Abstract
Objective
To investigate the accuracy of eight different prognostic scores (Stiehm, Niklasson, Leclerc, Garlund, the MOC score, Tesero, the Glasgow Meningococcal Septicaemia Prognostic Score (GMSPS) and Tüyzüs) in the prediction of fatal outcome in meningococcal disease.
Design
Combined prospective and retrospective study.
Setting
A 175-bed pediatric department of a university hospital providing secondary care to ±180,000 inhabitants and serving as a referral center. The Pediatric Intensive Care (14 beds) is one of the six PICUs in the Netherlands and provides tertiary care for children under 18 years.
Patients
During an 8-year period (1986–1994) 125 children (mean age 4 years, 10 months) with culture-proven meningococcal disease were studied: 34 patients presenting with meningitis, 33 patients with septic shock and 58 patients with meningitis and septic shock.
Main results
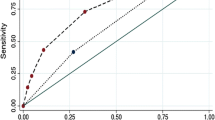
All eight scores discriminated above average between survivors and non-survivors, as expressed by the corresponding Receiver Operator Characteristic (ROC) curves. The area under the ROC curve (AUC) ranged from 0.74 for the Garlund score to 0.93 for the GMSPS. The GMSPS performed significantly better than its competitors, even after exclusion of the base deficit as one of the score components (AUC=0.92). It showed above average calibration when logistically transformed into a probability of mortality, and accurately identified a subgroup of patients with no mortality. None of the scores correctly identified non-survivors.
Conclusion
The GMSPS is a simple score that can be reliably used for risk classification and the identification of low-risk patients.
Similar content being viewed by others
References
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE—acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9:591–597
Pollack MM, Ruttiman UE, Getson PR (1988) Pediatric risk of mortality (PRISM) score. Crit Care Med 16: 1110–1116
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, Harrell FE (1991) The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100:1619–1636
Baumgartner JD, Büla C, Vaney C (1992) A novel score for predicting mortality of septic shock patients. Crit Care Med 20:953–960
Hebert PC, Drummond AJ, Singer J (1993) A simple multiple organ failure scoring system predicts mortality of patients who have sepsis syndrome. Chest 104:230–235
Knaus WA, Harrell FE, Fisher CJ (1993) The clinical evaluation of new drugs for sepsis. A prospective study design based on survival analysis. JAMA 270:1233–1241
Bone RC, Fisher CJ Jr, Clemmer TP, Slotman GJ, Metz CA, Balk RA (1989) Sepsis syndrome: a valid clinical entity. Crit Care Med 17:389–394
Barriere SL, Lowry SF (1995) An overview of mortality risk prediction in sepsis. Crit Care Med 23:376–393
Stiehm ER, Damrosch DS (1966) Factors in the prognosis of meningococcal infection. J Pediatr 68:457–467
Niklasson P, Lundbergh P, Strandell T (1971) Prognostic factors in meningococcal disease. Scand J Infect Dis 3: 17–25
Leclerc F, Beuscart R, Guillois B, Diependaele JF, Krim G, Devictor D (1985) Prognostic factors of severe infectious purpura in children. Intensive Care Med 11:140–143
Garlund B (1986) Prognostic evaluation in meningococcal disease. A retrospective study of 115 cases. Intensive Care Med 12:302–307
Gedde-Dahl TW, Bjark P, Høiby EA, Høst JH, Bruun JN (1990) Severity of meningococcal disease: Assessment by factors and scores and implications for patient management. Rev Inf Dis 12: 973–992
Tesoro LJ, Selbst SM (1991) Factors affecting outcome in meningococcal infections. Am J Dis Child 145:218–220
Sinclair JF, Skeoch CH, Hallworth D (1987) Prognosis of meningococcal septicaemia. Lancet ii:38
Thomson APJ, Sills JA, Hart CA (1991) Validation of the Glasgow Meningococcal Septicaemia Prognostic Score: a 10-year retrospective survey. Crit Care Med 19:26–30
Tüysüz B, özlü I, Ali DY, Erginel A (1993) Prognostic factors in meningococcal disease and a new scoring system. Acta Paediatr 82:1053–1056
Kahn A, Blum D (1978) Factors for poor prognosis in fulminating meningococcemia. Conclusions from observations of 67 childhood cases. Clin Pediatr 17:680
Stokland T, Flaegstad T, Gutteberg TJ (1985) A clinical score for the prediction of outcome of patients with meningococcal infection. Acta Paediatr Scand 322:12
Gray R, Begg CB, Greenes RA (1984) Construction of Receiver Operating Characteristic Curves when disease verification is subject to selection bias. Med Decis Making 4:151–164
Sox HC, Blatt MA, Higgins MC, Marton KI (1988) Medical decision-making. Butterworth, Boston.
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148: 839–843
Lemeshow S, Klar J, Teres D (1995) Outcome prediction for individual intensive care patients: useful, misused, or abused? Intensive Care Med 21: 770–776
Gemke JBJ, Bonsel GJ, Vught JA van (1994) Effectiveness and efficiency of a Dutch pediatric intensive care unit: validity and application of the pediatric risk of mortality (PRISM) score. Crit Care Med 22:1477–1484
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Derkx, H.H.F., van den Hoek, J., Redekop, W.K. et al. Meningococcal disease: A comparison of eight severity scores in 125 children. Intensive Care Med 22, 1433–1441 (1996). https://doi.org/10.1007/BF01709565
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01709565