, G., Dinarello, C.A., Mizel, S.B., Colten, H.R.: Cachetin/tumor necrosis factor regulates hepatic acute phase gene expression. J. Clin. Invest.78:1349, 1986
Newsholme, E.A., Leech, A.R.: Regulation of glucose and fatty acid oxidation in relation to energy demand in muscle. In Biochemistry for the Medical Sciences, E.A. Newsholme, A.R. Leech, editors, Chicester-New York-Brisbane-Toronto-Singapore, John Wiley and Sons, 1983, pp. 300–335
Leninger, A.L.: Electron transport, oxidative phosphorylation, and regulation of ATP production. In Principles of Biochemistry, 3rd edition, S. Anderson, J. Fox, editors, New York, Worth Publishers, 1982, pp. 467–510
Wilmore, D.W., Aulick, L.H. Mason A. Jr., Pruitt, B.A. Jr.: Influence of the burn wound on local and systemic responses to injury. Ann. Surg.186:444, 1977
Wolfe, R.R., Herndon, D.N., Jahoor, F., Miyoshi, H., Wolfe, M.H.: Effect of severe burn injury of substrate cycling by glucose and fatty acids. N. Engl. J. Med.317:403, 1987
Shulman, G.I., Ladenson, P.W., Wolfe, M.H., Ridgway, E.C., Wolfe, R.R.: Substrate cycling between gluconeogenesis and glycolysis in euthyroid, hypothyroid, and hyperthyroid man. J. Clin. Invest.76:757, 1985
Burke, J.F., Wolfe, R.R., Mullany, D.J., Matthews, D.E., Bier, D.M.: Glucose requirements following burn injury. Ann. Surg.190:274, 1979
Wolfe, R.R., Durkot, M.J., Allsopo, J.R., Burke, J.F.: Glucose metabolism in severely burned patients. Metabolism28:1031, 1979
Tredget, E.E., Burke, J.F.: Calorie and substrate requirements in trauma and sepsis. In Trauma, Sepsis, and Shock, the Physiologic Basis of Therapy, G.H.A. Clowes, Jr., editor, New York-Basel, Marcel Dekker, Inc., 1988, pp. 269–305
Aulick, L.H., Wilmore, D.W., Mason, A.D. Jr., Pruitt, B.A. Jr.: Peripheral blood flow in thermally injured patients. Fed. Proc.36:417, 1977
Wolfe, R.R., Burke, J.F.: Effect of burn trauma on glucose turnover, oxidation, and recycling in guinea pigs. Am. J. Physiol.233:E80, 1976
Cori, C.F.: Mammalian carbohydrate metabolism. Physiol. Rev.11:143, 1931
Kreisbereg, R.A.: Pathogenesis and management of lactic acidosis. Ann. Rev. Med.35:181, 1984
Laugness, U., Udenfriend, S.: Collagen proline hydroxylase activity and anaerobic metabolism. In Biology of the Fibroblast, E. Kulonen, J. Pikkarainen, editors, New York, Academic Press, 1973, pp. 373
Hunt, T.K., Conolly, W.B., Aronson, S.B.: Anaerobic metabolism and wound healing: An hypothesis for the initiation and cessation of collagen synthesis in wounds. Am. J. Surg.135:328, 1978
Black, P.R., Brooks, D.C., Bessey, P.Q., Wolfe, R.R., Wilmore, D.W.: Mechanisms of insulin resistance following injury. Ann. Surg.196:420, 1982
Jahoor, F., Wolfe, R.R.: Role of insulin and glucagon in the response of glucose and alanine kinetics in burn injured patients. J. Clin. Invest.78:807, 1986
Czech, M.P.: New perspectives on the mechanism of insulin action. Recent Prog. Horm. Res.40:346, 1985
Brooks, D.C., Bessey, P.Q., Black, P.R., Wolfe, R.R., Wilmore, D.W.: Post-traumatic insulin resistance in uninjured forearm tissue. J. Surg. Res.37:100, 1984
Shangraw, R.E., Jahoor, F., Miyoshi, H., Neff, W.A., Stuart, C.A., Herndon, D.N., Wolfe, R.R.: Differentiation between septic and postburn insulin resistance. Metabolism38:983, 1989
