Abstract
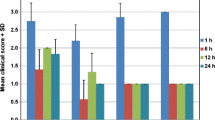
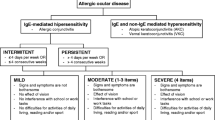
The purpose of this study was to assess the activity of some marketed products in ocular non-immune and immune type I hypersensitivity reactions, and during intra-ocular type III hypersensitivity. In order to compare these activities, we improved and validated three different models of ocular allergic reaction already known for their ability to reproduce allergic conjunctivitis or uveitis. Allergic conjunctivitis was induced by ocular immediate hypersensitivity after instillation of compound 48/80 in the rat, or an active anaphylaxis reaction with ovalbumin immunisation and challenge in the guinea pig. Uveitis was induced by a reverse passive anaphylaxis reaction using intra-vitreal rabbit anti-bovine IgG anti-serum sensitisation and intravenous bovine gammaglobulin challenge in the rabbit. Clinical scores and blood-tissue permeability indices were studied. Using the same schedule of ocular instillation, the effects of Livostin® (levocabastine 0.05%), Almide® (lodoxamide 0.1%), Opticrom® (sodium cromoglycate 2%), Ocufen® (flurbiprofen 0.03%), Acular® (ketorolac 0.5%) and 0.3% chlorpheniramine maleate were compared to positive and negative controls. We demonstrated the potent activity of chlorpheniramine maleate 0.3% and Livostin® in both allergic conjunctivitis models. Significant activity was also evidenced with Almide®, which was only active in the non-immune allergy model, while Opticrom® was definitely not active in these models. In the uveitis model, Acular® and Ocufen® are active and potent drugs, while Livostin® and Almide® were not active. These results are discussed with respect to the models used and the mediators involved.
Similar content being viewed by others
References
Levene RZ. Mast cells and amines in normal ocular tissues. Invest Ophthalmol 1962;1:531–43.
Allansmith MR, Greiner JV, Baird RS. Number of inflammatory cells in the normal conjunctiva. Am J Ophthalmol 1978;86:250–9.
Donshik PC. Allergic conjunctivitis. Int Ophthalmol Clin 1988;28:294–302.
Manjo G, Palado GE. Studies on inflammation. I. The effect of histamine and serotonin on vascular permeability: an electron microscopic study. J Biophys Biochem Cytol 1961;11:571–605.
Leng W, Chang K, Williamson JR, Jakschik BA. Increased regional vascular permeability in the rat during anaphylaxis. J Immunol 1989;142:1982–5.
Allansmith MR, Ross RN. Ocular allergy. Clin Allergy 1988;18:1–13.
Müller-Ruchholtz W. Fundamentals of immunology and their application to uveitis. Uveitis. Pathophysiology and Therapy, (Ed. Kraus-Mackiw E, O'Connor GR), Stuttgart: Thieme Med Publ 1986; pp. 1–28.
Paton WDM. Compound 48/80: a potent histamine liberator. Br J Pharmacol 1951;6:499–508.
Johnson AR, Moran NC. Release of histamine from rat mast cells. A comparison of the effects of 48/80 and two antigen-antibody systems. Fed Proc 1969;28:1716.
Okada M, Shimada K. Effects of various pharmacologic agents on allergic inflammation of the eye. Invest. Ophthalmol Vis Sci 1980;19:176–81.
Udell IJ, Abelson MB. Animal and human ocular surface response to a topical nonimmune mast-cell degranulating agent (compound 48/80). Am J Ophthalmol 1981;91:226–30.
Baird RS, Bloch KJ, Allansmith MR. Edema test for assessing ocular anaphylaxis. Curr Eye Res 1983;2:657–61.
Trocmé SD, Trocmé MC, Bloch KJ, Allansmith MR. Topically induced ocular anaphylaxis in rats immunized with egg albumin. Ophthalmic Res 1986;18:68–74.
Harada M, Takeushi M, Fukao T, Katagiri K. A simple method for the quantitative extraction of dye extravasated into the skin. J Pharm Pharmacol 1971;23:218–9.
Levine JD, Dardick SJ, Basbaum AL, Scipio E. Reflex neurogenic inflammation. I. Contribution of the peripheral nervous system to spatially remote inflammation responses that follow injury. J Neurosci 1985;5:1380–6.
Doherty MJ, Easty DL. Inflammatory and immunological cell profiles in a rat model of conjunctival immediate hypersensitivity. Clin Exp Allergy 1989;19:449–55.
McIntosh FC, Paton WDM. The liberation of histamine by certain organic bases. J Physiol (Lond) 1949;109:190–8.
