Abstract
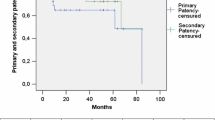
The purpose of this study was to review our results with axillofemoral by-passes performed for aortoiliac occlusive disease. Fifty patients receiving 51 axillofemoral by-passes from January 1989 to December 1994 were retrospectively reviewed. The 30-day post-operative mortality was 4%. Seven patients (14%) presented graft-related local complications and all but one required reoperation. Five patients were lost to follow-up, the mean length of which was 36 months (16–74 months). Forty-nine per cent of the patients died during the follow-up period. At 36 months, the primary patency rate was 51%, the secondary patency rate was 69%, and limb valvage rate was 87%. A statistical difference was seen in the secondary patency rate between axillobifemoral by-pass (87%) and axillo-unifemoral by-pass (56%) at 36 months (P<0.01), but no difference was seen in the limb salvage rate at 36 months between the two configurations of the by-pass (94% vs 81 %) (P=NS). Twenty patients (40%) operated upon for acute ischemia had a significantly higher post-operative mortality rate (10% vs 0), a significantly higher amputation rate (20% vs 6.6%) and a significantly lower patency rate of by-pass (26% vs 63%) (P<0.01), than the 30 patients (60%) operated on for claudication, rest pain or trophic ulcers. Our findings indicate that the results of axillofemoral by-pass are significantly influenced by the selection of patients for operation, namely the clinical status of ischaemic symptoms, and that since the overall results of axillofemoral by-pass are inferior to those of aortofemoral by-pass, this treatment should be restricted to patients at high risk of aortic clamping.
Zusammenfassung
Es wurden 51 axillofemorale By-passoperationen aus dem Zeitraum Januar 1989 bis Dezember 1994 retrospektiv analysiert. Die postoperative Mortalitätsrate (nach 30 Tagen) betrug 4%. Bei 7 Patienten (14%) traten am Graft Komplikationen ein, so daß 6 von ihnen reoperiert werden mußten. In die Nachuntersuchung (mittleres Follow-up: 36 Monate, Spanne: 16–74 Monate) konnten 5 Patienten nicht einbezogen werden. Während der Follow-up-Periode verstarben 49% der Patienten. Nach 36 Monaten betrug die primäre Durchflußwiederherstellungsrate 51%, die sekundäre 69%, die Sanierungsrate im betroffenen Glied 87%. Statistisch gab es nach 36 Monaten bei der sekundären Durchflußwiederherstellungsrate einen Unterschied zwischen axillo-bifemoralen (87%) und axillo-uni-femoralem Bypass (56%) (p<0,01), aber hinsichtlich der Heilungsrate gab es zu diesem Zeitpunkt zwischen den beiden Bypass-Arten keinen signifikanten Unterschied (94% vs. 81%). Die postoperative Mortalitätsrate war bei 20 Patienten (40%), die wegen akuter Ischämie operiert worden waren, signifikant höher (10% vs. 0%); ebenso die Amputationsrate (20% vs. 6,6%); signifikant niedriger hingegen war die Durchflußwiederherstellungsrate nach Bypass (26% vs. 63%) (p<0,01) —im Vergleich zu 30 Patienten (60%), die wegen Claudicatio, Ruheschmerz oder trophischen Ulzera operiert worden waren. Nach unseren Untersuchungen sind die Ergebnisse bei axillofemoralen Bypassoperationen entscheidend abhängig von der Auswahl der Patienten gemäß klinischem Zustand und ischämischen Symptomen. Die Gesamtergebnisse nach axillofemoralem Bypass sind schlechter als nach aortofemoralem Bypass, und darum sollte die erstgenannte Operation nur bei Patienten angewendet werden, bei denen die Abklemmung der Aorta ein hohes Risiko darstellen würde.