Jahoor, F., Shangraw, R.E., Miyoshi, H., Wallfish, H., Herndon, D.N., Wolfe, R.R.: Role of insulin and glucose oxidation in mediating the protein catabolism of burns and sepsis. Am. J. Physiol.257:E323, 1989
Gottschlich, M.M., Alexander, J.W.: Fat kinetics and recommended dietary intake in burns. J.P.E.N. J. Parenter. Enteral. Nutr.11:80, 1987
Galster, A.D., Bier, D.M., Cryer, P.E., Monafo, W.W.: Plasma palmitate turnover in subjects with thermal injury. J. Trauma24:938, 1984
Wolfe, R.R., Herndon, D.N., Peters, E.J., Jahoor, F., Desai, M.H., Holland, O.B.: Regulation of lipolysis in severely burned children. Ann. Surg.206:214, 1987
Wilmore, D.W., Moylan, J.A., Jelmkamp, G.M., Pruitt, B.A. Jr.: Clinical evaluation of a 10% intravenous fat emulsion for parenteral nutrition in thermally injured patients. Ann. Surg.178:503, 1973
Kudsk, K.A., Stone, J.M., Sheldon, G.F.: Nutrition in trauma and burns. Surg. Clin. North Am.62:183, 1982
Wan, J.M.F., Teo, T.C., Babayan, V.K., Blackburn, G.L.: Lipids and the development of immune dysfunction and infection. J.P.E.N. J. Parenter. Enteral. Nutr.12:43S, 1988
Wolfe, B.M., Ney, D.M.: Lipid metabolism in parenteral nutrition. In Parenteral Nutrition, J.L. Rombeau, M.D. Caldwell, editors, Philadelphia, W.B. Saunders, 1986, pp. 72–99
Kinsella, J.E., Lokesh, B., Broughton, S.: Dietary polyunsaturated fatty acids and eicosanoids: Potential effects on the modulation of inflammatory and immune cells: An Overview. Nutrition5:24, 1990
Hageman, J.R., McCulloch, K., Gora, P., Olsen, E.K., Pachman, L., Hunt, C.E.: Intralipid alterations in pulmonary prostaglandin metabolism and gas exchange. Crit. Care Med.11:794, 1983
Abel, R.M., Fisch, D., Grossman, M.L.: Hemodynamic effects of intravenous 20% soy oil emulsion following coronary bypass surgery. J.P.E.N. J. Parenter. Enteral. Nutr.7:534, 1983
Hamaway, K.J., Moldawer, L.L., Georgieff, M., Valicenti, A.J., Babyan, V.K., Bistrian, B.R., Blackburn, G.L.: The effect of lipid emulsions on reticuloendothelial system function in the injured animal. J.P.E.N. J. Parenter. Enteral. Nutr.9:559, 1985
Freeman, J., Goldmann, D.A., Smith, N.E., Sidebottom, D.G., Epstein, M.F., Platt, R.: Association of intravenous lipid emulsion and coagulase-negative staphylococcal bacteremia in neonatal intensive care units. N. Engl. J. Med.323:301, 1990
Griffin, E., Breckenridge, W.C., Kuksis, A., Bryan, M.H., Angel, A.: Appearance and characterization of lipoprotein X during continuous intralipid infusions in the neonate. J. Clin. Invest.64:1703, 1979
Untraucht, S.: Alterations of serum lipoproteins resulting from total parenteral nutrition with intralipid. Biochim. Biophys. Acta711:176, 1982
Alexander, J.W., Saito, H., Ogle, C.K., Trocki, O.: The importance of lipid type in the diet after burn injury. Ann. Surg.204:1, 1986
Endres, S., Ghobani, R., Kelley, V.E., Cannon, J., Dinarello, C.A.: The effect of dietary supplementation with N-3 polyunsaturated fatty acids on the synthesis of interleukin-1 and tumor necrosis factor by mononuclear cells. N. Engl. J. Med.320:252, 1989
Babayan, V.K.: Medium chain triglycerides and structured lipids. Lipids22:417, 1987
Kinsella, J.E.: Lipids, membrane receptors, and enzymes: Effects of dietary fatty acids. J.P.E.N. J. Parenter. Enteral. Nutr.14:200S, 1990
