Summary
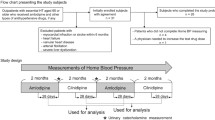
Hypertension is due to disturbance of the complex interplay between numerous known and unknown mechanisms that normally control blood pressure. Antihypertensive agents may, therefore, reduce blood pressure through widely different actions and, at the same time, elicit counterregulatory responses. This is a review of the long-term hemodynamic effects at rest as well as during exercise of nine relatively new antihypertensive compounds: a beta-blocker (epanolol), an alpha-receptor blocker (doxazosin), two double-acting compounds (dilevalol and carvedilol), three calcium antagonists (amlodipine, felodipine, and diltiazem), an angiotensin-converting enzyme inhibitor (lisinopril), a serotonin antagonist (ketanserin), and low-salt diet as a nonpharmacological treatment in 171 patients with mild to moderate essential hypertension. The results in the treatment groups are compared to the hemodynamic changes seen in 28 hypertensive patients left untreated for 10 years. The patient populations of the different groups were comparable. The invasive hemodynamic technique, including intraarterial blood pressure recording and measurements of cardiac output by Cardigreen, was the same in all studies. While blood pressure remained nearly unchanged in the untreated group, all antihypertensive compounds induced significant and sustained blood pressure reduction both at rest and during exercise. The modest reduction (3–5%) in blood pressure during a low-salt diet was also statistically significant. This review shows the multiplicity of the long-term hemodynamic changes, ranging from a reduction in cardiac output to peripheral vasodilatation, during chronic antihypertensive therapy. In untreated hypertensives, the cardiac output is reduced by 1–2% per year and total peripheral resistance is increased by 2–3% per year. The review also focuses on counterregulatory responses that modify the initial reduction in blood pressure after drug treatment for hypertension. It is concluded that proper understanding of the hemodynamic effects of antihypertensive agents is useful in the selection of the right treatment for specific groups of hypertensive patients.
Similar content being viewed by others
References
Lund-Johansen P. Hemodynamics in early essential hypertension.Acta Med Scand 1967;181(Suppl 482):1–101.
Tarazi RC, Ferrario CM, Dustan HP. The heart in hypertension. In: Genest J, Koiw E, Kuchel O, eds.Hypertension. New York: McGraw-Hill, 1977:738–754.
Werkø L, Lagerløf H. Studies on the circulation in man. IV. Cardiac output and blood pressure in the right auricle, right ventricle and pulmonary artery in patients with hypertensive cardiovascular disease.Acta Med Scand 1949;133:427–436.
Shapiro LM, Mackinnon K, Beevers DG. Echocardiographic features of malignant hypertension.Br Heart J 1981;46:374–379.
Pickering GW, Cranston WI, Pears MA.The treatment of hypertension. Springfield, IL: Charles C. Thomas, 1961.
Gudbrandsson T, Hanson L, Herlitz H, Andren L. Malignant hypertension—improving prognosis in a rare disease.Acta Med Scand 1979;206:495–499.
Tarazi RC. Reversal of cardiac hypertrophy by medical treatment.Annu Rev Med 1985;36:407–414.
Omvik P, Lund-Johansen P, Haugland M. Modest antihypertensive effect of epanolol, a beta1-selective receptor blocker with beta1-agonist activity. An acute and long-term hemodynamic study at rest and during exercise and double-blind crossover comparison with atenolol on ambulatory blood pressure.Cardiovasc Drugs Ther 1992;7:125–132.
Lund-Johansen P, Omvik P, Haugland H. Acute and chronic haemodynamic effects of doxazosin in hypertension at rest and during exercise.Br J Clin Pharmacol 1986;21(Suppl 1):45s-54s.
Lund-Johansen P, Omvik P, Nordrehaug JE, White W. Carvedilol in hypertension: Effects on hemodynamics and 24 hour blood pressure.J Cardiovasc Pharmacol 1992;19(Suppl 1):S27-S34.
Lund-Johansen P, Omvik P. Acute and chronic hemodynamic effects of drugs with different actions on adrenergic receptors: a comparison between alpha blockers and different types of beta blockers with and without vasodilating effect.Cardiovasc Drugs Ther 1991;5:605–616.
Lund-Johansen P, Omvik P, White W, et al. Long-term haemodynamic effects of amlodipine at rest and during exercise in essential hypertension.J Hypertens 1990;8:1129–1136.
Lund-Johansen P, Omvik P. Chronic hemodynamic effects of tiapamil and felodipine in essential hypertension at rest and during exercise.J Cardiovasc Pharmacol 1990;15(Suppl 4):S42-S47.
Lund-Johansen P, Omvik P. Effect of long-term diltiazem treatment on central haemodynamics and exercise endurance in essential hypertension.Eur Heart J 1990;11:543–551.
Omvik P, Lund-Johansen P. Comparison of long-term hemodynamic effects at rest and during exercise of lisinopril plus sodium restriction versus hydrochlorothiazide in essential hypertension.Am J Cardiol 1990;65:331–338.
