Abstract
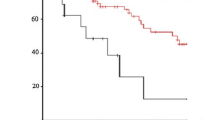
A study of risk factors that affect morbidity and mortality in 523 patients with squamous cell cancer of the esophagus who had one-stage resection was undertaken. The 30-day and hospital mortality rates were 5.0% and 15.5%, respectively. Pulmonary complications, malignant cachexia, and surgical complications accounted for 42%, 25%, and 21% of hospital deaths, respectively. Major pulmonary complications occurred in 23% of patients. Multivariate analysis identified six factors that predicted major pulmonary complications: age, mid-arm circumference, percent of predicted FEV1, abnormal chest radiograph, amount of blood loss, and palliative resection. Three risk groups of pulmonary complications were identified: low, median, and high risk group with complications in 3%, 17%, and 43% of patients, respectively. Significantly, patients with curative resection had a lower hospital mortality rate (9%) than those with palliative resection (20%), p=0.001. Patients with stage I, IIa, or IIb disease had a lower hospital mortality rate (9%) than those with stage III or IV disease (18%), p=0.026. Multivariate analysis identified six factors that predicted hospital death: age, mid-arm circumference, history of smoking, incentive spirometry, number of stairs climbed, and amount of blood loss. Three risk groups of hospital death were identified: low, median, and high risk groups with death in 7%, 30%, and 38%, respectively. Anastomotic leakage rate was 4%. Technical faults were identified in 53% of patients with leakage. Together with other surgical complications, a presumed or apparent technical error was noted in 63% of patients. The identification of high-risk patients and prevention of technical faults can help improve surgical outcome.
Résumé
Dans cette étude, on a étudié les facteurs de risque influençant la morbidité et la mortalité chez 523 patients ayant un cancer épidermoïde de l'oesophage et ayant eu une résection en un seul temps. La mortalité à 30 jours et la mortalité hospitalière ont été respectivement de 5% et de 15.5%. Les complications pulmonaires, la cachexie maligne et les complications chirurgicales ont été responsable respectivement de 42%, 25% et 21% des décès hospitaliers. Une analyse multifactorielle a permis d'identifier six facteurs prédictifs des complications pulmonaires: l'âge, la circonférence brachiale, la prévision du volume expiratoire forcé en une seconde, les anomalies de la radiographie thoracique, la quantité de sang perdu, et le caractère palliatif de la résection. Trois groupes, dont le risque de complications pulmonaires a été classé faible, moyen et élevé, ont été identifiés. Le taux de complications dans ces groupes ont été respectivement de 3%, 17% et 43%. Les patients ayant eu une résection à visée curative avaient une mortalité hospitalière significativement plus basse (9%) comparée à celle des patients ayant eu une résection à visée palliative (20%) (p=0.001). Les patients ayant des maladies de stades I, IIa, IIb avaient une mortalité plus basse (9%) que ceux qui avaient des stades III ou IV (18%), (p=0.026). L'analyse multifactorielle a permis d'identifier six facteurs prédictifs de la mortalité hospitalière: l'âge, la circonférence brachial, des antécédents de consommation excessive du tabac, la spirométrie, le nombre d'escaliers que le patient peut monter, et la quantité de sang perdu. Trois groupes de patients, dont le risque de mortalité hospitalière a été classé faible, moyen, et élevé, ont eu des décès dans respectivement 7%, 30% et 38% des cas. Le taux de fistule a été de 4%. Une faute technique a été identifiée chez 53% des patients ayant eu une fistule. Une faute technique apparente ou présumée a été identifie chez 63% des patients ayant eu soit une fistule soit une complication chirurgicale. L'identification des patients à haut risque et la prévention des fautes techniques peuvent contribuer à améliorer le pronostic après chirurgie.
Resumen
Se emprendió un estudio sobre los factores de riesgo que afectaron la mortalidad en 523 pacientes con carcinoma escamocelular del esófago sometidos a resección en una etapa en nuestra institución.
