Abstract
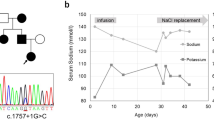
This paper describes a patient with severe pseudohypoaldosteronism (PHA) for over 12 years. The patient presented at 10 days of age with a serum sodium of 118 mEq/l and potassium of 12 mEq/l. After failing to maintain normal fluid and electrolyte status with standard therapy, including maximal mineralocorticoid stimulation, he was given a special formula containing minimal potassium plus salt supplements which normalized his electrolyte status. However, when he was 4.5 years of age, an acute gastrointestinal illness led to severe volume depletion, hyperkalemia, and cardiopulmonary arrest. This resulted in significant neurological impairment. At 12.5 years of age, the patient continues to require massive sodium supplements and his diet contains less than 0.5 mEq/kg potassium daily; his height and weight are at the 95th percentile, thus demonstrating that normal growth may be achieved with strict dietary manipulation in a patient with persistent, severe PHA. Serial studies to further define the lesion in this patient have demonstrated: (1) normal binding of aldosterone to aldosterone binding globulin (5.1% bound); (2) normal mineralocorticoid “activity”; (2) suppressible renin and aldosterone levels; (4) increased prostaglandin excretion (3.15 μg/g creatinine); (5) lack of benefit of prostaglandin inhibition with indomethacin; (6) normal proximal tubule function (\(C_{Na} + C_{H_2 O} = 18.0 ml/100\) ml glomerular filtration rate; (7) impaired distal tubule function\(\left( {C_{H_2 O} /C_{Na} + C_{H_2 O} = 79.8\% } \right)\) during water diuresis.
Similar content being viewed by others
References
Cheek DB, Perry JW (1958) A salt wasting syndrome in infancy. Arch Dis Child 33: 252–256
Donnell GN, Litman N, Roldan M (1959) Pseudohypo-adrenalocorticism. Renal sodium loss, hyponatremia, and hyperkalemia due to a renal tubular insensitivity to mineralocorticoids. J Dis Child 97: 813–828
Raine DN, Roy J (1962) A salt-losing syndrome in infancy. Pseudohypoadrenocorticalism. Arch Dis Child 37: 548–556
Royer P, Bonnette J, Mathieu H, Gabilan JC, Klutchko C, Zittoun R (1963) Pseudohypoaldosteronisme. Ann Pediatr 10: 595–605
Barakat AY, Papadopoulou ZL, August GP (1972) A hyperkalemic salt-wasting syndrome in infancy. Pediatr Res 6: 394A
Proesmans W, Guessens H, Corbeel L, Eeckels R (1974) Pseudohypoaldosteronism. Am J Dis Child 126: 510–516
Dillon MJ, Leonard JV, Buckler JM, Ogilvie D, Lillystone D, Honour JW, Shackleton CHL (1980) Pseudohypoaldosteronism. Arch Dis Child 55: 427–434
Savitt H, Molitch M, Kawaoka E, Leake R (1975) Pseudohypoaldosteronism. Clin Res 23: 165A
Shackleton CHL, Snodgrass GHAI (1974) Steroid excretion by an infant with an unusual salt-losing syndrome: a gas chromatographic-mass spectrometric study. Ann Clin Biochem 11: 91–99
Postel-Vinay MD, Alberti GM, Ricour C, Limal JM, Rappaport R, Royer P (1974) Pseudohypoaldosteronism: persistence of hyperaldosteronism and evidence for renal tubular and intestinal responsiveness to endogenous aldosterone. J Clin Endocrinol Metab 39: 1038–1044
McCredie Da, Cheek DB, Rotenberg E, Stokigt JR (1977) Pseudohypo-aldosteronism — a long-term follow-up. Abstracts of the 4th International Symposium of Pediatric Nephrology 86A
Satayaviboon S, Dawgert F, Monteleone PL, Monteleone JA (1982) Persistent pseudohypoaldosteronism in a 7-year-old boy. Pediatrics 69: 458–462
Armanini D, Kuhnle U, Strasser T, Dorr H, Butenandt I, Weber PC, Stockigt JR, Pearce P, Funder JW (1985) Aldosterone-receptor deficiency in pseudohypoaldosteronism. N Engl J Med 313: 1178–1181
