Abstract
Thirteen children, aged 2 to 16 years, had a subtotal resection of small bowel, following a mid-gut volvulus in 10 cases. All children are alive, and their growth is normal; 36 cumulative patient-years of parenteral nutrition and 11 years of constant-rate enteral nutrition were performed. In 7 cases, in which residual small bowel varied between 30 to 120 cm, termination of all artificial nutritional support was possible 30 months in mean after intestinal resection. In contrast, if resection was near total with less than 20 cm remaining, life-long dependence on parenteral nutrition is unavoidable unless intestinal transplantation becomes feasible. With cyclic parenteral nutrition at home, the patients' quality of life is near normal.
Résumé
Treize enfants âgés de 2 à 16 ans ont subi une résection subtotale de l'intestin grêle dont 10 pour volvulus de sa partie moyenne. Tous ont survécu leur croissance s'étant effectuée normalement. Le total en années de la nutrition parentérale qu'ils ont reçu s'élève à 36 ans. Dans 7 cas, où la longueur du segment intestinal restant variait entre 30 et 120 cm, il fut possible d'arrêter l'alimentation parentérale 30 mois en moyenne après la résection. En revanche si la résection est quasi totale, la longueur du segment de grêle conservé étant inférieure à 20 cm, le maintien permanent de l'alimentation parentérale est inévitable à moins que la transplantation intestinale ne devienne possible. Grâce à l'alimentation parentérale organisée à domicile, la qualité de vie de ces sujets est presque normale.
Resumen
Trece niños de edades entre los 2 y los 16 años han sido sometidos a resección subtotal del intestino delgado, como consecuencia de vólvolus del intestino medio en 10 casos. Todos los niños se encuentran vivos y su crecimiento es normal; ellos representan 36 años-pacientes acumulados de nutrición parenteral y 11 años de nutrición enteral a tasa constante. En siete casos en quienes el intestino residual media entre 30 y 120 cm, fué posible terminar todo tipo de soporte nutricional artificial a los 30 meses, en promedio, después de realizada la resección intestinal. Por el contrario, si la resección fué casi total con menos de 20 cm de intestino residual, la dependencia vitalicia de nutrición parenteral es inevitable, a menos que el transplante intestinal llegue a ser factible. Mediante la nutrición parenteral cíclica realizada a domicilio, la calidad de la vida de estos pacientes llega a ser casi normal.
Similar content being viewed by others
References
Ricour, C., Duhamel, J.F.: Nutritional problems. In Care of the Critically Ill Patient, J. Tinker, M. Rapin, editors. Berlin-Heidelberg-New York, Springer-Verlag, 1983, pp. 1087–1103.
Ricour, C., Revillon, Y., Bougle, D., et al.: Nutrition parenterale par fistule arterio-veineuse. Arch. Fr. Pédiatr.40:457, 1983
Ricour, C., Duhamel, J.F., Revillon, Y., et al.: Une nouvelle approche nutritionnelle: La nutrition parenterale exclusive discontinue chez l'enfant. Arch. Fr. Pédiatr.35:918, 1978
Ricour, C., Maurage, C., Duhamel, J.F., et al.: Nutrition artificielle et résection étendue du grêle chez le nourrisson. Gastroenterol. Clin. Biol.6:294, 1982
Bohane, T.D., Haka-Ikse, K., Biggar, W.D., Hamilton, J.R., Gall, D.G.: A clinical study of young infants after small intestinal resection. J. Pediatr.94:552, 1979
Wilmore, D.W.: Factors correlating with a successful outcome following extensive intestinal resection in newborn infants. J. Pediatr.80:88, 1972
Krejs, G.J.: The small bowel. Part I. Intestinal resection. Clin. Gastroenterol.8:373, 1979
Weser E.: The management of patients after small bowel resection. Gastroenterology71:146, 1976
Walman, H.B.: Growth and fat absorption after resection of ileum in childhood. J. Pediatr.88:41, 1976
Cosnes, J., Gendre, J.P., Le Quintrec, Y.: Role of the ileocecal valve and site of intestinal resection in malabsorption after extensive small bowel resection. Digestion18:329, 1978
Mitchell, J.E., Breuer, R.I., Zuckerman, L., Berlin, J., Schilli, R., Dunn, J.K.: The colon influence ileal resection diarrhea. Dig. Dis. Sci.25:33, 1980
Ricour, C., Harouchi, A., Parc, R., et al.: Résection subtotale du grêle chez le porcelet et nutrition parenterale. Resultats préliminaires. Ann. Anesth. Fr.2:19, 1974