Jensen, G.L., Mascioli, E.A., Seidner, D.L., Istafan, N.W., Donmitch, A.M., Selleck, K., Babayan, V.K., Blackburn, G.L., Bistrian, B.R.: Parenteral infusion of long- and medium-chain triglycerides and reticuloendothelial system function in man. J.P.E.N. J. Parenter. Enteral. Nutr.14:467, 1990
DeMichele, S.J., Karlstad, M.D., Bistrian, B.R., Istafan, N., Babayan, V.K., Blackburn, G.L.: Enteral nutrition with structured lipid: Effect on protein metabolism in thermal injury. Am. J. Clin. Nutr.50:1295, 1989
Mullen, J.L.: Consequences of malnutrition in the surgical patients. Surg. Clin. North Am.61:465, 1981
Moore, F.D., Brennan, M.F.: Surgical injury. In Manual of Surgical Nutrition, F.D. Bellinger, editor, Philadelphia, Saunders, 1975, pp. 169–222
Kinney, J.M., Elwyn, D.H.: Protein metabolism and injury. Ann. Rev. Nutr.3:433, 1983
Jahoor, F., Desai, M., Herdon, D.N., Wolfe, R.R.: Dynamics of the protein metabolic response to burn injury. Metabolism4:330, 1988
Hedden, M.P., Mazuski, J.E., Chute, E.: General stimulation of muscle protein synthesis by branched-chain amino acidsin vitro. Proc. Soc. Exp. Bio. Med.160:410, 1979
Hagenfeldt, L., Eriksson, S., Wahren, J.: Influence of leucine on arterial concentrations and regional exchange of amino acids in healthy subjects. Clin. Sci.59:173, 1980
Elia, M., Farrell, R., Ilie, V., Smith, R., Williamson, D.H.: The removal of infused leucine after injury, starvation and other conditions in man. Clin. Sci.59:275, 1980
Desai, S.P., Bistrain, B.R., Moldawere, L.L., Miller, M.M., Blackburn, G.L.: Plasma amino acid concentrations during branched-chain amino acid infusion in stressed patients. J. Trauma22:747, 1982
Wolfe, R.R., Goodenough, R.D., Burke, J.F., Wolfe, M.H.: Response of protein and urea kinetics in burn patients to different levels of protein intake. Ann. Surg.197:163, 1983
Yu, Y.M., Wagner, D.A., Waleswski, J.C., Burke, J.F., Young, V.R.: A kinetic study of leucine metabolism in severely burned patients. Ann. Surg.207:421, 1988
Milliken, W.J., Jr., Henderson, J.M., Galloweay, J.R.:In vivo measurement of leucine metabolism with stable isotopes in normal subjects and in those with cirrhosis fed conventional and branched-chain amino acid enriched diets. Surgery98:405, 1986
Wolfson, A.M.I.: Amino acids-their role as an energy source. Proc. Nutr. Soc.42:489, 1983
Brennan, M.F., Cerra, F., Daly, J.M., Fischer, J.E., Moldawer, L.L., Smith, R.J., Vinnars, E., Wannemacher, R., Young, V.R.: Report of a research workshop: Branched-chain amino acids in stress and injury. J.P.E.N. J. Parenter. Enteral. Nutr.10:446, 1986
Garlick, P.J., Grant, I.: Amino acid infusion increases the sensitivity of muscle protein synthesisin vivo to insulin. Biochem. J.254:579, 1988
Newsholme, E.A., Newsholme, D.P., Phil, D., Curi, R., Challoner, E., Ardawi, M.S.M.: A role for muscle in the immune system and its importance in surgery, trauma, sepsis and burns. Nutrition International4:261, 1988
Bergstrom, L., Furst, P., Noree, L.O., Vinnars, E.: Intracellular free amino acid concentration in human muscle tissue. J. Appl. Physiol.36:693, 1974
Smith, R.J.: Regulation of protein degradation in differentiated skeletal muscle cells in monolayer culture, in intracellular protein catabolism. Prog. Clin. Biol. Res.180:633, 1984