Las tasas de mortalidad a 30 días y de mortalidad hospitalaria fueron 5% y 15%. Las complicaciones pulmonares, caquexia maligna y quirúrgica representaron 42%, 25% y 21% de las muertes hospitalarias, respectivamente. Complicaciones pulmonares mayores fueron registradas en 23% de los pacientes.
El análisis multivariado identificó seis factores que predicen complicaciones pulmonares mayores: edad, circunferencia del brazo, porcentaje del FEV1 predecible, radiografía de tórax anormal, pérdida de sangre durante la operación y resección de tipo paliativo. Se identificaron tres grupos de riesgo de desarrollar complicaciones pulmonares: bajo, medio y alto, con tasas de 3%, 17% y 43% de los pacientes, respectivamente. Los pacientes que recibieron resección curative exhibieron una significativamente menor tasa de mortalidad hospitalaria (9%) en comparación con los que recibieron resección paliativa (20%), p=0.001. Los pacientes con enfermedad en estados I, IIa, IIb exhibieron menor mortalidad hospitalaria (9%) en comparación con los estados III o IV (18%), p=0.026. El análisis multivariado identificó seis factores que predicen mortalidad hospitalaria: edad, circunferencia del brazo, historia de tabaquismo, espirometría de incentivo, número de escalones que puede ascender y pérdida de sangre durante la operación. Se identificaron tres grupos de riesgo de mortalidad hospitalaria: bajo, medio y alto, con tasas de 7%, 30% y 38% respectivamente.
La tasa de fuga anastomótica fue 4% y se identificaron defectos técnicos en 53% de los pacientes. Junto con otras complicaciones quirúrgicas, se observó un error técnico presumible o aparente en 63% de los pacientes.
La identificación de los pacientes de alto riesgo y la prevención de los errores técnicos pueden ayudar a mejorar el pronóstico.
Similar content being viewed by others
References
Earlam, R., Cunha-Melo, J.R.: Oesophageal squamous cell carcinoma. I. A critical review of surgery. Br. J. Surg. 67:381, 1980
Muller, J.M., Erasmi, H., Stelzner, M., Zieren, U., Pichlmaier, H.: Surgical therapy of oesophageal carcinoma. Br. J. Surg. 77:845, 1990
DeMeester, T.R., Barlow, A.P.: Surgery and current management for cancer of the esophagus and cardia. Curr. Probl. Surg. 25:475, 1988
Huang, G.J., Gu, X.Z., Wang, L.J.: Experience with combined preoperative irradiation and surgery for carcinoma of the esophagus. Gann Monogr. Cancer Res. 31:159, 1986
Law, S.Y.K., Fok, M., Cheng, S.W.K., Wong, J.: A comparison of outcome after resection for squamous cell carcinomas and adenocarcinomas of the esophagus and cardia. Surg. Gynecol. Obstet. 175:107, 1992
Couraud, L., Velly, J.F., Clerc, P., Martigne, C.: Experience of partial oesophagectomy in surgical treatment of lower and middle thoracic oesophageal cancer: from a follow-up of 366 cases. Eur. J. Cardiothorac. Surg. 3:99, 1989
Mansour, K.A., Downey, R.S.: Esophageal carcinoma: surgery without preoperative adjuvant chemotherapy. Ann. Thorac. Surg. 48:201, 1989
Wong, J.: Esophageal resection for cancer: the rationale of current practice. Am. J. Surg. 153:18, 1987
Wong, J.: Stapled esophagogastric anastomosis in the apex of the right chest after subtotal esophagectomy for carcinoma. Surg. Gynecol. Obstet. 164:568, 1987
Fok, M., Siu, K.F., Wong, J.: A comparison of transhiatal and transthoracic resection for carcinoma of the thoracic esophagus. Am. J. Surg. 158:414, 1989
