Abstract
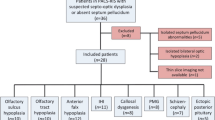
Septo-optic dysplasia (SOD) is characterized by hypoplasia of the optic nerve, various types of forebrain defects and hormonal deficiencies. We have studied the clinical and endocrinological characteristics of 18 such patients retrospectively to: (1) better define the endocrine abnormalities in children with SOD; and (2) to find approaches for the interdisciplinary long-term care of children with SOD. The children were seen at the Children's Hospital of the University of Munich from 1976 to 1992 (8 boys, 10 girls; age at initial presentation: 1 day–13 years of age, mean 1.9 years). Unilateral hypoplasia of the optic nerve was found in 7 cases, bilateral hypoplasia in 11. Sonographic, CCT or MRI yielded the following results: 4 of the patients had a cavum septum pellucidum, 3 patients had hypoplasia of the cerebellum, 1 aplasia of the corpus callosum and 1 aplasia of the fornix. An empty sella with or without an ectopic pituitary was seen in 4 cases. Height standard deviation score (SDS) at time of diagnosis was −4.0 to +0.4, mean −2.92. Endocrine deficiencies were present in all 11 patients who had undergone endocrinological investigations. Seven patients suffered from isolated growth hormone (GH) deficiency or multiple hypopituitarism. One had diabetes insipidus centralis, 2 had hypogonadotropic hypogonadism, 1 had hypothyroidism and 2 adrenal insufficiency. Hypothalamic testing was performed only in a subset of patients: in 5 of 11 children tested a thyrotropin releasing hormone (TRH test), in two out of nine a gonadotropin releasing hormone (GnRH) test, and in three out of six GH releasing hormone (GHRH) test yielded abnormal results. High prolactin levels were measured in two out of five patients.
Conclusion
SOD is characterized by optic nerve hypoplasia and a variety of endocrine deficiencies. In addition, forebrain malformations are present in most SOD patients. Hormonal disorders are present in some SOD patients which may be of hypothalamic origin and need to be investigated systematically.
Similar content being viewed by others
Abbreviations
- CRH :
-
corticotropin releasing hormone
- FSH :
-
follicle stimulating hormone
- GH :
-
growth hormone
- GHRH :
-
growth hormone releasing hormone
- GnRH :
-
gonadotropin releasing hormone
- IGF-I :
-
insulin-like growth factor-I
- LH :
-
luteinizing hormone
- SOD :
-
septo-optic dysplasia
- TRH :
-
thyrotropin releasing hormone
References
Arslanian SA, Rothfus WE, Foley TP, Becker DJ (1984) Hormonal, metabolic and neuroradiologic abnormalities associated with Septo-optic Dysplasia. Acta Endocrinol 107: 282–288
Barkyvich AJ, Fram EK, Norman D (1989) Septo-optic dysplasia: MR imaging. Radiology 171: 189–192
Bellastella A, Parlato F, Sinisi AA (1990) Blindness impairs plasma growth hormone response to L-Dopa but not to Arginine. J Clin Endocrinol Met 70: 856–858
Billson F, Hopkins IJ (1972) Optic hypoplasia and hypopituitarism. Lancet I: 905
Bohlayer R, Straßburg HM, Sauer M (1983) Das Cavum Septi Pellucidi und Cavum Vergae beim Säugling — Eine Untersuchung mit der zweidimensionalen Sektor-Echo-Enzephalographie. Klin Pädiatr 195: 92–96
Costin G, Linn MA (1985) Hypothalamic-pituitary function in children with optic nerve hypoplasia. Am J Dis Child 139: 249–254
Davis GV, Shock JP (1975) Septo-optic dysplasia associated with see-saw nystagmus. Arch Ophthalmol 93: 137–139
Deeg KH, Bundscherer F, Böwing B (1986) Zerebrale Ultraschalldiagnostik bei Hirnmißbildungen. Monatsschr Kinderheilkd 134: 738–747
Edwards WC, Layden WE (1970) Optic nerve hypoplasia. J Ophthal 70: 950–959
Ellenberger C, Runyan TE (1970) Holoprosencephaly with hypoplasia of the optic nerves, dwarfism, and agenesis of the septum pellucidum. Am J Ophthalmol 70: 960–967
Elster AB, McAnarney ER (1979) Maternal age re septo-optic dysplasia. J Pediatr 93: 162
Hanna CE, LaFranchi SH (1983) Evolving hypopituitarism in children with central nervous system lesions. Pediatrics 72: 65–70
Hanna CE, Mandel SH, La Franchi SH (1989) Puberty in the syndrome of Septo-optic Dysplasia. Am J Dis Child 143: 186–189
Hoyt WF, Kaplan SL, Grumbach MM, Glaser JS (1970) Septo-optic dysplasia and pituitary dwarfism. Lancet 1: 893–894