Rennie, M.J., Hundal, H.S., Babil, P., MacLennan, P.A., Taylor, P.M., Watt, P.W.: Characteristics of a glutamine carrier in skeletal muscle have important consequence for nitrogen loss in injury, infection and chronic disease. Lancet2:1008, 1986
Jepson, M.M., Bates, P.C., Broadbent, P., Pell, J.M., Millward, D.J.: Relationship between glutamine concentration and protein synthesis in rat skeletal muscle. Am. J. Physiol.255:E166, 1988
Maclennan, P.A., Brown, R.A., Rennie, M.J.: A positive relationship between protein synthetic rate and intracellular glutamine concentration in perfused rat skeletal muscle. FEBS Lett.215:187, 1987
Vinnars, E., Bergstrom, J., Furst, P.: Influence of postoperative state on the intracellular free amino acids in human muscle tissue. Ann. Surg.192:78, 1980
Askanazi, J., Carpentier, J.A., Michelsen, C.B., Elwyn, U.H., Furst, P., Kantrowitz, L.R., Gump, F.E., Kinney, J.M.: Muscle and plasma amino acids following injury: Influence of intercurrent infection. Ann. Surg.192:78, 1980
Hundal, H.S., Rennie, M.J., Watt, P.W.: Characteristics of glutamine transport in perfused rat skeletal muscle. J. Physiol. (Lond)393:283, 1987
Ahmed, A., Talor, P.M., Rennie, M.J.: Characteristics of glutamine transport in sarcolemmal vesicles from rat skeletal muscle. Am. J. Physiol.259:E284, 1990
Newsholme, E.A., Leech, E.A.: Biochemistry for the Medical Sciences, Chichester, John Wiley & Sons, 1983, pp. 233–234
Newsholme, E.A., Crabtree, B., Ardawi, M.S.M.: The role of high rates of glycolysis and glutamine utilization in rapidly dividing cells. Biosci. Rep.4:393, 1985
Newsholme, E.A., Crabtree, B., Ardawi, M.S.M.: Glutamine metabolism in lymphocytes, its biochemical, physiological and clinical importance. Q. J. Exp. Physiol.70:473, 1985
Newsholme, E.A., Newsholme, P., Curi, R.: The role of citric acid cycle in cells of the immune system and its importance in sepsis, trauma and burns. Biochem. Soc. Symp.54:145, 1987
Newsholme, E.A., Parry-Billings, M., Phil, D.: Properties of glutamine release from muscle and its importance for the immune system. J.P.E.N. J. Parenter. Enteral. Nutr.14:63s, 1990
Dimarchi, R.D., Tam, J.P., Kent, S.B., Merrifield, R.B.: Weak acid-catalyzed pyrrolidine carboxylic acid formation from glutamine during solid phase peptide synthesis. Int. J. Pept. Protein Res.19:88, 1982
Stehle, P., Ratz, I., Furst, P.:In vivo utilization of intravenously supplied L-alanine-L-glutamine in various tissues of the rat. Nutrition5:411, 1989
Adibi, S.A.: Experimental basis for use of peptides as substrate for parenteral nutrition: A review. Metabolism36:1001, 1987
Furst, P., Albers, S., Stehle, P.: Glutamine-containing dipeptides in parenteral nutrition. J.P.E.N. J. Parenter. Enteral. Nutr.14:118s, 1990
Stehle, P., Ratz, I., Furst, P.:In vivo utilization of intravenously supplied L-alanine-L-glutamine in various tissues of the rat. Nutrition5:411, 1989
Adibi, S.A.: Experimental basis of for use of peptides as substrate for parenteral nutrition: A review. Metabolism36:1001, 1987
Hammarqvist, F., Wernerman, J., Ali, R., Von Der Decken, A., Vinnars, E.: Addition of glutamine to total parenteral nutrition after elective abdominal surgery spares free glutamine in muscle, counteracts the fall in muscle protein synthesis, and improves nitrogen balance. Ann. Surg.209:455, 1989