Fok, M., Wong, J.: Esophagogastrectomy for carcinoma of the abdominal esophagus and gastric cardia. In: Mastery of Surgery (2nd ed.), L.M. Nyhus, R.J. Baker, editors. Boston, Little, Brown, 1992, pp. 731–741
American Joint Committee on Cancer: Manual for Staging of Cancer (3rd ed.) O.H. Beahrs, D.E. Henson, R.V.P. Hutter, M.H. Myers, editors. Philadelphia, Lippincott, 1988, pp. 63–67
Giuli, R., Sancho-Garnier, H.: Diagnostic, therapeutic, and prognostic features of cancers of the esophagus: results of the international prospective study conduced by the OESO group (790 patients). Surgery 99:614, 1986
Postlethwait, R.W.: Complications and deaths after operations for esophageal carcinoma. J. Thorac. Cardiovasc. Surg. 85:827, 1983
Collard, J.M., Otte, J.B., Reynaert, M., Michel, L., Carlier, M.A., Kestens, P.J.: Esophageal resection and bypass: a 6 year experience with a low postoperative mortality. World J. Surg. 15:635, 1991
Nishi, M., Hiramatsu, Y., Hioki, K., Hatano, T., Yamamoto, M.: Pulmonary complications after subtotal oesophagectomy. Br. J. Surg. 75:527, 1988
Peracchia, A., Bardini, R., Ruol, A., et al.: Carcinoma of the esophagus in the elderly (70 years of age or older): indications and results of surgery. Dis. Esophagus 1:147, 1988
Tsutsui, S., Moriguchi, S., Morita, M., et al.: Multivariate analysis of postoperative complications after esophageal resection. Ann. Thorac. Surg. 53:1052, 1992
Elman, A., Boudinet, A., Flamant, Y.: Contraindications related to respiratory function. In Cancer of the Esophagus in 1984, 135 Questions. First Polydisciplinary International Congress of OESO (answers compiled by R. Giuli). Paris, Maloine, 1984, pp. 18–21
Nishi, N., Hiramatsu, Y., Hioki, K., et al.: Risk factors in relation to postoperative complications in patients undergoing esophagectomy or gastrectomy for cancer. Ann. Surg. 207:148, 1988
Kawaguchi, Y.: Preoperative assessment for the risk of postoperative pulmonary complications in patients with esophageal cancer. Nippon Geka Gakkai Zasshi 91:1667, 1990
Toyoizumi, S., Usui, S., Sakamoto, A., et al.: Study of risk factors for postoperative pulmonary complications following esophageal cancer surgery—multivariate statistical analysis. Nippon Kyobu Geka Gakkai Zasshi 38:215, 1990
Fan, S.T., Lau, W.Y., Yip, W.C., et al.: Prediction of postoperative pulmonary complications in oesophagogastric cancer surgery. Br. J. Surg. 74:408, 1987
Jewell, E.R., Persson, A.V.: Preoperative evaluation of the high risk patients. Surg. Clin. North Am. 65:3, 1985
Ergina, P.L., Gold, S.L., Meakins, J.L.: Perioperative care of the elderly patient. World J. Surg. 17:192, 1993
Bartlett, R.H., Gazzaniga, A.B., Geraghty, T.R.: Respiratory maneuvers to prevent postoperative pulmonary complications. J.A.M.A. 224:1017, 1973
Hall, J.C., Tarala, R., Harris, J., Tapper, J., Christiansen, K.: Incentive spirometry versus routine chest physiotherapy for prevention of pulmonary complications after abdominal surgery. Lancet 337:953, 1991
Van Nostrand, D., Kjelsberg, M.O., Humphrey, E.W.: Preresectional evaluation of risk from pneumonectomy. Surg. Gynecol. Obstet. 127:306, 1968
Windsor, J.A., Hill, G.L.: Risk factors for postoperative pneumonia: the importance of protein depletion. Ann. Surg. 208:209, 1988
Brandmair, W., Lehr, L., Siewert, J.R.: Nutritional status in esophageal cancer: assessment and significance for preoperative risk assessment. Langenbecks Arch. Chir. 374:25, 1989
