Abstract
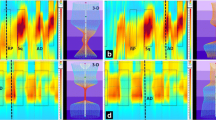
PURPOSE: A study was undertaken to assess physiologic characteristics and clinical significance of anismus. Specifically, we sought to assess patterns of anismus and the relation of these findings to the success of therapy. METHODS: Sixty-eight patients were found to have anismus based on history and diagnostic criteria including anismus by defecography and at least one of three additional tests: anorectal manometry, electromyography, or colonic transit time study. Interpretation of defecography was based on the consensus of at least three of four observers. Anal canal hypertonia (n=32) was defined when mean and maximum resting pressures were at least 1 standard deviation higher than those in 63 controls. There were two distinct defecographic patterns of anismus: Type A (n=26), a flattened anorectal angle without definitive puborectalis indentation but a closed anal canal; Type B (n=42), a clear puborectalis indentation, narrow anorectal angle, and closed anal canal. Outcomes of 57 patients who had electromyographybased biofeedback therapy were reported as either improved or unimproved at a mean follow-up of 23.7 (range, 6–62) months. These two types of anismus were compared with biofeedback outcome to assess clinical relevance. RESULTS: Patients with Type A anismus showed greater perineal descent at rest (mean, 5.1 vs. 3.5 cm;P < 0.01), greater dynamic descent between rest and evacuation (mean, 2.7 vs. 1.4 cm;P <0.01), greater difference of anorectal angle between rest and evacuation (mean, 14.6 vs. −3.1°;P <0.001), higher mean resting pressure (mean, 77.1 vs. 62.8 mmHg;P <0.05), lower mean squeeze pressure (58.8 vs. 80.7 mmHg;P <0.05), and a higher incidence of anal canal hypertonia (69.2 vs. 33.3 percent;P <0.01) than did patients with Type B anismus. Only 25 percent of patients who had Type A anismus with anal canal hypertonia were improved by biofeedback therapy. Conversely, 86 percent of patients with Type B anismus without anal canal hypertonia were successfully treated with biofeedback (P <0.001; Fisher's exact test). CONCLUSIONS: These two distinct physiologic patterns of anismus correlate with the success of biofeedback treatment. Therefore, knowledge of these patterns may help direct therapy.
Similar content being viewed by others
References
Kuijpers JH, Bleijenberg G. Assessment and treatment of obstructed defecation. Ann Med 1990;22:405–11.
Bartolo DC, Roe AM, Virjee J, Mortensen NJ, Locke-Edmunds JC. An analysis of rectal morphology in obstructed defecation. Int J Colorectal Dis 1988;3:17–22.
Meunier P, Marechal JM, de Beaujeu MJ. Rectoanal pressure and rectal sensitivity studies in chronic childhood constipation. Gastroenterology 1979;77:330–6.
Preston DM, Lennard-Jones JE. Anismus in chronic constipation. Dig Dis Sci 1985;30:413–8.
Jones PN, Lubowski D2, Swash M, Henry MM. Is paradoxical contraction of puborectalis muscle of functional importance? Dis Colon Rectum 1987;30:667–70.
Parks AG, Porter NH, Melzak J. Experimental study of the reflex mechanism controlling the muscles of the pelvic floor. Dis Colon Rectum 1962;5:407–14.
Rasmussen O. Anorectal function. Dis Colon Rectum 1994;37:386–403.
Johansson C, Ihre T, Holmström B, Nordström E, Dolk A, Bróden G. A combined electromyographic and cineradiologic investigation in patients with defecation disorders. Dis Colon Rectum 1990;33:1009–13.
Kuijpers JH, Strijk SP. Diagnosis of disturbances of continence and defecation. Dis Colon Rectum 1984;27:658–62.
Jorge JM, Wexner SD, Ger GC, Salanga VD, Nogueras JJ, Jagelman DG. Cinedefecography and electromyography in the diagnosis of nonrelaxing puborectalis syndrome. Dis Colon Rectum 1993;36:668–76.
Jorge JM, Wexner SD, Marchetti F, Rosato GO, Sullivan ML, Jagelman DG. How reliable are currently available methods of measuring the anorectal angle? Dis Colon Rectum 1992;35:332–8.
Wexner SD, Marchetti F, Salanga VD, Corredor C, Jagelman DG. Neurophysiologic assessment of the anal sphincters. Dis Colon Rectum 1991;34:606–12.