Stehle, P., Zander, J., Mertes, N., Albers, S., Puchstein, C., Lawin, P., Furst, P.: Effect of parenteral glutamine peptide supplements on muscle glutamine loss and nitrogen balance after major surgery. Lancet1:231, 1989
Ziegler, T.R., Benfell, K., Smith, R.J., Young, L.S., Brown, E., Ferrari-Baliviera, E., Lowe, D.K., Wilmore, D.W.: Safety and metabolic effects of L-glutamine administration in humans. J.P.E.N. J. Parenter. Enteral Nutr.14:137s, 1990
Grant, J.P., Snyder, P.J.: Use of L-glutamine in total parenteral nutrition. J. Surg. Res.44:506, 1988
Souba, W.W., Klimberg, V.S., Hautamaki, R.D., Mendenhall, W.H., Bova, F.C., Howard, R.J., Bland, K.I., Copeland, E.M.: Oral glutamine reduces bacterial translocation following abdominal radiation. J. Surg. Res.48:1, 1990
Souba, W.W., Klimberg, V.S., Plumley, D.A., Salloum, R.M., Flynn, T.C., Bland, K.I., Copeland, E.M.: The role of glutamine in maintaining gut structure and function and supporting the metabolic response to injury and infection. J. Surg. Res.48:383, 1990
Seifter, E., Rettura, G., Barbul, A., Levenson, S.M.: Arginine: An essential amino acid for injured rats. Surgery84:224, 1978
Barbul, A.: Arginine: Biochemistry, physiology and therapeutic implications. J.P.E.N. J. Parenter. Enteral. Nutr.10:227, 1986
Saito, H., Trocki, O., Wang, S.L., Gonce, S.J., Joffe, S.N., Alexander, J.W.: Metabolic and immune effects of dietary arginine supplementation after burn. Arch. Surg.122:784, 1987
Alexander, J.W., Gottschlich, M.M.: Nutritional immunomodulation in burn patients. Crit. Care Med.18:S149, 1990
Daly, J.M., Reynolds, J., Thom, A., Kinsley, L., Dietrick-Gallagher, M.: Metabolic effects of arginine in the surgical patients. Ann. Surg.208:512, 1988
Barbul, A., Wasserkrug, H.L., Penberthy, L.T., Norman, N.Y., Tao, R.C., Efron, G.: Optimal levels of arginine in maintenance intravenous hyperalimentation. J.P.E.N. J. Parenter. Enteral. Nutr.8:281, 1984
Barbul, A.: Arginine: Biochemistry, physiology and therapeutic implications. J.P.E.N. J. Parenter. Enteral. Nutr.10:227, 1986
Barbul, A., Lazarou, S.A., Efron, D.T., Wasserkrug, H.L., Effron, G.: Arginine enhances wound healing and lymphocyte immune responses in humans. Surgery108:331, 1990
Hibbs, J.B., Taintor, R.R., Vavrin, Z.: Macrophage cytotoxicity: Role for L-arginine deaminase and imino nitrogen oxidation to nitrite. Science235:473, 1987
Granger, D.L., Hibbs, J.B., Jr., Perfect, J.R., Durack, D.T.: Specific amino acid (L-arginine) requirement for the microbiostatic activity of murine macrophages. J. Clin. Invest.81:1129, 1988
Granger, D.L., Hibbs, J.B., Jr., Perfect, J.R., Durack, D.T.: Metabolic fats of L-arginine in relation to microstatic capability of murine macrophages. J. Clin. Invest.85:264, 1990
Randomski, M.W., Palmer, R.M.J., Moncada, S.: An L-arginine/nitric oxide pathway present in human platelets regulates aggregation. Proc. Natl. Acad. Sci.87:5193, 1990
Leaf, C.D., Wishnock, J.S., Tennenbaum, S.R.: L-arginine is a precursor for nitrate biosynthesis in humans. Biochem. Biophys. Res. Commun.163:1032, 1989
