Abstract
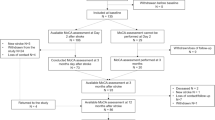
To investigate the frequency, course, and clinical correlates of disorientation following stroke, we administered the Mini-Mental State Examination orientation subtest to 177 alert patients 7–10 days and 3 months after stroke and 240 stroke-free nondemented subjects. Disorientation was defined as a score ≤ 8/10. Seventy-two (40.7%) of the patients were disoriented 7–10 days after stroke and 39 patients (22.0% of the sample) remained disoriented 3 months later. A logistic regression analysis determined that persistent disorientation was significantly related to stroke status [odds ratio (OR)=5.8], after adjusting for memory and attentional deficits and demographic variables. Among stroke patients, disorientation was associated with severe hemispheral stroke syndromes (OR=7.7), but not infarct location or vascular risk factor history, after adjusting for memory and attentional deficits and demographic variables. Sensitivity and specificity analyses determined that disorientation was an inaccurate marker for dementia or deficits in memory or attention, while intact orientation was associated with a low probability of dementia or memory dysfunction in most patients but not preserved attention. We conclude that disorientation is common and persistent following stroke and associated with severe hemispheral stroke syndromes but not infarct location. While disorientation is a poor marker for dementia or deficits in memory or attention, intact orientation should suggest that cognitive functions are likely to be preserved.
Similar content being viewed by others
References
Benton AL (1968) Differential behavioral effects in frontal lobe disease. Neuropsychologia 6:53–60
Desmond DW, Tatemichi TK, Stern Y, Sano M (1992) Cognitive dysfunction following first stroke (abstract). Neurology 42 [Suppl 3]:426
Desmond DW, Tatemichi TK, Paik M, Stern Y (1993) Risk factors for cerebrovascular disease as correlates of cognitive function in a stroke-free cohort. Arch Neurol 50:162–166
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Foulkes MA, Wolf PA, Price TR, Mohr JP, Hier DB (1988) The Stroke Data Bank: design, methods, and baseline characteristics. Stroke 19:547–554
Gottlieb G, Wilson I (1965) Cerebral dominance: temporary disruption of verbal memory by unilateral electroconvulsive shock treatment. J Comp Physiol Psychol 60:368–372
Groher M (1977) Language and memory disorders following closed head injury. J Speech Hear Res 20:212–223
Halliday AM, Davison K, Browne MW, Kreeger LC (1968) A comparison of the effects on depression and memory of bilateral E.C.T. and unilateral E.C.T. to the dominant and nondominant hemispheres. Br J Psychiatry 114:997–1012
High WM, Levin HS, Gary HE (1990) Recovery of orientation following closed-head injury. J Clin Exp Neuropsychol 12:703–714
Huber SJ, Shuttleworth EC, Freidenberg DL (1989) Neuropsychological differences between the dementias of Alzheimer's and Parkinson's diseases. Arch Neurol 46:1287–1291
Hunter R, McLuskie R, Wyper D, Patterson J, Christie JE, Brooks DN, McCulloch J, Fink G, Goodwin GM (1989) The pattern of function-related regional cerebral blood flow investigated by single photon emission tomography with99mTc-HMPAO in patients with presenile Alzheimer's disease and Korsakoff's psychosis. Psychol Med 19:847–855
Kopelman MD (1986) Clinical tests of memory. Br J Psychiatry 148:517–525
Levin HS, Grossman RG (1978) Behavioral sequelae of closed head injury: a quantitative study. Arch Neurol 35:720–727
Mahurin RK, DeBettignies BH, Pirozzolo FJ (1991) Structured Assessment of Independent Living Skills: preliminary report of a performance measure of functional abilities in dementia. J Gerontol 46:P58-P66
Mesulam MM (1990) Large-scale neurocognitive networks and distributed processing for attention, language, and memory. Ann Neurol 28:597–613
Stern Y, Andrews H, Pittman J, Sano M, Tatemichi T, Lantigua R, Mayeux R (1992) Diagnosis of dementia in a heterogeneous population: development of a neuropsychological paradigm-based diagnosis of dementia and quantified correction for the effects of education. Arch Neurol 49:453–460
Tatemichi TK, Desmond DW, Mayeux R, Paik M, Stern Y, Sano M, Remien RH, Williams JBW, Mohr JP, Hauser WA, Figueroa M (1992) Dementia after stroke: baseline frequency, risks, and clinical features in a hospitalized cohort. Neurology 42:1185–1193
Thase ME, Liss L, Smeltzer D, Maloon J (1982) Clinical evaluation of dementia in Down's syndrome: a preliminary report. J Ment Defic Res 26:239–244
Valentine M, Keddie KMG, Dunne D (1968) A comparison of techniques in electro-convulsive therapy. Br J Psychiatry 114:989–996
Wade DT, Skilbeck C, Hewer RL (1989) Selected cognitive losses after stroke: frequency, recovery, and prognostic importance. Int Disabil Stud 11:34–39
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Desmond, D.W., Tatemichi, T.K., Figueroa, M. et al. Disorientation following stroke: Frequency, course, and clinical correlates. J Neurol 241, 585–591 (1994). https://doi.org/10.1007/BF00920621
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00920621