Ger GC, Wexner SD, Jorge JM, Salanga VD. Anorectal manometry in the diagnosis of paradoxical puborectalis contraction. Dis Colon Rectum 1993;36:816–25.
Jorge JM, Wexner SD. A practical guide to basic anorectal physiology. Contemp Surg 1993;43:214–24.
Barnes PR, Hawley PR, Preston DM, Lennard-Jones JE. Experience of posterior division of the puborectalis muscle in the management of chronic constipation. Br J Surg 1985;72:475–7.
Kuijpers JH, Bleijenberg G. The spastic pelvic floor syndrome. Dis Colon Rectum 1985;28:669–72.
Kerremans R. Electrical activity and mobility of the internal anal sphincter: an “in vivo” electrophysiological study in man. Acta Gastroenterol Belg 1968;31:465–482.
Ihre T. Studies in anal function in continent and incontinent patients. Scand J Gastroenterol Suppl 1974;25:1–64.
Gaston EA. The physiology of fecal incontinence. Surg Gynecol Obstet 1948;87:280–90.
Duthie HL, Watts J. Contribution of the external anal sphincter to the pressure zone in the anal canal. Gut 1965;6:64–8.
Frenckner B, von Euler C. Influence of pudendal block on the function of the anal sphincters. Gut 1975;16:482–9.
Floyd W, Walls E. Electromyography of the anal sphincter ani externus in man. J Physiol (Lond) 1953;122:599–609.
Kumar D, Waldron D, Williams NS, Browning C, Hutton MR, Wingate DL. Prolonged anorectal manometry and external anal sphincter electromyography in ambulant human subjects. Dig Dis Sci 1990;35:641–8.
Gaston EA. Physiological basis for preservation of fecal continence after resection of the rectum. JAMA 1951;146:1486–9.
Roberts JP, Womack NR, Hallan RI, Thorpe AC, Williams NS. Evidence from dynamic integrated proctography to redefine anismus. Br J Surg 1992;79:1213–5.
Hancock BD. Measurement of anal pressure and mobility. Gut 1976;17:645–51.
Hancock BD. Internal sphincter and the nature of hemorrhoids. Gut 1977;18:651–6.
Duthie GS, Miller R, Bartolo DC. Internal anal sphincter of electromyographic frequency is related to anal canal resting pressure [abstract]. Gut 1993;31:A619.
Wexner SD, Cheape JD, Jorge JM, Heymen S, Jagelman DG. Prospective assessment of biofeedback for the treatment of paradoxical puborectalis contraction. Dis Colon Rectum 1992;35:145–50.
Bleijenberg G, Kuijpers HC. Treatment of the spastic pelvic floor syndrome with biofeedback. Dis Colon Rectum 1987;30:108–11.
Fleshman JW, Dreznik Z, Meyer K, Fry RD, Carney R, Kodner IJ. Outpatient protocol for biofeedback therapy of pelvic floor outlet obstruction. Dis Colon Rectum 1992;35:1–7.
Hallan RI, Williams NS, Melling J,et al. Treatment of anismus in intractable constipation with botulinum A toxin. Lancet 1988;2:714–7.
Barnes PR, Hawley PR, Preston DM,et al. Experience of posterior division of the puborectalis muscle in the management of chronic constipation. Br J Surg 1985;72:475.
Guillemot F, Leroi H, Lone YC, Rousseau CG, Lamblin M-D, Cortot A. Action ofin situ nitroglycerin on upper anal canal pressure of patients with terminal constipation: a pilot study. Dis Colon Rectum 1993;36:372–6.
Weber J, Ducrotte Ph, Touchais JY, Roussignol C, Denis PH. Biofeedback training for constipation in adults and children. Dis Colon Rectum 1987;30:844–6.
Gorfine SR. Treatment of benign anal disease with topical nitroglycerin. Dis Colon Rectum 1995;38:453–7.
Author information
Authors and Affiliations
Additional information
Dr. Park was a visiting colorectal surgeon from the Section of Colon and Rectal Surgery, Department of Surgery, College of Medicine, Kon-Kuk University Hospital, Chung Ju, Korea.
About this article
Cite this article
Park, U.C., Choi, S.K., Piccirillo, M.F. et al. Patterns of anismus and the relation to biofeedback therapy. Dis Colon Rectum 39, 768–773 (1996). https://doi.org/10.1007/BF02054442
Issue Date:
DOI: https://doi.org/10.1007/BF02054442