Huseman CA, Kelch RP, Hopwood NJ, Zipf WB (1978) Sexual precocity in association with septo-optic dysplasia and hypothalamic hypopituitarism. J Pediatr 92: 748–753
Izenberg N, Rosenblum M, Parks JS (1984) The endocrine spectrum of Septo-optic dysplasia. Clin Paediatr 23: 632–636
Jellinger K, Gross H (1973) Congenital telencephalic midline defects. Neuropädiatrie 4: 446–452
Kewitz G, Girard J, Probst A, Olafsson A, Vest M, Hirt HR, Periat P, Forrer A, Daicker B, Wieser D, Boss M (1984) Septo-optic pituitary dysplasia. Helv Paediatr Acta 39: 355–364
Kitamura M, Namiki M, Okuyama A, Arita N, Mizutani S, Sonoda T (1988) Isolated gonadotropin deficiency secondary to glioma in septum pellucidum. Urol Int 43: 122–124
Kobori JA, Herrick MK, Urich H (1987) Arhinencephaly — the spectrum of associated malformations. Brain 110: 237–260
Kraus EJ (1919) Zur Kenntnis der Nanosomie. Beitr Pathol Anat Allg Pathol 65: 535–546
Kuban KCK, Littlewood Teele R, Wallmann J (1989) Septo-optic-dysplasia-schizencephaly. Pediatr Radiol 19: 145–150
Manelfe C, Rochiccioli P (1979) CT of septo-optic dysplasia. Am J Radiol 133: 1157–1160
Margalith D, Jan JE, McCormick AQ, Tze WJ, Lapointe J (1984) Clinical spectrum of congenital optic nerve hypoplasia: review of 51 patients. Dev Med Child Neurol 26: 311–322
Margalith D, Tze WJ, Jan JE (1985) Congenital optic nerve hypoplasia with hypothalamic-pituitary dysplasia. A review of 16 cases. Am J Dis Child 139: 361–366
Morgan SA, Emsellem HA, Sandler JR (1985) Absence of the septum pellucidum: overlapping clinical syndromes. Arch Neurol 42: 769–770
O'Dwyer JA, Newton TH, Hoyt WF (1980) Radiologic features of septo-optic daysplasia: de Morsier syndrome. Am J Neuroradiol 1: 443–447
Ohzeki T, Hanaki K, Asano T, Ishitani N, Wakatsuki H, Shiraki K (1986) Hypodipsic hypernatremia associated with absence of septum lucidum and olfactory dysfunction. Acta Paediatr Scand 75: 1046–1050
Patel H, Tze WJ, Crichton JU, McCormick AQ, Robinson GC, Dolman CL (1975) Optic nerve hypoplasia with hypopituitarism. Am J Dis Child 129: 175–180
Polomeno RC, Staudenmaier C, Guyda HJ, Little JM (1980) Ocular defects and short stature. Can J Ophthalmol 15: 125–130
Prader A, Largo RH, Molinari L, Issler C (1989) Physical growth of Swiss children from birth to 20 years of age. First Zurich longitudinal study of growth and development. Helv Paediatr Acta [Suppl] 52: 1–125
Rabl W, Müller OA, Roggenkämper P, Stünkel S, Werder K von (1988) Neuroendokrine Insuffizienz und Funktionsdiagnostik: Die septo-optische Dysplasie als Modell. Pädiatrie 1,2: 114–123
Roberts-Harry J, Green SH, Wilshaw HE (1990) Optic nerve hypoplasia: associations and management. Arch Dis Child 65: 103–106
Roessmann U, Velasco ME, Small EJ, Hori A (1987) Neuropathology of septo-optic dysplasia (de Morsier syndrome) with immunohistochemical studies of the hypothalamus and pituitary gland. J Neuropathol Exp Neurol 46: 597–608
Rush JA, Bajandas FJ (1978) Septo-optoc dysplasia (De Morsier syndrome) Am J Ophthalmol 86: 202–205
Stanhope R, Preece MA, Brook CGD (1984) Hypoplastic optic nerves and pituitary dysfunction. A spectrum of anatomical and endocrine abnormalities. Arch Dis Child 59: 111–114
Stewart C, Castro-Magana M, Sherman J, Angulo M, Collipp PJ (1983) Septo-optic dysplasia and median cleft face syndrome in a patient with isolated growth hormone deficiency and hyperprolactinemia. Am J Dis Child 137: 484–487
Strasser B, Holthausen H, Egger J, Belohradsky B, Dörr H (1987) Neurohormonelle Störungen bei Kindern mit Septo-optischer Dysplasia. Literatur-übersicht und eigene Beobachtungen. Aktuelle Neuropädiatrie 1986, H Fichsel (Hrsg.) Springer Verlag Berlin Heidelberg, pp 148–152
Walton DS, Robb RM (1970) Optic nerve hypoplasia: a report of 20 cases. Arch Ophthalmol 84: 572–576
Wilson DM, Enzmann DR, Hintz RL, Rosenfeld RG (1984) Computed tomographic findings in septo-optic dysplasia: discordance between clinical and radiological findings. Neuroradiology 26: 279–283
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Willnow, S., Kiess, W., Butenandt, O. et al. Endocrine disorders in septo-optic dysplasia (De Morsier syndrome) — evaluation and follow up of 18 patients. Eur J Pediatr 155, 179–184 (1996). https://doi.org/10.1007/BF01953934
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01953934