Summary
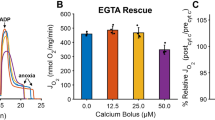
Cellular changes occuring in the left ventricular myocardium during ischaemia after different methods of cardiac arrest have been evaluated by morphological and morphometric parameters: volume densities of mitochondria (VVMi), sarcoplasm (VVSp), myofibrils (VVMf), surface densities of mitochondria (SVMi). The surface to volume ratio of mitochondria (SVratioMi) has been used as an independent parameter of mitochondrial swelling.
Since ischaemic swelling of myocardial cells increases the volume of the reference space and ischaemic swelling of mitochondria decreases the free sarcoplasm, VVMi and VVSp cannot be considered as reliable indicators of the degree of oedema. SVMi/VVMf remains nearly constant after different forms of cardiac arrest, demonstrating the integrity of mitochondrial outer membranes. The inverse linear ratio between SVratioMi and the mean mitochondrial volume indicates that the increase in mitochondrial volume is achieved by surface smoothing.
Loss of matrix structure and fragmentation of cristae occur at an SVratioMi of about 5.8, cristolysis at 5.5 to 5.6 and amorphous matrix densities at an SVratioMi of less than 5.5 μm2/μm3.
The SVratioMi is a suitable parameter for evaluating mitochondrial swelling both at the onset and during global myocardial ischaemia, independent of the method of cardiac arrest used. It serves as an indicator of the state of structural preservation of mitochondria during ischaemia.
Similar content being viewed by others
References
Anversa P, Loud AV, Giacomelli F, Wiener J (1978) Absolute morphometric study of myocardial hypertrophy in experimental hypertension. Lab Invest 38:597–609
Bretschneider HJ (1964) Überlebenszeit und Wiederbelebungszeit des Herzens bei Normo- und Hypothermie. Verh Dtsch Ges Kreisl-Forsch 30:11–34
Canale ED, Campbell GR, Smolich JJ, Campbell JH (1986) Cardiac Muscle. In: Oksche A, Vollrath L (eds) Handbook of microscopic anatomy, Vol II/7. Springer, Berlin Heidelberg New York
David H (1979) Some recent results of the quantitative characterization of heart muscle cells. Z Mikr-Anat Forsch Leipzig 93:113–137
Ferrans VJ, Robert WC (1971/72) Myocardial ultrastructure in acute and chronic hypoxia. Cardiology 56:144–160
Gebhard MM, Preusse CJ, Schnabel PhA, Bretschneider HJ (1984) Different effects of cardioplegic solution HTK during single or intermittent administration. Thorac Cardiovasc Surgeon 32:271–276
Gebhard MM, Bretschneider HJ, Schnabel PhA (1989) Cardioplegia: Principles and problems. In: Sperelakis N (ed) Physiology and pathophysiology of the heart, 2nd ed. Kluwer Dordrecht, pp 655–669
Goldstein MA, Murphy DL (1983) A morphometric analysis of ischemic canine myocardium with and without reperfusion. J Mol Cell Cardiol 15:325–334
Greve G, Rotevatn S, Grong K, Stangeland L (1988) Cellular morphometric changes in cat hearts subjected to three hours of regional ischemia. Virchows Arch [A] Pathol Anat 412:205–213
Gundersen HJG, Osterby R (1981) Optimizing sampling efficiency of stereological studies in biology: or “Do less more well!” J Microsc 121:65–73
Hayat MA (1981) Fixation for electron microscopy. Academic Press, New York London Toronto Sydney San Francisco
Jennings RB, Hawkins HK (1980) Ultrastructural changes of acute myocardial ischemia. In: Wildenthal K (ed) Degradative processes in heart and skeletal muscle. Elsevier/North-Holland, Biomedical Press, Amsterdam New York Oxford, pp 295–346
Jennings RB, Reimer KA, Jones RN, Peyton RB (1983) High energy phosphates, aenerobic glycolysis and irreversibility in ischemia. In: Spitzer JJ (ed) Myocardial injury. Plenum Press, New York London, pp 403–419
Karnovsky MJ (1965) A formaldehyde-glutaraldehyde fixative of high osmolality for use in electron microscopy. J Cell Biol 27:137–138
Mall G, Mattfeldt T, Möbius H-J, Leonhard R (1986) Stereological study on the rat heart in chronic alimentary thiamine deficiency — absence of myocardial changes despite starvation. J Mol Cell Cardiol 18:635–643
Marino ThA, Houser StR, Martin FG, Freeman AR (1983) An ultrastructural morphometric study of the papillary muscle of the right ventricle of the cat. Cell Tissue Res 230:543–552
McCallister LP, Daiello DC, Tyers GFO (1978) Morphometric observation of the effect of normothermic ischemic arrest on dog myocardial ultrastructure. J Mol Cell Cardiol 10:67–80
