Summary
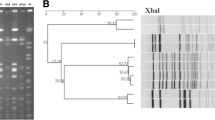
The first outbreak of infections caused by an SHV-5 producing strain ofKlebsiella pneumoniae is reported. Within a period of 1 year and 9 months, multiresistantK. pneumoniae strains caused severe infections, mostly of the lower respiratory tract, in 22 patients. The strains were resistant to penicillins, third-generation cephalosporins, aztreonam, chloramphenicol, tetracycline and co-trimoxazole. The resistance determinants were transferable toEscherichia coli. All isolates produced a beta-lactamase with a pI of 8.2. Ceftazidime was hydrolyzed at this band. These characteristics, together with the resistance phenotype, are identical to those of a reference strain producing the beta-lactamase SHV-5. TheK. pneumoniae strains of all patients were identical in their capsular serotype (K1), plasmid pattern and plasmid fingerprint after digestion with Dra I restriction endonuclease. We conclude that this outbreak was caused by the spread of one clone ofK. pneumoniae producing SHV-5 beta-lactamase among patients of different wards. Our results indicate a real risk for failure of therapy by third-generation cephalosporins in intensive care patients due to SHV-5 producing pathogens.
Zusammenfassung
Wir berichten über das in Deutschland erstmalig gehäufte Auftreten von Infektionen verursacht durch einen Stamm vonKlebsiella pneumoniae, der die plasmidische Betalaktamase SHV-5 produziert. Innerhalb eines Beobachtungszeitraumes von einem Jahr und neun Monaten verursachte dieser Stamm bei 22 Patienten schwere nosokomiale Infektionen zumeist der tiefen Atemwege. Der Erreger war resistent gegenüber Penicillinen, Cephalosporinen der dritten Generation, Aztreonam, Chloramphenicol, Tetrazyklin und Co-trimoxazol. Die Resistenzdeterminanten waren aufEscherichia coli übertragbar. Alle Isolate produzierten eine Betalaktamase mit einem isoelektrischen Punkt von 8,2, die Ceftazidim hydrolysierte. Diese Merkmale zusammen mit dem Resistenz-Phänotyp sind identisch mit denen eines mitgeführten Referenzstammes, der die Betalaktamase SHV-5 produziert. AlleK. pneumoniae-Stämme waren identisch in ihrem Kapsel-Serotyp, ihrem Plasmidmuster und ihrem Plasmid-Fingerprint (nach Verdauen mit der Restriktionsendonuclease Dra I). Wir schließen daraus, daß dieser Ausbruch von Infektionen durch einen einzigen Klon eines betalaktamase-produzierendenK. pneumoniae-Stammes verursacht wurde, der sich über verschiedene Stationen verbreitete. Diese Ergebnisse signalisieren das Risiko von Therapiemißerfolgen in Deutschland bei empirischem Einsatz von Drittgenerations-Cephalosporinen bei Infektionen mitK. pneumoniae.
Similar content being viewed by others
References
Bauernfeind, A., Casellas, J. M., Goldberg, M., Holley, M., Jungwirth, R., Mangold, P., Röhnisch, T., Schweighart, S., Wilhelm, R. A new plasmidic cefotaximase from patients infected withSalmonella typhimurium. Infection 20 (1992) 158–163.
Miller, G. H., Sabatelli, F. J., Hare, R. S., Waitz, J. A. Survey of aminoglycoside resistance patterns. Dev. Ind. Microbiol. 21 (1980) 91–104.
Bauernfeind, A., Petermüller, C., Schneider, R. Bacteriocins as tools in analysis of nosocomialKlebsiella pneumoniae infections. J. Clin. Microbiol. 14 (1981) 15–19.
Palfreyman, U. Klebsiella serotyping by counter current immunoelectrophoresis. J. Hyg. 81 (1978) 219–225.
Gutmann, L., Ferré, B., Goldstein, F. W., Rizk, N., Pinto-Schuster, E., Acar, J. F., Collatz, E. SHV-5, a novel SHV-type β-lactamase that hydrolyzes broad-spectrum cephalosporins and monobactams. Antimicrob. Agents Chemother. 33 (1989) 951–956.
Knothe, H., Shah, P., Krčméry, V., Antal, M., Mitsuhashi, S. Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates ofKlebsiella pneumoniae andSerratia marcescens. Infection 11 (1983) 315–317.
Shah, P. M., Stille, W. Escherichia coli andKlebsiella pneumoniae strains more susceptible to cefoxitin than to third generation cephalosporins. J. Antimicrob. Chemother. 11 (1983) 597–601.
Bauernfeind, A., Shah, P., Petermüller, C., Motz, M.: Plasmid-determined resistance to third generation cephalosporins in enterobacteria. Proceedings of the IV Mediterranean Congress of Chemotherapy, 1984, pp. 30–31.
Jacoby, G., Medeiros, T. More extended-spectrum β-lactamases. Antimicrob. Agents Chemother. 35 (1991) 1697–1704.
Matthew, M., Harris, A. M., Marshall, M. J., Ross, G. W. The use of analytical isoelectric focussing for detection and identification of β-lactamases. J. Gen. Microbiol. 88 (1975) 169–178.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bauernfeind, A., Eberlein, E., Holley, M. et al. Spread ofklebsiella pneumoniae producing SHV-5 beta-lactamase among hospitalized patients. Infection 21, 18–22 (1993). https://doi.org/10.1007/BF01739303
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01739303