Abstract
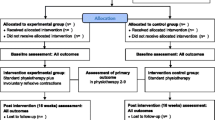
The authors compared intensive pelvic floor exercise alone (A) with intensive pelvic floor exercise plus vaginal cones (B) in premenopausal women with mild to moderate stress urinary incontinence. Forty-six patients (mean 43±6 years) were randomized into two training groups and treated for 3 months. Pre- and post-therapy urethral pressure profiles at rest and under stress and subjective results were obtained from 29 patients. The subjective improvement rate of the compliant patients after 12 weeks was 85% in group A and 84% in group B. When the dropouts (9 in group A and 8 in group B) were included in the subjective results an overall improvement rate of 48% in group A and 52% in group B was obtained. In group A one pressure transmission ratio (PTR) improved significantly at 6 weeks and the position of maximum urethral closure pressure was shifted proximally at 12 weeks. In group B one PTR in the midurethra was improved significantly at 6 weeks. The other urodynamic parameters were unchanged. There were no differences between groups A and B in subjective results or urodynamic findings. These results suggest that intensive pelvic floor exercise with or without vaginal cones improves the symptoms of mild to moderate stress incontinence in about 85% of premenopausal women, but that it has little effect on urodynamic parameters. Vaginal cones provided no additional benefit but may be useful for women for whom closely supervised pelvic floor exercise is not available.
Similar content being viewed by others
References
Kegel AH. Physiologic therapy for urinary stress incontinence.JAMA 1951;146:915–917
Wilson PD, Al Samarrai T, Deakin M, Kolbe E, Brown ADG. An objective assessment of physiotherapy for female stress incontinence.Br J Obstet Gynaecol 1987;94:575–582
Henella SM, Kirwan P, Castleden CM, Hutchins CJ, Breeson AJ. The effect of pelvic floor exercise in the treatment of genuine stress incontinence in women at two hospitals.Br J Obstet Gynaecol 1988;95:602–608
Klarskov P, Belving D, Bischoff N. Pelvic floor exercise versus surgery for female urinary stress incontinence.Urol Int 1986;41:129–132
Klarskov P, Kroyer K, Kromann S, Maegaard E. Long term results of pelvic floor training and surgery for female genuine stress incontinence.Neurourol Urodyn 1989;8:357–359
Plevnik S. New method for testing and strengthening of pelvic floor muscles. In: Proceedings of the 15th annual meeting of the International Continence Society 1985;267–268
Peattie AB, Plevnik S, Stanton SL. Vaginal cones: a conservative method of treating genuine stress incontinence.Br J Obstet Gynaecol 1988;95:1049–1053
Jonasson A, Larsson B, Pschera H. Testing and training of the pelvic floor muscles after childbirth.Acta Obstet Gynaecol Scand 1989;68:301–304
Haken JA, Benness C, Cardozo L, Cutner A. A randomized trial of vaginal cones and pelvic floor exercises in the management of genuine stress incontinence.Neurourol Urodyn 1991;10:393–394
Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardization of terminology of lower urinary tract function recommended by the International Continence Society.Int Urogynecol J 1990;1:45–58.
Mouritsen L, Frimodt-Moller C, Moller M. Long term effect of pelvic floor exercise on female urinary incontinence.Br J Urol 1991;68:32–37
DeLancey JOL. Correlative study of paraurethral anatomy.Obstet Gynecol 1986;68:91–97
DeLancey JOL. Structural aspects of the extrinsic continence mechanism.Obstet Gynecol 1988;72:296–301
Bo K, Hagen R, Kvarstein B, Larsen S. The effect of two different pelvic floor muscle exercise programs in treatment of urinary stress incontinence in women.Neurourol Urodyn 1989;8:355–356
Ferguson KL, McKey PL, Bishop KR, Kloen P, Verheul JB, Dougherty MC. Stress urinary incontinence: effect of pelvic muscle exercise.Obstet Gynecol 1990;75:671–673
Moore K, Metcalfe JB. Effectiveness of vaginal cones in treatment of urinary incontinence.Urol Nursing 1992;12:69–72
Tchou DCH, Adams C, Varner RE, Denton B. Pelvic floor musculature exercises in treatment of anatomical urinary stress incontinence.Phys Ther 1988;68:652–655
Kujansuu E. The effect of pelvic floor exercises on urethral function in female stress urinary incontinence: a urodynamic study.Ann Chir Gynecol 1983;72:28–32
Author information
Authors and Affiliations
Additional information
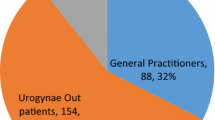
Editorial Comment: It is becoming increasingly clear from the literature that pelvic floor muscle exercises are effective in improving continence in many women with straightforward stress incontinence. An appropriate quest continues to determine how the exercises can best be taught and done. This article demonstrates that with frequent supervision, similar continence status is achieved both with and without the use of vaginal cones. It would be interesting to compare outcomes with and without cones in women who saw a health care provider only once for their initial teaching. If cones were found to be more effective in this setting, that would be a great aid to primary care physicians.
The authors state that there was no correlation between the cone weight and the degree of improvement of symptoms: however, only 2 of the subjects progressed to ‘the next heaviest cone weight’. My understanding of the principles of athletic muscles training is that as one increases the resistance the muscle fibers hypertrophy and strengthen. This is the principle behind building biceps. Body-builders or power-lifters continue to increase the amount of weight (resistance) they lift in order to increase bulk and strength. I wonder if this same principle is the reason for the differences in results between this study and the one by Peattie et al. quoted by the authors. My major concern is that people begin to devalue the amount of effort required to perform effective pelvic floor exercises and make assumptions that such exercises are not as good as a ‘permanent surgical cure’. I believe that we have not yet begun to develop really effective muscle strengthening regimens for the pelvic floor, and attitudes such as the above will only serve to inhibit our progress.
Rights and permissions
About this article
Cite this article
Pieber, D., Zivkovic, F., Tamussino, K. et al. Pelvic floor exercise alone or with vaginal cones for the treatment of mild to moderate stress urinary incontinence in premenopausal women. Int Urogynecol J 6, 14–17 (1995). https://doi.org/10.1007/BF01961842
Issue Date:
DOI: https://doi.org/10.1007/BF01961842