Albina, J.E., Mills, C.D., Barbul, A., Thirkill, C.E., Henry, W.L., Jr., Mastrofrancesco, B., Caldwell, M.D.: Arginine metabolism in wounds. Am. J. Physiol.254:E459, 1988
Albina, J.E., Mills, C.D., Henry, W.L., Jr., Caldwell, M.D.: Temporal expression of different pathways of L-arginine metabolism in healing wounds. J. Immunol.144:3877, 1990
Barbul, A., Rettura, G., Prior, E., Levenson, S.M., Seifter, E.: Supplemental arginine, wound healing and thymus: Arginine-pituitary interactions. Surg. Forum29:93, 1978
Barbul, A., Lazarou, S.A., Efron, D.T., Wasserkrug, H.L., Efron, G.: Arginine enhances wound healing and lymphocyte immune response in humans. Surgery108:331, 1990
Manson, J.M., Wilmore, D.W.: Positive nitrogen balance with human growth hormone and hypocaloric intravenous feeding. Surgery100:188, 1986
Windmueller, H.G., Spaeth, A.E.: Respiratory fuel and nitrogen metabolismin vivo in small intestine of fed rats. J. Biol. Chem.255:107, 1980
Windmueller, H.G., Spaeth, A.E.: Intestinal metabolism of glutamine and glutamate from the lumen as compared to glutamine from blood. Arch. Biophys. Biochem.171:662, 1975
Wilmore, D.W., Smith, R.J., O'Dwyer, S.T., Jacobs, D.O., Ziegler, T.R., Wang, X.D.: The gut: A central organ after surgical stress. Surgery104:917, 1988
Muhlbacher, F., Kapadia, C.R., Colpoys, M.F., Smith, R.J., Wilmore, D.W.: Effects of glucocorticoids on glutamine metabolism in skeletal muscle. Am. J. Physiol.247:E75, 1984
Brooks, D., Bessey, P.Q., Black, P.R., Aoki, T.T., Wilmore, D.W.: Insulin stimulated branched-chain amino acid uptake diminishes nitrogen efflux from skeletal muscle of injured patients. J. Surg. Res.40:395, 1986
Souba, W.W., Herskowitz, K., Salloum, R.M., Chen, M.K., Austgen, T.R.: Gut glutamine metabolism. J.P.E.N. J. Parenter. Enteral. Nutr.14:45s, 1990
Barry, G.: Structure, biochemistry, and assembly of epithelial tight junctions. Am. J. Physiol.253:c749, 1987
Madara, J.L.: Loosening tight junctions: Lessons from the intestine. J. Clin. Invest.83:1089, 1989
Dobbins, W.O., 3rd.: Gut immunophysiology: A gastroenterologist's view with emphasis on pathophysiology. Am. J. Physiol.242:G1, 1982
Wells, C.L., Maddaus, M.A., Simons, R.L.: Proposed mechanisms for the translocation of intestinal bacteria. Rev. Infect. Dis.10:958, 1988
Deitch, E.A.: The management of burns. N. Engl. J. Med.323:1249, 1990
Levine, G.M., Deren, J.J., Steiger, E.: Role of oral intake in maintenance of gut mass and disaccharidase activity. Gastroenterology67:975, 1974
Dworkin, L.D., Levine, G.M., Farber, N.J.: Small intestinal mass of the rat is partially determined by indirect effects of intraluminal nutrition. Gastroenterology71:626, 1976
Johnson, L.R., Copeland, E.M., Dudrick, J.J.: Structural and hormonal alterations in the gastrointestinal tract of parenterally fed rats. Gastroenterology68:117, 1975
Alverdy, J.A., Chi, H.S., Sheldon, G.S.: The effect of parenteral nutrition on gastrointestinal immunity: The importance of intestinal stimulation. Ann. Surg.202:681, 1985
Moore, F.A., Moore, E.E., Jones, T.N., McCroskey, B.L., Peterson, V.M.: TEN vs TPN following major abdominal trauma: Reduced septic morbidity. J. Trauma29:916, 1989
Border, J.R., Massett, J., LaDuca, J., Seibel, R., Steinberg, S., Mills, B., Losi, P., Border, D.: The gut origin septic states in blunt multiple trauma (ISS-40) in the ICU. Ann. Surg.206:427, 1987