Pettigrew, R.A., Hill, G.L.: Indicators of surgical risk and clinical judgement. Br. J. Surg. 73:47, 1986
Daly, J.M., Massar, E., Giacco, G., et al.: Parenteral nutrition in esophageal cancer patients. Ann. Surg. 196:203, 1982
Muller, J.M., Dienst, C., Brenner, U., Pichlmaier, H.: Preoperative parenteral feeding in patients with gastrointestinal carcinoma. Lancet 1:68, 1982
Moghissi, K., Hornshaw, J., Teasdale, P.R., Dawes, E.A.: Parenteral nutrition in carcinoma of the oesophagus treated by surgery: nitrogen balance and clinical studies. Br. J. Surg. 64:125, 1977
Lim, S.T.K., Choa, R.G., Lam, K.H., Wong, J., Ong, G.B.: Total parenteral nutrition versus gastrostomy in the preoperative preparation of patients with carcinoma of the oesophagus. Br. J. Surg. 68:69, 1981
Fan, S.T., Lau, W.Y., Wong, K.K., Chan, Y.P.M.: Preoperative parenteral nutrition in patients with oesophageal cancer: a prospective, randomised, clinical trial. Clin. Nutr. 8:23, 1989
Siewert, J.R.: Esophageal cancer from the German point of view. Jpn. J. Surg. 19:11, 1989
Orringer, M.B., Marshall, B., Stirling, M.C.: Transhiatal esophagectomy for benign and malignant disease. J. Thorac. Cardiovasc. Surg. 105:265, 1993
Fok, M., Cheng, S.W.K., Wong, J.: Endosonography in patient selection for surgical treatment of esophageal carcinoma. World J. Surg. 16:1098, 1992
Bumm, R., Holscher, A.H., Feussner, H., Tachibana, M., Bartels, H., Siewert, J.R.: Endodissection of the thoracic esophagus: technique and clinical results in transhiatal esophagectomy. Ann. Surg. 218:97, 1993
Dewar, L., Gelfand, G., Finley, R.J., Evans, K., Inculet, R., Nelems, B.: Factors affecting cervical anastomotic leak and stricture formation following esophagogastrectomy and gastric tube interposition. Am. J. Surg. 163:484, 1992
Wong, J., Cheung, H., Lui, R., Fan, Y.W., Smith, A., Siu, K.F.: Esophagogastric anastomosis performed with a stapler: the occurrence of leakage and stricture. Surgery 101:408, 1987
Fok, M., Ah-Chong, A.K., Cheng, S.W.K., Wong, J.: Comparison of a single layer continuous hand-sewn method and circular stapling in 580 oesophageal anastomoses. Br. J. Surg. 78:342, 1991
Lam, T.C.F., Fok, M., Cheng, S.W.K., Wong, J.: Anastomotic complications after esophagectomy for cancer: a comparison of neck and chest anastomoses. J. Thorac. Cardiovasc. Surg. 104:395, 1992
Hermreck, A.S., Crawford, D.G.: The esophageal anastomotic leak. Am. J. Surg. 132:794, 1976
Chasseray, V.M., Kiroff, G.K., Buard, J.L., Launois, B.: Cervical or thoracic anastomosis for esophagectomy for carcinoma. Surg. Gynecol. Obstet. 169:55, 1989
Fok, M., Cheng, S.W.K., Wong, J.: Pyloroplasty versus no drainage in gastric replacement of the esophagus. Am. J. Surg. 162:447, 1991
Matthews, H.R., Powell, D.J., McConkey, C.C.: Effect of surgical experience on the results of resection for oesophageal carcinoma. Br. J. Surg. 73:621, 1986
Lorentz, T., Fok, M., Wong, J.: Anastomotic leakage after resection and bypass for esophageal cancer: lessons learned from the pats. World J. Surg. 13:472, 1989
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Law, S.Y.K., Fok, M. & Wong, J. Risk analysis in resection of squamous cell carcinoma of the esophagus. World J. Surg. 18, 339–346 (1994). https://doi.org/10.1007/BF00316812
Issue Date:
DOI: https://doi.org/10.1007/BF00316812