Summary
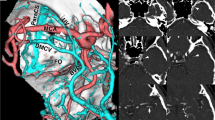
The anatomical variations of Sylvian vein and cistern were investigated during the pterional approach in 230 patients with 276 aneurysms of anterior circulation arteries, that were operated on at the Neurosurgical Department of Atatürk University Medical School, Erzurum, Turkiye. All patients underwent radical surgery for aneurysm by the right or left pterional approach. The findings were recorded during surgical intervention and observed through the slides and videotapes of the operations.
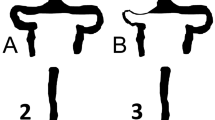
In our study, we surgically classified the variations of the Sylvian vein, according to its branching and draining patterns. Type I: The fronto-orbital (frontosylvian), fronto-parietal (parietosylvian) and anterior temporal (temporosylvian) veins drain into one sylvian vein. Type II: Two superficial Sylvian veins with separated basal vein draining into the sphenoparietal and Rosenthal's basal vein. Type III: Two superficial Sylvian veins draining into the sphenoparietal and the superior petrosal veins. Type IV: Hypoplastic superficial Sylvian vein and the deep one. Four types of Sylvian vein variations were defined as follows. The Type I was seen in 45% (n = 103), the Type II was found in 29% (n = 67), Type III was recorded in 15% (n = 34) and Type IV, or hypoplastic and deep form was discovered in 11% (n = 26) of patients. The course of the Sylvian vein was on the temporal side (Temporal Coursing) in 70 percent of the cases (n= 160), on the frontal side (Frontal Coursing) in 19% of the patients (n = 45) and in 8 percent of the cases (n= 18) in the deep localization (Deep Coursing). Only 3 percent of the cases (n = 7) showed a mixed course. The variations of the Sylvian cisterns were classified into three types, according to the relationships between the lateral fronto-orbital gyrus and the superior temporal gyrus. In Sylvian Type, the frontal and temporal lobes are loosely (Sylvian Type A, Large) or tightly (Sylvian Type B, Close and Narrow) approximated on the surface thereby covering the area of the Sylvian cistern. In frontal type, the proximal part of the lateral fronto-orbital gyrus herniated into the temporal lobe. In temporal type, the proximal part of the superior temporal gyrus herniated into the lateral fronto-orbital gyrus. The variations of the Sylvian cisterns in 230 patients were as follows: in 31% (n = 71) Sylvian Type A, in 21% (n = 48) Sylvian Type B, in 34% (n = 78) Frontal Type, and in 14% (n = 33) Temporal Type.
We concluded that venous perfusion disorder of the brain is the most important factor during the pterional approach. Careful intraoperative assessment and protection of the Sylvian vein, which is a surgical pitfall, is an indispensable part of the operation. The recognition of the anatomical variations of the Sylvian vein and cistern, and the detailed knowledge of the microvascular relationships at that level will allow the neurosurgeon to construct a better and safter microdissection plan, to save time and can prevent postoperative neurological deficits.
Similar content being viewed by others
References
Andrews RJ, Bringas JR (1993) A review of brain retraction and recommendations for minimizing intraoperative brain injury. Neurosurgery 33: 1052–1064
Aydin IH, Kadioğlu HH, Takçi E, Kayaoğlu ÇR, Tüzün Y (1995) The anatomical variations of Sylvian fissure and vein in 700 operative cases. Congress of Neurological Surgeons 45th Annual Meeting, October 14–19, San Francisco, CA, USA, Abstract Book, p 216
Aydin IH, Önder A, Kadioğlu HH (1993) Giant intracranial aneurysms in children and adolescents. Zentralbl Neurochir 54: 35–38
Aydin IH, Önder A, Kadioğlu HH, Tahmazoğlu I, Kayağlu ÇR (1992) Postoperative anosmia after removal of pituitary gland adenomas using the pterional approach. Acta Neurochir (Wien) 119: 101–103
Aydin IH, Önder A, Takçi E, Kadioğlu HH, Kayaoğlu ÇR, Tüzün Y (1994) Heubner's artery variations in anterior communicating artery aneurysms. Acta Neurochir (Wien) 127: 17–20
Aydin IH, Takçi E, Kadioğlu HH, Kayaoğlu ÇR, Tüzün Y (1995) Pitfalls in the pterional approach to the parasellar area (review). Minim Invas Neurosurg 38: 146–153