Wilmore, D.W.: Nutrition and metabolism following thermal injury. Clin. Plast. Surg.1:603, 1979
Bessey, P.Q., Watters, J.M., Aoki, T.T., Wilmore, D.W.: Combined hormonal infusion stimulates the metabolic response to injury. Ann. Surg.200:264, 1984
Shamoon, H.M., Hendler, R., Sherwin, R.S.: Synergistic interactions among anti-insulin hormones in the pathogenesis of stress hyperglycemia in humans. J. Clin. Endocrinol. Metab.52:1235, 1985
Watters, J.M., Bessey, P.Q., Dinarello, C.A., Wolff, S.M., Wilmore, D.W.: Both inflammatory and endocrine mediators stimulate host responses to sepsis. Arch. Surg.121:179, 1986
Kupper, T.S., Deitch, E. A., Baker, C.C., Wong, W.: The human burn wound as a primary source of interleuekin-1 activity. Surgery100:409, 1986
Sauder, D.N., Monick, M.M., Hunninghake, G.W.: Epidermal cell derived thymocyte activating factor (ETAF) is a potent T cell chemoattractant. J. Invest. Dermatol.85:431, 1985
Heideman, M.: Complement activation by thermal injury and its possible consequences for immune defense. In The Immune Consequences of Thermal Injury, J.L. Ninneman, editor, Baltimore, Williams and Wilkins, 1981, pp. 127–131
Okusawa, S., Dinarello, C.A., Yancey, K.B., Endres, S., Lawley, J.J., Frank, M.M., Burke, J.F., Gelfand, J.A.: C5a induction of human interleukin-1. J. Immunol.139:2635, 1985
Marano, M.A., Fong, Y., Moldawer, L.L., Tracey, K.J., Lowry, S.F., Beutler, B., Shires, T.S.: Serum cachectin/TNF in critically ill burn patients correlates with infection and mortality. Surg. Gynecol. Obstet.170:32, 1990
Guo, J., Dickerson, C., Chrest, F.J., Adler, W.H., Munster, A.M., Winchurch, R.A.: Increased levels of circulating interleukin-6 in burn patients. Clin. Immunol. Immunopathol.54:361, 1990
Tredget, E.E., Yu, Y.M., Zhong, S., Burini, R., Okusawa, S., Gelfand, J.A., Dinarello, C.A., Young, V.R., Burke, J.F.: Role of interleukin 1 and tumor necrosis factor on energy metabolism in rabbits. Am. J. Physiol.255:E760, 1988
Feingold, K.R., Grunfeld, C.: Tumor necrosis factor-alpha stimulates hepatic lipogenesis in the ratin vivo. J. Clin. Invest.80:184, 1987
Perlmutter, D.H., Dinarello, C.A., Punsal, P.K., Colten, H.R.: Cachectin tumor necrosis factor regulates hepatic acute phase gene expression. J. Clin. Invest.78:1349, 1986
Warren, R.S., Starnes, H.F., Gabrilove, J.L.: The acute metabolic effects of tumor necrosis factor administration. Arch. Surg.122:1396, 1987
Dinarello, C.A., Mier, J.W.: Current concepts: Lymphokines. N. Engl. J. Med.317:940, 1987
Tracey, K.J., Lowry, S.F., Fahey, T.J., III, Albert, J.D., Fong, Y., Hesse, D., Beutler, B., Manogue, K.R., Calvano, S., Wei, H., Cerami, A., Shires, G.R.: Cachectin/tumor necrosis factor induces lethal shock and stress hormone responses in the dog. Surg. Gynecol. Obstet.164:415, 1987
Uehara, A., Gottschall, P.E., Dahl, R.R., Arimura, A.: Interleukin-1 stimulates ACTH release by an indirect action which requires endogenous corticotropin releasing factor. Endocrinology121:1580, 1987
Sandler, S., Bentzen, K., Borg, L.A.H.: Studies on the mechanisms causing inhibition of insulin secretion in rat pancreatic islets exposed to human interleukin-1 beta indicate a perturbation in the mitochondrial function. Endocrinology124:1492, 1989