Omvik P, Lund-Johansen P. Long-term effects on central haemodynamics and body fluid volumes of ketanserin in essential hypertension. Studies at rest and during dynamic exercise.J Hypertens 1983;1:405–412.
Omvik P, Lund-Johansen P. Is sodium restriction effective treatment of borderline and mild essential hypertension? A long-term haemodynamic study at rest and during exercise.J Hypertens 1986;4:535–541.
Lund-Johansen P. Spontaneous changes in central hemodynamics in essential hypertension—a 10-year follow-up study. In: Onesti G, Klimt CR, eds.Hypertension—Determinants, complications, and intervention. New York: Grune and Stratton, 1979:201–218.
Perera GA, Blood DW. The relationship of sodium chloride to hypertension.J Clin Invest 1947;26:1109–1118.
Dahl LK, Stall BG, Cotzias GC. Metabolic effects of marked sodium restriction in hypertensive patients: changes in total exchangable sodium and potassium.J Clin Invest 1954;33:1397–1406.
Parijs J, Joosens JV, van der Linden L, et al. Moderate sodium restriction and diuretics in the treatment of hypertension.Am Heart J 1973;85:22–34.
MacGregor GA, Markandu ND, Best FE, et al. Double-blind randomised crossover trial of moderate sodium restriction in essential hypertension.Lancet 1982;1:351–354.
Fagerberg B, Andersson OK, Isaksson B, Bjørntorp P. Blood pressure control during weight reduction in obese hypertensive men: separate effects of sodium and energy restriction.Br Med J 1984;288:11–14.
Law MR, Frost CD, Wald NJ. By how much does dietary salt reduction lower blood pressure? III-Analysis of data from trials of salt reduction.Br Med J 1991;30:819–824.
Lund-Johansen P. Central hemodynamic effects of beta-blockers in hypertension. A comparison between atenolol, metoprolol, timolol, penbutolol, alprenolol, pindolol and bunitrolol.Eur Heart J 1983;4(Suppl):1–12.
Kaiser P. Physical performance and muscle metabolism during beta-adrenergic blockade in man.Acta Physiol Scand 1984;(Suppl 576):1–53.
Cruickshank JM, Prichard BN, eds.Beta-blockers in clinical practice. Edinburgh: Churchill, Livingstone, 1987.
Smith HD, Halliday SE, Earl DCN, Stribling D. Effects of selective (beta1 and beta2) and nonselective beta-adrenoceptor antagonists on the cardiovascular and metabolic responses to isoproterenol: comparison with ici 141 292.J Pharmacol Exp Ther 1983;226:211–216.
Frohlich ED, Tarazi RC, Dustan HP, Page IH. The paradox of beta-adrenergic blockade in hypertension.Circulation 1968;37:417–423.
van Zwieten PA. Alpha-adrenoceptor-blocking agents in the treatment of hypertension. In: Laragh JH, Brenner BM, eds.Hypertension. Pathophysiology, diagnosis, and management. New York: Raven Press, 1990:2233–2249.
Omvik P, Lund-Johansen P. Review of central haemodynamic effects of alpha-blockers and their future use in hypertension.Br J Clin Practice 1987;41(Suppl 54):15–21.
Langer SZ. Presynaptic regulation of release of catecholamines.Pharmacol Rev 1981;32:337–362.
1988 Joint National Committee. The 1988 Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure.Arch Intern Med 1988;148:1023–1038.
Nayler WG.Calcium antagonists. London: Academic Press, 1988.
Editorial. Calcium antagonist caution.Lancet 1991;337:885–886.
Mroczek WJ, Burris JF, Allenby KS. A double-blind evaluation of the effect of amlodipine on ambulatory blood pressure in hypertensive patients.J Cardiovasc Pharmacol 1988;12(Suppl 7):S79-S84.
Lund-Johansen P. Hemodynamic effects of verapamil in essential hypertension at rest and during exercise.Acta Med Scand 1984;(Suppl 681):109–115.
Biollaz J, Schelling JL, Jacot Des Combes B, et al. Enalapril maleate and lysine analogue (MK 521) in normal volunteers: relationship between plasma drug levels and the renin angiotensin system.Br J Clin Pharmacol 1982;14:363–368.
Page IH. Serotonin (5-hydroxy-tryptamin).Physiol Rev 1954;34:563–588.
Vanhoutte P, Amery A, Birkenhager W, et al. Serotoninergic mechanisms in hypertension. Focus on the effects of ketanserin.Hypertension 1988;11:111–133.
Cameron HA, Waller PC, Ramsay LE. Ketanserin in essential hypertension: use as monotherapy and in combination with a diuretic or β-adrenoceptor antagonist.Br J Clin Pharmacol 1987;24:705–711.
Weiss YA, Safar ME, London GM, et al. Repeat hemodynamic determinations in borderline hypertension.Am J Med 1978;64:382–387.