Dowling, R.H.: The influence of luminal nutrition on intestinal adaptation after small bowel resection and by-pass. In Intestinal Adaptation, R.H. Dowling, E.O. Riecken, editors. New York, Stuttgart, F.K. Schattauer Verlag, 1974, pp. 35–46
Feldman, E.J., Dowling, R.H., McNaughton, J., Peters, T.J.: Effects of oral versus intravenous nutrition on intestinal adaptation after small bowel resection in the dog. Gastroenterology70:712, 1976
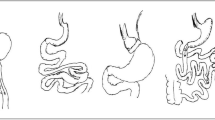
Kalifa, G., Devred, P., Ricour, C., et al.: Radiological aspects of the small bowel after extensive resection in children. Pediatr. Radiol.8:70, 1979
Morin, C.L., Ling, V., Van Caillie, M.: Role of oral intake on intestinal adaptation after small bowel resection in growing rats. Pediatr. Res.12:268, 1978
Schmitz, J., Rey, F., Bresson, J.L., et al.: Etude par perfusion intestinale de l'absorption des sucres après résection étendue du grêle. Arch. Fr. Pédiatr.37:491, 1980
Williamson, R.C.N.: Intestinal adaptation. N. Engl. J. Med.298:1393, 1978
Wittman, T., Crenner, F., Felder, G., et al.: Motricité intestinale après résection jejunale: étude electromyographique chez le rat. Gastroenterol. Clin. Biol.8:414, 1984
Weser, E., Heller, R., Tawil, T.: Stimulation of mucosal growth in the rat by bile and pancreatic secretions after jejunal resection. Gastroenterology73:524, 1977
Weser, E., Bell, D., Tawil, T.: Effects of octapeptide-cholecystokinin secretin, and glucagon on intestinal mucosal growth in parenterally nourished rats. Dig. Dis. Sci.26:409, 1981
Lauritsen, K.B., Moody, A.J., Christensen, K.C., et al.: Gastric inhibitory polypeptide (GIP) and insulin release after small bowel resection in man. Scand. J. Gastroenterol.15:833, 1980
Besterman, H.S., Adrian, T.E., Mallinson, C.N., Christofides, N.D., Sarson, D.L., Pera, A., Lombardo, L., Modigliani, R., Bloom, S.R.: Gut hormone release after intestinal resection. Gut23:854, 1982
Ricour, C.: Utilisation de la cholestyramine et des triglycerides à chaîne moyenne dans les résections ileales chez l'enfant. Acta Gastroenterol. Belg.36:78, 1973
Remington, M., Fleming, C.R., Malagelada, J.R.: Inhibition of postprandial pancreatic and biliary section by loperamide in patients with short bowel syndrome. Gut23:98, 1982
Ghnassia, J.C., Ricour, C., Duhamel, J.F., et al.: Flore bactérienne duodenale de l'enfant au cours des stases post chirurgicales. Arch. Fr. Pédiatr.35:854, 1978
King, C.E., Toskes, P.P.: Small intestine bacterial overgrowth. Gastroenterology76:1035, 1979
Maini, B., Blackburn, G.L., Bistrian, B.R., et al.: Cyclic hyperalimentation: An optimal technique for preservation of visceral protein. J. Surg. Res.20:515, 1976
Putet, G., Bresson, J.L., Ricour, C.: Nutrition parenterale exclusive chez l'enfant: Influence de l'apport continu ou cyclique sur l'utilisation des nutriments. Arch. Fr. Pédiatr.41:111, 1984
Cannon, R.A., Byrne, W.J., Ament, M.E., Gates, B., O'Connor, M., Fonkalsrud, E.W.: Home parenteral nutrition infants. J. Pediatr.96:1098, 1980
Buxton, B.: Small bowel resection and gastric acid hypersecretion. Gut15:229, 1974
Barros, D'Sa A.A.B., Buchanan, K.D.: Role of gastrointestinal hormones in the response to massive resection of small bowel. Gut18:877, 1977
Murphy, J.P., King, D.R., Dubois, A.: Treatment of gastric hypersecretion with cimetidine in the short bowel syndrome. N. Engl. J. Med.300:80, 1979
Pellerin, D., Bertin, P., Nihoul-Fekete, C., et al.: Cholelithiasis and ileal pathology in children. J. Pediatr. Surg.10:35, 1975
Roslyn, J.J., Pitt, H.A., Mann, L.L., Ament, M.E., Den Besten, L.: Gallbladder disease in patients on long-term parenteral nutrition. Gastroenterology84:148, 1983
Cohen, Z., Nordgre, S.R., MacKenzie, R.D., et al.: Pharmacokinetics of cyclosporine in a canine intestinal transplantation model. Transplant. Proc.15:3013, 1983
Ricour, C., Revillon, Y., Arnaud-Battandier, F., et al.: Successful small bowel allografts in piglets using cyclosporine. Transplant. Proc.15:3019, 1983
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ricour, C., Duhamel, J.F., Arnaud-Battandier, F. et al. Enteral and parenteral nutrition in the short bowel syndrome in children. World J. Surg. 9, 310–315 (1985). https://doi.org/10.1007/BF01656325
Issue Date:
DOI: https://doi.org/10.1007/BF01656325