Abstract
Recently, the 5-year results of a multicenter trial on proximal gastric vagotomy (PGV) have been reported. Symptomatic results in 415 duodenal ulcer patients, according to the Visick grading, were as follows: grade 1, 64%; 2, 28%; 3, 4%; and 4, 4%. It appears that one-third of the patients are symptomatic, and the question arises as to which standard such a Visick grade pattern should be compared.
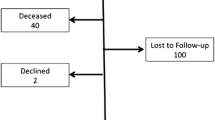
Five hundred sixty-one healthy controls (blood donors), without history of peptic ulcer or previous gastric operation, have been examined according to a standard questionnaire identical to that used for follow-up interrogation in the PGV trial. The control group was matched for sex and age with the trial population. Answers to 3 screening questions were compared with the result of detailed interrogation. The control group's Visick pattern was as follows: grade 1, 64.5%; 2, 28.9%; 3, 6.4%; and 4, 0.2%. Symptoms most frequently encountered were those of dyspepsia (pain, epigastric fullness) and gastroesophageal reflux. Dumping (2%) and diarrhea (4%) were also noted. Our conclusions are these: (1) The Visick grade pattern 5 years after PGV is almost identical with that of healthy controls. (2) Dull pain, epigastric fullness, and reflux symptoms are not specific signs after PGV. (3) Screening questions are misleading and follow-up examinations must be based on a standard questionnaire to provide valid information. (4) The separation between Visick grade 1 and 2 should be abandoned, as it has no clinical importance. (5) PGV has virtually no specific long-term sequelae except recurrence.
Résumé
Récemment les résultats à cinq ans d'une étude multicentrique consacrée à la vagotomie suprasélective ont été rapportés. Ces résultats en fonction de l'échelle d'appréciation de Visick chez 415 malades opérés pour un ulcère duodénal furent les suivants: degré I, 1,64%; degré II, 2,28%; degré III, 4%; degré IV, 4%. Il résulte de ces faits qu'au total 1/3 des opérés accusaient des troubles postopératoires, cette constatation soulevant la question de la crédibilité de cette classification. Pour l'apprécier, la même appréciation fut entreprise chez 561 sujets en bonne santé (donneurs de sang) ne présentant aucune histoire ulcéreuse ou n'ayant pas subi d'intervention gastrique, le sexe et l'âge étant pris en considération. Les réponses à 3 questions tests furent comparées à celle de l'interrogation détaillée. Les résultats de l'enquête chez ces sujets en fonction de l'échelle de Visick furent les suivants: degré 1, 64,5%; degré 2, 28,9%; degré 3, 4%; degré 6.4, 0,2%, ces sujets sains accusant le plus souvent des troubles dyspeptiques (douleurs et sensation de plénitude gastrique) ou un reflux oesophagien. 4% d'entre eux souffraient de diarrhées et 1% de dumping.1 Les auteurs tirent les conclusions suivantes de cette étude comparative:
-
1)
5 ans après vagotomie suprasélective, les troubles accusés par les opérés sont semblables à ceux présentés par les sujets en bonne santé.
-
2)
La douleur sourde, la sensation de plénitude gastrique, les signes de reflux n'appartiennent pas en propre à la vagotomie suprasélective.
-
3)
Les 3 questions tests sont trompeuses et l'appréciation postopératoire doit être fondée sur un questionnaire standard très précis pour être valable.
-
4)
La distinction entre le degré 1 et le degré 2 de l'échelle de Visick doit être abandonnée car elle ne possède aucune valeur clinique.
-
5)
La vagotomie suprasélective n'entraîne pas de séquelles spécifiques, exception faite de la récidive ulcéreuse.
Resumen
Los resultados de un ensayo de 5 años de duración, realizado en múltiples centros, sobre vagotomía gástrica proximal (VGP) han sido recientemente informados. Los resultados sintomáticos en 415 pacientes con úlcera duodenal, de acuerdo a la gradación de Visick, fueron: grado 1, 64%; 2, 28%; 3, 4% y 4, 4%. Un tercio de los pacientes aparecieron sintomáticos, y surge el interrogantes relativo al patrón de gradación, tal como el patrón de Visick, mediante el cual deben ser comparados.
Quinientos sesenta y un individuos saludables (donantes de sangre) y sin historia de úlcera péptica u operación gástrica anterior, sirvieron como control; fueron examinados de acuerdo a un cuestionario estandar idéntico al que se utilizó para el interrogatorio de seguimiento en el ensayo anterior a la VGP. El grupo control fue igualado en cuanto a sexo y edad con la población del ensayo. Las respuestas a 3 interrogantes generales de tanteo fueron comparados con el resultado de la interrogación detallada.