Woloski, M.M.R.N.J., Smith, E.M., Meyer, W.J., III, Fuller, G.M., Blalock, J.E.: Corticotropin-releasing activity of monokines. Science230:1035, 1985
Bernton, E.W., Beach, J.E., Holady, J.W., Smallridge, R.C., Fein, H.G.: Release of multiple hormones by a direct action of interleukin-1 on pituitary cells. Science238:521, 1987
Baracos, V., Rodemann, P., Dinarello, C.A., Goldberg, A.L.: Stimulation of muscle protein degradation and prostaglandin E2 release by leukocytic pyrogen (interleukin-1). N. Engl. J. Med.303:553, 1983
Libby, P., Ordovas, J.M., Auger, K.R., Robbins, A.H., Birinyi, L.K., Dinarello, C.A.: Endotoxin and tumor necrosis factor induce interleukin-1 gene expression in adult human vascular endothelial cells. Am. J. Pathol.124:179, 1986
Dayer, J.M., DeRochemonteix, B., Burrus, B.: Human recombinant interleukin-1 stimulates collagenase and prostaglandin E2 production by human synovial cells. J. Clin. Invest.77:645, 1986
Lee, M.D., Zentella, A., Pekala, P.H., Cerami, A.: Effect of endotoxin-induced monokines on glucose metabolism in the muscle cell line L6. Biochemistry84:2590, 1987
Vary, T.C., Siegel, J.H., Nakatani, T., Sato, T., Aoyama, H.: Effect of sepsis on activity of pyruvate dehydrogenase complex in skeletal muscle and liver. Am. J. Physiol.250:E634, 1986
Sayeed, M.M.: Ion transport in circulatory and/or septic shock. Am. J. Physiol.252:R809, 1987
Spitzer, J.A., Deaciuc, I.V.: IP3-independent Ca2+ release in permeabilized hepatocytes of endotoxemic and septic rats. Am. J. Physiol.16:E130, 1987
Dinarello, C.A., Savage, N.: Interleukin-1 and its receptor. Crit. Rev. Immun.9:1, 1989
Kunkel, S.L., Remick, D.G., Strieter, R.M., Larrick, J.W.: Mechanisms that regulate the production and effects of tumor necrosis factor-alpha. Crit. Rev. Immunol.9:93, 1989
Granger, D.L., Lehninger, A.L.: Sites of inhibition of mitochondrial electron transport in macrophage-injured neoplastic cells. J. Cell. Biol.95:527, 1982
Kilbourn, R.G., Klostergaard, J., Lopez-Berestein, G.: Activated macrophages secrete a soluble factor that inhibits mitochondrial respiration of tumor cells. J. Immunol.133:2577, 1984
Rosenstreitch, D.L., Yost, S.L., Brown, K.M.: Human urine-derived inhibitors of interleukin-1. Rev. Infect. Dis.9(suppl 5):594, 1987
Jiang, J., He, G., Zhang, S., Wang, X., Yang, N., Zhu, Y., Wilmore, D.W.: Low-dose growth hormone and hypocaloric nutrition attenuate the protein-catabolic response after major operation. Ann. Surg.210:513, 1989
Tracey, K.J., Yuman, F., Hesse, D.G.: Anti-cachetin/TNF monoclonal antibodies prevent septic shock during lethal bacteremia. Nature33:662, 1987
Strock, L.L., Singh, H., Abdullah, A., Miller, J.A., Herndon, D.N.: The effect of insulin-like growth factor I on postburn hypermetabolism. Surgery108:161, 1990
Herndon, D.N., Barrow, R.E., Kunkel, K.R., Broemeling, L., Rutan, R.L.: Effects of recombinant human growth hormone on donor-site healing in severely burned children. Ann. Surg.212:424, 1990
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tredget, E.E., Yu, Y.M. The metabolic effects of thermal injury. World J. Surg. 16, 68–79 (1992). https://doi.org/10.1007/BF02067117
Issue Date:
DOI: https://doi.org/10.1007/BF02067117