Paulussen F, Hübner G, Grebe D, Bretschneider HJ (1968) Die Feinstruktur des Herzmuskels während einer Ischämie mit Senkung des Energiebedarfs durch spezielle Kardioplegie. Klin Wochenschr 46:165–171
Preusse CJ, Gebhard MM, Bretschneider HJ (1981) Myocardial “equilibration processes” and myocardial energy turnover during initiation of artificial cardiac arrest with cardioplegic solution — reasons for a sufficiently long cardioplegic perfusion. Thorac Cardiovasc Surgeon 29:71–76
Riede VN, Wassilew G, Tschirkov A (1982) Pharmakologische Kardioplegie und Myokardprotektion während der Ischämiephase durch Nifedipin. Eine ultrastrukturell-morphometrische Studie. In: Just H, Tschirkov A, Schlosser V (eds) Kalziumsantagonisten zur Kardioplegie und Myokardprotektion in der offenen Herzchirurgie. Thieme, Stuttgart New York, pp 154–164
Schaper J, Mulch B, Winkler B, Schaper W (1979) Ultrastructural, functional and biochemical criteria for estimation of reversibility of ischemic injury: a study on the effects of global ischemia on the isolated dog heart. J Mol Cell Cardiol 11:521–541
Schaper J, Meister E, Stämmler G (1985) Ultrastructural morphometric analysis of myocardium from dogs, rats, hamsters, mice, and from human hearts. Circ Res 56:377–391
Schaper J, Scheld HH, Schmidt U, Hehrlein F (1986) Ultrastructural study comparing the efficacy of five different methods of intraoperative myocardial protection in the human heart. J Thorac Cardiovasc Surg 92:47–55
Schmiedl A (1988) Zur Beeinflußbarkeit der Feinstruktur der Mitochondrien von Herzmuskelzellen während und nach Ischämiebelastung. Dissertation an der Mathematischnaturwissenschaftlichen Fakultät der Universität Göttingen
Schmiedl A, Schnabel PhA, Eins S, Gebhard MM, Pomykaj Th, Richter J, Bretschneider HJ (1987) Vergleich zwischen Immersions- und Perfusionsfixierung nach Kardioplegie — Morphometrische Befunde. Verh Anat Ges 81:143–144
Schmiedl A, Gebhard MM, Mall G, Schnabel PhA, Richter J, Bretschneider HJ (1988) Korrelationen der Mitochondrienschwellung zu metabolischen Parametern im global ischämischen Hundemyokard. Z Kardiol 77 (Suppl 1):24, 62
Schnabel PhA, Gebhard MM, Preusse CJ, Richter J, Schwartz P, Spieckermann B, Bretschneider HJ (1983) Protektion der Ultrastruktur im ischämischen Myokard durch die kardioplegische Lösung HTK nach Bretschneider bei 25° C. Verh Anat Ges 77:605–608
Schnabel PhA, Gebhard MM, Pomykaj Th, Schmiedl A, Preusse CJ, Richter J, Bretschneider HJ (1987a) Myocardial protection: left ventricular ultrastructure after different forms of cardiac arrest. Thorac Cardiovasc Surgeon 35:148–156
Schnabel PhA, Pomykaj Th, Schmiedl A, Gebhard MM, Richter J, Bretschneider HJ (1987b) Structural inhomogeneities of myocardial biopsies after cardioplegia. Thorac Cardiovasc Surgeon 35 (special issue 1): 45–46
Schnabel PhA, Gebhard MM, Pomykaj Th, Richter J, Schmiedl A, Bretschneider HJ (1987c) Optimierung von Perfusionsfixierungen des Herzens durch Kardioplegie. Verh Anat Ges 81:141–142
Steen RG, Newman WH, Lindemayer GE (1983) Modification of ischemia-induced myocardial damage. In: Trump BF, Arstila AV (eds) Pathobiology of cell membranes. Academic Press, New York, pp 63–85
Tranum-Jensen J, Janse MJ, Fidet JWT, Krieger WJG, D'Alnoncourt CN, Durrer D (1981) Tissue osmolality, cell swelling, and reperfusion in acute regional myocardial ischemia in the isolated porcine heart. Circ Res 49:364–381
Trump BF, Berezesky JK, Collan Y, Kahng MW, Mergner WJ (1976) Recent studies on the pathophysiology of ischemic cell injury. Beitr Path 158:363–388
Wassilew G, David H (1977) Vergleichende morphometrische Untersuchungen an normalen Herz- und Zwerchfellmitochondrien des Hundes. Verh Anat Ges 71:239–241
Weibel ER (1979) Stereological methods, Vol 1. Practical methods for biological morphometry. Academic Press, New York
Author information
Authors and Affiliations
Additional information
Supported by the Deutsche Forschungsgemeinschaft, SFB 330-Organprotektion — Göttingen
Rights and permissions
About this article
Cite this article
Schmiedl, A., Schnabel, P.A., Mall, G. et al. The surface to volume ratio of mitochondria, a suitable parameter for evaluating mitochondrial swelling. Vichows Archiv A Pathol Anat 416, 305–315 (1990). https://doi.org/10.1007/BF01605291
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01605291