El patrón de Visick para el grupo control fue: grado 1, 64.5%; 2, 28.9%; 3, 6.4% y 4, 0.2%. Los síntomas encontrados con mayor frecuencia fueron aquellos de dispepsia (dolor, llenura apigástrica) y reflujo gastroesofágico. También se encontró dumping (1%) y diarrea (4%). Estas son nuestras conclusiones:
-
1.
El patrón de gradación de Visick hallado 5 años después de VGP es casi idéntico con el de controles saludables.
-
2.
Dolor sordo, llenura epigástrica y síntomas de reflujo no son signos específicos después de la VGP.
-
3.
Las preguntas generales de tanteo son enganosas y los exámenes de seguimiento deben estar basados más bien en un cuestionario definido.
-
4.
La separación entre el Visick grado 1 y el 2 debe ser abandonada, puesto que no conlleva importancia clínica.
-
5.
La VGP virtualmente está libre de secuelas a largo plazo, excepto la recurrencia.
Similar content being viewed by others
References
Visick, A.H.: A study of the failures after gastrectomy. Ann. R. Coll. Surg. Engl.3:266, 1948
Andersen, D., Høstrup, H., Amdrup, E.: The Aarhus Vagotomy Trial. II. An interim report on reduction in acid secretion and ulcer recurrence rate following parietal cell vagotomy and selective gastric vagotomy. World J. Surg.2:91, 1978
De Miguel, J.: Late results of proximal gastric vagotomy without drainage for duodenal ulcer: 5–9 year follow-up. Br. J. Surg.69:7, 1982
Goligher, J.C., Hill, G.L., Kenny, T.E., Nutter, E.: Proximal gastric vagotomy without drainage for duodenal ulcer: Results after 5–8 years. Br. J. Surg.65:145, 1978
Liåvag, I., Roland, M.: A seven-year follow-up of proximal gastric vagotomy. Scand. J. Gastroenterol.14:49, 1979
Mühe, E., Muller, C., Martinoli, S., Schacht, U., Fiedler, L., Engelke, B., Zumtobel, V., Marrie, A.: 5-year results of a prospective multicenter trial on proximal gastric vagotomy. In Vagotomy in Modern Surgical Practice, J.H. Baron, J. Alexander-Williams, M. Allgöwer, C. Muller, and J. Spencer, editors. London, Butterworths, 1982, p. 176–186
Imperati, L., Natale, C., Marinaccio, F.: Acid-fundic selective vagotomy of the stomach without drainage in the treatment of duodenal ulcer: Technique and results. Br. J. Surg.59:602, 1972
Sekine, T., Sato, T., Maki, T., Shiratori, T.: Pylorus preserving gastrectomy for gastric ulcer—One—to nine-year follow-up study. Surgery77:92, 1977
Muller, C., Allgöwer, M.: Elektive chirurgische Eingriffe in der Ulcus duodeni-Therapie. Chirurg53:9, 1982
Gisin, H.: Visick-Grading von Magengesunden. Thesis, University of Basel, 1982
Humphrey, C.S., Johnston, D., Walker, B.E., Pulvertaft, C.N., Goligher, J.C.: Incidence of dumping after truncal and selective vagotomy with pyloroplasty and highly selective vagotomy without drainage procedure. Br. Med. J.3:785, 1972
Johnston, D., Humphrey, C.S., Walker, B.E., Pulvertaft, C.N., Goligher, J.C.: Vagotomy without diarrhoea. Br. Med. J.3:788, 1972
Kennedy, T., Johnston, G.W., Macrea, K.D., Spencer, E.F.A.: Proximal gastric vagotomy: Interim results of a randomized controlled trial. Br. Med. J.2:301, 1975
Rohde, H., Troidl, H., Lorenz, W.: Systematic follow-up: A concept for evaluation of operative results in duodenal ulcer surgery. Klin. Wochenschr.55:925, 1977
Muller, C., Siewert, J.R.: Alternatives to vagotomy. In Vagotomy in Modern Surgical Practice, J.H. Baron, J. Alexander-Williams, M. Allgöwer, C. Muller, and J. Spencer, editors. London, Butterworths, 1982, p. 333–358
Johnston, D.: A therapeutic index (scoring system) for the evaluation of operations for peptic ulcer. Gastroenterology70:433, 1976
Muller, C.: Recurrent peptic ulcer after proximal gastric vagotomy. In Vagotomy in Modern Surgical Practice, J.H. Baron, J. Alexander-Williams, M. Allgöwer, C. Muller, and J. Spencer, editors. London, Butterworths, 1982, p. 312–318
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Muller, C., Engelke, B., Fiedler, L. et al. How do clinical results after proximal gastric vagotomy compare with the Visick grade pattern of healthy controls?. World J. Surg. 7, 610–615 (1983). https://doi.org/10.1007/BF01655337
Issue Date:
DOI: https://doi.org/10.1007/BF01655337