Abstract
A 4.5-year-old boy received a combined liver and kidney transplant for correction of hyperoxaluria type 1. Both organs were from the same donor and functioned primarily. Three months after transplantation, urine oxalate excretion reached a maximum of 10500 μmol/24 h and remained above 2300 μmol/24 h for the next 2 months. Two months later, oxalate excretion decreased to about 565 μmol/24 h, indicating exhaustion of a large oxalate pool. Six months after transplantation plasma oxalate is near normal (4.9 μmol/l). With the exception of one episode of acute rejection of the renal transplant, both organs were tolerated well and continue to have a unimpaired function 9 months after transplantation. However, there is increased echogenity on renal ultrasound, indicating oxalate deposits in the grafted kidney. This case illustrates that successful combined transplantation of both liver and kidney can be performed in infants, resulting in cure of the metabolic defect. The prolonged or acute excretion of oxalate may lead to oxalate deposition in the grafted kidney without impaired graft function or early graft loss.
Similar content being viewed by others
Abbreviations
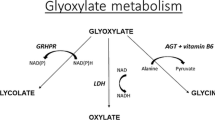
- AGT:
-
alanine: glyoxalate aminotransferase
- CyA:
-
cyclosporine A
- PHI:
-
primary hyperoxaluria type I
- TPL:
-
transplantation
- U-Ox:
-
urinary oxalate
References
Broyer M, Brunner FP, Brynger H, Dykes SR, Ehrich JHH, Fassbinder W, Geerlings W, Rizzoni G, Selwood NH, Tufevson G, Wing AJ (1990) Kidney transplantation in primary oxalosis: data from the EDTA registry. Nephrol Dial Transplant 5:332–336
Cochat P, Faure JL, Divry P, Danpure CJ, Descos B, Wright C, Takvorian P, Floret D (1989) Liver transplantation in primary hyperoxaluria type 1. Lancet I:1142–1143
Danpure CJ (1989) Recent advances in the understanding of primary hyperoxaluria type 1. J Inherited Metab Dis 12:210–224
Danpure CJ, Jennings PR (1986) Peroxisomal alanine: glyoxalate aminotransferase deficiency in primary hyperoxaluria type 1. FEBS Lett 201:20–24
Frosch M, Kuwertz-Bröking E, Bulla M, Bassewitz DB von, Leusmann DB (1989) Oxalose Typ 1 im Kindesalter — Beobachtungen im Rahmen der terminalen Niereninsuffizienz beim Kind. Klin Wochenschr 67:1156–1167
Hillman RE (1989) Primary hyperoxalurias. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic basis of inherited disease, vol 1. McGraw-Hill, New York, pp 933–944
Kasidas GP, Rose GA (1986) Measurements of plasma oxalate in healthy subjects and in patients with chronic renal failure using immobilised oxalate oxidase. Clin Chim Acta 154:49–58
Katz A, Kim Y, Scheinman J, Najarian JS, Mauer SM (1989) Long-term outcome of kidney transplantation in children with oxalosis. Transplant Proc 21:2033–2035
Leumann EP, Niederwieser A, Fanconi A (1987) New aspects of infantile oxalosis. Pediatr Nephrol 1:531–535
McDonald JC, Landreneau MD, Rohr MS, Devault GA (1989) Reversal by liver transplantation of the complications of primary hyperoxaluria as well as the metabolic defact. N Engl J Med 321:1100–1103
Morgan SH, Watts RWE (1989) Perspectives in the assessment and management of patients with primary hyperoxaluria type I. Adv Nephrol 18:95–106
Schürmann G, Schärer K, Wingen AM, Otto G, Herfarth C (1990) Early liver transplantation for primary hyperoxaluria type 1. Nephrol Dial Transpl (in press)
Wanders RJA, Ruiter J, Roermund CWT van, Ofman R, Schutgens RBA, Jurrians S, Tager JM (1990) Human liverl-alanine: glyoxalate aminotransferase: characteristics and activity in controls and hyperoxaluria type 1 patients using a simple spectrophotometric method. Clin Chim Acta (in press)
Watts RWE, Calne RY, Williams R, Mansell MA, Veall N, Purkiss P, Rolles K (1985) Primary hyperoxaluria (type 1) attempted treatment by combined hepatic and renal transplantation. Q J Med 57:697–793
Watts RWE, Calne RY, Rolles K, Danpure CJ, Morgan SH, Mansell MA, Williams R, Purkiss P (1987) Successful treatment of primary hyperoxaluria type 1 by combined hepatic and renal transplant. Lancet II:474–475
Watts RWE, Morgan SH, Purkiss P, Mansell MA, Baker LRI, Brown CB (1988) Timing of renal transplantation in the management of pyridoxine-resistant type 1 primary hyperoxaluria. Transplantation 45:1143–1145
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ruder, H., Otto, G., Schutgens, R.B.H. et al. Excessive urinary oxalate excretion after combined renal and hepatic transplantation for correction of hyperoxaluria type 1. Eur J Pediatr 150, 56–58 (1990). https://doi.org/10.1007/BF01959482
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01959482