Julius S, Quadir H, Gajendragadkar S. Hyperkinetic stage: a precursor of hypertension? A longitudinal study of border-line hypertension. In: Gross F, Strasser T, eds.Mild hypertension: Natural history and management.Proceedings of the Joint WHO/ISH meeting, Susono, Japan. Bath: Pitman Medical, 1979:116–126.
Andersson OK, Sannerstedt R, Beckman M, et al. Essential hypertension, implications for pathogenesis from repeated hemodynamic investigations in young men with elevated blood pressure.J Hypertens 1983;1(Suppl 2):91–93.
Birkenhäger WH, de Leeuw PW. Cardiac aspects of essential hypertension.J Hypertens 1984;2:121–125.
Fleg JL. Alterations in caridovascular structure and function with advancing age.Am J Cardiol 1986;57:33C-43C.
Lund-Johansen P. The dye dilution method for measurement of cardiac output.Eur Heart J 1990;11(Suppl 1):6–12.
de Leeuw PW, Birkenhäger WH. Some comments on the usefulness of measuring cardiac output by dye dilution.Eur Heart J 1990;11(Suppl 1):13–16.
Gould BA, Mann S, Davies AB, et al. Does placebo lower blood pressure?Lancet 1981;2:1377–1381.
Australian National Blood Pressure Management Committee. The Australian therapeutic trial in mild hypertension.Lancet 1980;1:1261–1267.
Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results.Br Med J 1985;291:97–104.
Mancia G, Casadei R, Groppeli A, et al. Effects of stress on the diagnosis of hypertension.Hypertension 1991;17(Suppl III):56–62.
Omvik P, Lund-Johansen P. The initial hemodynamic response to newer antihypertensive agents at rest and during exercise: review of visacor, doxazosin, nisoldipine, tiapamil, perindoprilat, pinacidil, dilevalol, and carvedilol.Cardiovasc Drugs Ther 1990;4:1135–1144.
Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context.Lancet 1990;335:827–838.
Liebson PR, Savage DD. Echocardiography in hypertension: a review. II. Echocardiographic studies of the effects of antihypertensive agents on left ventricular wall mass and function.Echocardiography 1987;4:215–249.
Sullivan JM, Ratts TE, Taylor JC, et al. Hemodynamic effects of dietary sodium in man. A preliminary report.Hypertension 1980;2:506–514.
Andersson OK, Fagerberg B, Hedner T. Importance of dietary salt in the hemodynamic adjustment to weight reduction in obese, hypertensive men.Hypertension 1984;6:814–819.
Menard J, Bellet M, Brunner HR. Clinical development of antihypertensive drugs. In: Laragh JH, Brenner BM, eds.Hypertension. Pathophysiology, diagnosis, and management. New York: Raven Press, 1990:2331–2342.
Cruickshank JM, Thorp JM, Zacharias FJ. Benefits and potential harm of lowering high blood pressure.Lancet 1987;1:581–584.
Page IH. Pathogenesis of arterial hypertension.JAMA 1949;140:451–458.
Brittain RT, Drew GM, Levy GP. The alpha and beta-adrenoceptor blocking properties of labetalol and its individual stereo-isomers in anaesthetized dogs and isolated tissues.Br J Pharmacol 1982;77:105–114.
Sponer G, Bartsch W, Strein K, et al. Pharmacological profile of carvedilol as a beta-blocking agent with vasodilating and hypertensive properties.J Cardiovasc Pharmacol 1986;8:317–327.
Lund-Johansen P. Hemodynamic effects on antihypertensive agents. In: Doyle AE, ed.Handbook of hypertension, Vol 5: Clinical pharmacology of antihypertensive drugs. Amsterdam: Elsevier, 1988:41–72.
James GD, Pickering TG, Yee LS, et al. The reproducibility of average ambulatory, home, and clinic pressures.Hypertension 1988;11:545–549.
Wilson NV, Meyer BM. Early prediction of hypertension using exercise blood pressure.Prev Med 1981;10:62–68.
Muller JE, Tofler CH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular events.Circulation 1989;79:733–743.
Fagard R, Bielen E, Hespel P, et al. Physical exercise in hypertension. In: Laragh JH, Brenner BM, eds.Hypertension. Pathophysiology, diagnosis, and management. New York, Raven Press, 1990:2233–2249.
Heber ME, Brigden GS, Caruana MP, et al. Carvedilol for systemic hypertension.J Cardiovasc Pharmacol 1987;10(Suppl 11):S113-S118.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Omvik, P., Lund-Johansen, P. Long-term hemodynamic effects at rest and during exercise of newer antihypertensive agents and salt restriction in essential hypertension: Review of epanolol, doxazosin, amlodipine, felodipine, diltiazem, lisinopril, dilevalol, carvedilol, and ketanserin. Cardiovasc Drug Ther 7, 193–206 (1993). https://doi.org/10.1007/BF00878508
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00878508