Tomioka H, Ishizaka K. Mechanisms of passive sensitization. II. Presence of receptors for IgE on monkey mast cells. J. Immunol. 1971;107:971–8.
Bloch KJ, Ohman JL, Waltin J, Cygan RW. Potentiated reagin response: initiation with minute doses of antigen and alum followed by infection with Nippostrongylus brasiliensis. J Immunol 1973;110:197–204.
Dwyer RSC, Turk JL, Darougar S. Immediate hypersensitivity in the guinea pig conjunctiva. I. Characterisation of the IgE andIgG 1 antibodies involved. Int Arch Allergy 1974;46:910–24.
Allansmith MR, Bloch KJ, Baird RS, Sinclair K. Ocular anaphylaxis: induction by local injection of antigen. Immunology 1981;44:623–7.
Carreras I, Carreras B, McGrath L, Rice A, Easty DLE. Activated T cells in an animal model of allergic conjunctivitis. Br J Ophthalmology 1993;77:509–14.
Allansmith MR, Baird RS, Greiner JV, Bloch KJ. Late-phase reactions in ocular anaphylaxis in the rat. J Allergy Clin Immunol 1984;73:49–55.
Abelson MB, Udell IJ, Weston JH. Conjunctival eosinophils in compound 48/80 rabbit model. Arch Ophthalmol 1983;101:631–3.
Tannenbaum S, Oertel H, Henderson W, Kaliner M. The biologic activity of mast cell granules: I. Elicitation of inflammatory responses in rat skin. J Immunol 1980;125:325–35.
Calonge MC, Pastor JC, Herreras JM, Gonzalez JL. Pharmacologic modulation of vascular permeability in ocular allergy in the rat. Invest. Ophthalmol Vis Sci 1990;31:176–80.
Allansmith MR, Baird RS, Henriquez AS, Bloch KJ. Sequence of mast cell changes in the ocular anaphylaxis. Immunology 1983;49:281–7.
Allansmith MR, Baird RS, Ross RN, Barney NP, Bloch KJ. Ocular anaphylaxis induced in the rat by topical application of compound 48/80. Dose response and time course study. Acta Ophthalmol 1989;67:145–53.
Rowley DA, Benditt EP. 5-Hydroxytryptamine and histamine as mediators of the vascular injury produced by agents which damage mast cells in rats. J Exp Med 1956;103:399–415.
Woodward DF, Ledgard SE, Nieves AL. Conjunctival immediate hypersensitivity: Re-evaluation of histamine involvement in the vasopermeability response. Invest Ophthalmol Vis Sci 1986;27:57–63.
Umemoto M, Tanaka H, Miichi H, Hayashi S. Histamine receptors on rat ocular surface. Ophthalmic Res 1987;19:200–4.
Kirkegaard J, Secher C, Mygind N. Effect of the H1 antihistamine chlorpheniramine maleate on histamine-induced symptoms in the human conjunctiva. Allergy 1982;37:203–8.
Dechant KL, Goa KL. Levocabastine. A review of its pharmacological properties and therapeutic potential as a topical antihistamine in allergic rhinitis and conjunctivitis. Drugs 1991;41:202–24.
Sorkin EM, Ward A. Ocular sodium cromoglycate: an overview in its therapeutic efficacy in allergic eye disease. Drugs 1986;31:131–48.
Easty DL. Sodium cromoglycate eye drops in allergic conjunctivitis. Acta Allerg 1977;32:62–7.
Iso T, Nakajima N, Suda H, Yamauchi H, Uda K. Passive anaphylaxis in rat conjunctiva and topical effects of antiallergic agents. Ophthalmic Res 1980;12:9–15.
Calonge M, Ng B, Allansmith MR, Bloch KJ. Vascular permeability during the early and late phase of ocular anaphylaxis. Invest Ophthalmol Vis Sci 1992;33:55–9.
Lewis RA, Austen KF. Mediation of local homeostasis and inflammation by leukotrienes and other mast cell-dependent compounds. Nature (Lond) 1981;293:103–8.
Crunkhorn P, Willis AL. Cutaneous reactions to intradermal prostaglandins. Br J Pharmacol 1971;41:49–56.
Smelser GK, Silver S. The distribution of mast cells in the normal eye. A method of study. Exp Eye Res 1963;2:134–40.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Khosravi, E., Elena, P.P. & Hariton, C. Allergic conjunctivitis and uveitis models: Reappraisal with some marketed drugs. Inflamm Res 44, 47–54 (1995). https://doi.org/10.1007/BF01630487
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01630487