Aydin IH, Takçi E, Kadioğlu HH, Kayaoğlu ÇR, Tüzün Y (1996) The variations of lenticulostriate arteries in the middle cerebral artery aneurysms. Acta Neurochir (Wien) 138: 555–559
Bisaria KK (1985) The superficial Sylvian vein in humans: with special reference to its termination. Anat Rec 212: 319–363
Browder J, Krieger AJ, Kaplan HA (1974) Cerebral veins in the surgical exposure of the middle cerebral artery. Surg Neurol 2: 319–325
Cambria S (1980) Thrombosis of the vein of Labbé with hemorrhagic cerebral infarction. Rev Neurol (Paris) 136: 321–326
Harkey HL, Al-Mefty O, Haines DE, Smith RR (1989) The surgical anatomy of the cerebral sulci. Neurosurgery 24: 651–654
Inagawa T (1991) Superficial Sylvian veins as landmarks for operation of middle cerebral artery aneurysms. Hiroshima J Med Sci 40: 71–73
Kageyama Y, Fukuda K, Kobayashi S, Odaki M, Nakamura H, Satoh A, Watanabe Y (1992) Cerebral vein disorders and postoperative brain damage associated with the pterional approach in aneurysm surgery. Neurol Med Chir (Tokyo) 32: 733–738
Krayenbuhl HA, Yaşargil MG (1968) Cerebral angiography. Lippincott, Philadelphia, pp 85–108
Meder JF, Chiras J, Roland J, Guinet P, Bracards S, Bargy F (1994) Venous territory of the brain. J Neuroradiol 21: 118–133
Oka K, Rhoton AL Jr, Barry M, Rodriguez R (1985) Microsurgical anatomy of the superficial veins of the cerebrum. Neurosurgery 17: 711–748
Okudera T, Ohta T, Huang YP, Yokota A (1988) Developmental and radiological anatomy of the superficial cerebral convexity vessels in the human fetus. J Neuroradiol (France) 15: 205–224
Ono M, Kubik S, Abernathey CD (1990) Atlas of the cerebral sulci. Thieme, Stuttgart
Ono M, Rhoton AL Jr, Peace D, Rodriguez R (1984) Microsurgical anatomy of the deep venous system of the brain. Neurosurgery 15: 621–657
Rhoton AL Jr, Yamamoto I, Peace DA (1981) Microsurgery of the third ventricle. Part 2. Operative approaches. Neurosurgery 8: 57–373
Yamamoto I, Rhoton AL Jr, Peace DA (1981) Microsurgery of the third ventricle. Part 1. Microsurgical anatomy. Neurosurgery 8: 334–356
Vorkapic P, Perneczky A, Tschabitscher M, Knops E, Flohr A (1985) Transsylvian approach to the tentorial hiatus. Anatomical remarks on the microsurgical exposure. Zentralbl Neurochir 46: 2–10
Wilkins RH, Odom GL (1982) General operative technique. In: Youmans JR (ed) Neurological surgery. Saunders, Philadelphia, p 1146
Witelson SF, Kigar DL (1992) Sylvian fissure morphology and asymmetry in men and women: bilateral differences in relation to handness in men. J Comp Neurol 323: 326–340
Yaşargil MG, Gravens GF, Roth P (1988) Surgical approaches of “inaccessible” brain tumors. Clin Neurosurg 34: 42–110
Yaşargil MG (1969) Microsurgery applied to neurosurgery. Thieme, Stuttgart, pp 119–143
Yaşargil MG, Antic J, Laciga R (1976) Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg Neurol 6: 83–91
Yaşargil MG (1994) Anatomy. Topographic anatomy for microsurgical approaches to intrinsic brain tumors, Vol 4A. In: Microneurosurgery. Thieme, New York, pp 2–114
Yaşargil MG (1984) Operative anatomy. In: Microneurosurgery, Vol 1. Thieme-Stratton, New York, pp 5–168
Yaşargil MG (1984) Interfascial pterional (frontotemporoshpenoidal) craniotomy. In: Microneurosurgery, Vol 1. Thieme-Stratton, New York, pp 215–233
Yaşargil MG, Fox JL, Ray MW (1975) The operative approach to aneurysms of the anterior communicating artery. In: Krayenbuhl Het al (eds) Advances and technical standards in neurosurgery, Vol 2. Springer, Wien New York, pp 113–170
Yaşargil MG, Smith RD, Firth JL (1989) The principles of microsurgery as applied to aneurysm surgery. In: Symon L, Thomas DG, Clark K (eds) Rob & Smith's operative surgery. London, Butterworths, pp 146–153
Yokoh A, Sugita K, Koboyashi S (1983) Intermittent versus continuous brain retraction. J Neurosurg 58: 918–923
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Aydin, I.H., Kadioğlu, H.H., Tüzün, Y. et al. The variations of sylvian veins and cisterns in anterior circulation aneurysms. Acta neurochir 138, 1380–1385 (1996). https://doi.org/10.1007/BF01411115
Issue Date:
DOI: https://doi.org/10.1007/BF01411115