Bierich JR, Schmidt U (1976) Tubular Na, K-ATPase deficiency, the cause of the congenital renal salt-losing syndrome. Eur J Pediatr 121: 81–87
Proesmans W, Muaka B ki, Corbeel L, Eeckels R (1978) Pseudohypo-aldosteronism, a proximal tubular sodium wasting disease. J Pediatr 92: 678–679
Roy C (1977) Pseudohypoaldosteronisme familial (A propos de 5 cas). Arch Fr Pediatr 34: 37–54
Loris C, Izaguirre C, Mazana M, Bassecourt M, Diez-Antonanzas J (1979) Pseudohypoaldosteronism: proximal or distal tubular wasting syndrome (abstract). Abstracts of the 13th Annual Meeting of the European Society for Paediatric Nephrology Capri, Italy, 7–10 June 1979
Savage MO, Jefferson IG, Dillon MJ, Milla PJ, Honour JW, Grant DB (1982) Pseudohypoaldosteronism: severe salt wasting in infancy caused by generalized mineralocorticoid unresponsiveness. J Pediatr 101: 239–242
Anand SK, Froberg L, Northway JD, Weinberger M, Wright JC (1976) Pseudohypoaldosteronism due to sweat gland dysfunction. Pediatr Res 10: 677–682
Oberfield SE, Levin LS, Cary RM, Bejar R, New MI (1979) Pseudohypo-aldosteronis multiple target organ unresponsiveness to mineralocorticoid hormones. J Clin Endocrinol Metab 48: 228–234
Rodriguez-Soriano J, Vallo A, Garcia-Fuentes M (1975) Distal renal tubular acidosis in infancy: a bicarbonate wasting state. J Pediatr 86: 527–532
Nowaczynski W, Genest OJ, Kuchel O, Messerli FH, Guthrie GP, Richardson K, Grose J (1977) Age and posture related changes in plasma protein binding and metabolism of aldosterone in essential and secondary hypertension. J Lab Clin Med 90: 475–478
Baxter JD, Schambelan M, Matulich DT, Spindler BJ, Taylor AA, Bartter FC (1976) Aldosterone receptors and the evaluation of plasma mineralocorticoid activity in normal and hypertensive states. J Clin Invest 58: 579–589
Frolich JC, Wilson TW, Sweetman BJ, Smigel M, Nies AS, Carr K, Watson JT, Oates JA (1975) Urinary prostaglandins. Identification and origin. J Clin Invest 55: 763–770
Frolich JC (1977) Gas chromatography-mass spectrometry of prostaglandins. In: Ramwell PW (ed) The prostaglandins, vol 3. Plenum, New York, pp 1–39
Rosler A, Theodor R, Boichis H, Gerty R, Ulick S, Alagem M, Tabachnik E, Cohen B, Rabinowitz D (1977) Metabolic responses to the administration of angiotensin II, K and ACTH in two salt-wasting syndromes. J Clin Endocrinol Metab 44: 292–301
Corvol P, Claire M, Oblin ME, Geering K, Rossier B (1981) Mechanism of the antimineralocorticoid effects of spirolactones. Kidney Int 20: 1–6
Rampini S, Furrer J, Kellr HP, Bucher H, Zachmann M (1978) Congenital pseudohypoaldosteronism: case report and review. Effect of indomethacin during sodium chloride depletion. Helv Paediatr Acta 33: 153–167
Mulrow PJ, Forman BH (1972) The tissue effects of mineralocorticoids. Am J Med 53: 561–572
Petersen S, Giese J, Kappelgaard AM, Lund HT, Lund JO, Nielsen MD, Tomsen AC (1978) Pseudohypoaldosteronism. Clinical, biochemical, and morphological studies in a long term follow-up. Acta Paediatr Scand 67: 255–261
Sebastian A, Sutton JM, Hulter HN, Schambelan M, Poler SM (1980) Effect of mineralocorticoid replacement therapy on renal acid-base homeostasis in adrenalectomized patients. Kidney Int 18: 762–773
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hogg, R.J., Marks, J.F., Marver, D. et al. Long term observations in a patient with pseudohypoaldosteronism. Pediatr Nephrol 5, 205–210 (1991). https://doi.org/10.1007/BF01095953
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01095953