Similar content being viewed by others
References
Blaisdell FW, Hall AD (1963). Axillary femoral artery by-pass for lower extremity ischemia. Surgery 54:563–568
Louw JH (1963) The treatment of combined aortoiliac and femoral popliteal occlusive disease by splenofemoral and axillofemoral by-pass graft. Surgery 55:387–395
Koskas F, Bahnini A, Ruotolo C, Kieffer E (1991) Techniques et indications des pontages axillo-femoraux. In: Kiefer E (ed) Les Lésions occlusives aorto-iliaques chroniques. AERCV Paris, pp 57–73
Alpert J, Brief DK, Parsonnet V (1967) Vascular restoration for aortoiliac occlusion and an alternative approach to the poor risk patient. J Newark Beth Israel Hosp 18:4–8
Johnson WC, Logerfo FW, Vollmar RW et al (1976) Is axillo bilateral femoral graft an effective substitute for aorto bilateral iliac femoral graft? Ann Surg 186:123–129
Mason RA, Smirnov VB, Newton GB, Giron F (1989) Alternative procedure to aorto bifemoral by-pass grafting. J Cardiovasc Surg 30:192–197
Harris EJ, Taylor LM, McConnel DB, Moneta GL, Yeager RA, Porter JM (1990) Clinical results of axillobifemoral by-pass using externally supported polytetrafluoroethylene. J Vase Surg 12:416–421
Rutherford RB, Flanigan DP, Gupta SK et al (1986) Suggested standards for reports dealing with lower extremity ischemia. J Vase Surg 4:80–94
Moore WD, Hall AD, Blaisdell FW (1971) Late results of axillary-femoral by-pass grafting. Am J Surg 122:148–154
Rutherford RB, Patt A, Pearce WH (1987) Extra-anatomic by-pass: a closer view. J Vase Surg 6:437–446
Eugene J, Goldstone J, Moore WS (1977) Fifteen-year experience with subcutaneous by-pass grafts for lower extremity ischemia. Ann Surg 186:177–183
Logerfo FW, Johnson WC, Corson JD et al (1977) A comparison of the late patency rates of axillo-bilateral femoral and axillounilateral femoral grafts. Surgery 81:33–40
Ray LI, O'Connor JB, David CC et al (1979) Axillofemoral by-pass: a critical reappraisal of its role in the management of aortoiliac occlusive disease. Am J Surg 138:117–128
Donaldson MC, Louras JC, Bucknam CA (1986) Axillofemoral by-pass: a toll with a limited role. J Vase Surg 3:757–763
Kalman PG, Hosang M, Cina et al (1987) Current indications for axillo-femoral and axillo-bifemoral by-pass grafts. J Vase Surg 5:828–832
Rutherford RB, Patt A, Pearce WH (1987) Extra-anatomic by-pass: a closer review. J Vase Surg 6:437–446
El Massry S, Saad E, Sauvage LR et al (1993) Axillofemoral by-pass with externally supported, knitted Dacron grafts: a follow-up through twelve years. J Vase Surg 17:107–115
Bacourt F (1993) Le pontage axillo-fémoral trente ans après. In: Fichelle JM (ed) Techniques et stratégie en chirurgie vasculaire. AERCV Paris 147–165
Blaisdell FW (1988) Extraanatomic by-pass procedures. World J Surg 12:798–804
Burrel MJ, Wheeler JR, Gregory RT, Snyder SO, Gayle RG, Mason MS (1982) Axillofemoral by-pass a ten year review. Ann Surg 195:796–799
Veith FJ (Discussant) (1993) J Vase Surg 17:107–115
Cavallaro A, Sciacca V, Di Marzo L, Bovxe S, Mingoli A (1988) The effect of body weight compression on axillo-femoral by-pass patency. J Cardiovasc Surg 29:476–479
Jarowenko MV, Buchbinder D, Shah DM (1981) Effect of external pressure on axillofemoral by-pass grafts. Ann Surg 193:274–276
Ascer E, Veith FJ, Gupta SK et al (1984) Comparison of axillounifemoral and axillobifemoral by-pass operations. Surgery 97:169–174
Agee JM, Kron IL, Flanagan T, Tribble CG (1991) The risk of axillofemoral by-pass grafting for acute vascular occlusion. J Vasc Surg 14:190–194
Moore WS (Discussant) (1990) J Vasc Surg 12:416–421
Schneider JR, McDaniel MD, Walsh DB, Zwoldak RM, Cronenwett JL (1992) Axillofemoral by-pass: outcome and hemodynamic results in high-risk patients. J Vasc Surg 15:952–963
Bergan JJ, Yao J (1985) Complications of extra-anatomic bypass grafting to the lower extremity. In: Bergan JJ, Yao J (eds.). Complications in vascular surgery, 2nd edn. Grune and Stratton, Orlando, pp 55–60
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Illuminati, G., Calio, F.G., Mangialardi, N. et al. Results of axillofemoral by-passes for aorto-iliac occlusive disease. Langenbecks Arch Chiv 381, 212–217 (1996). https://doi.org/10.1007/BF00571687
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF00571687