Summary
The objective of the study was to compare compliance with and the hypocholesterolaemic effect of lovastatin given once daily as a morning or an evening dose. Twenty-four out-patients with familial hypercholesterolaemia were randomly assigned to receive placebo first, then lovastatin 20 mg, to be taken once daily for 4 weeks, either with the breakfast or evening meal, in a single-blind fashion.
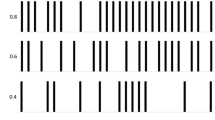
Drug compliance was assessed by pill counts and continuous electronic monitoring. Two compliance parameters were evaluated, consumption, defined as percentage of prescribed doses taken, and time compliance, the percentage of total dosing events recorded within defined intervals (6.00–10.00 h, and 17.00–21.00 h), for the morning and evening regimes.
Both regimes satisfactorily reduced the total and LDL-cholesterol concentrations, and there was no significant difference in the extent of the reductions.
Pill counts overestimated compliance, as revealed by the monitoring method. The times of actual consumption of doses by the patients often differed from that prescribed, predominantly in patients who were told to take the evening dose. Partial time compliance may have confounded the efficacy of the drugs. Electronic compliance monitoring appears to be particularly useful in chronopharmacological studies.
Similar content being viewed by others
References
Parker TS, McNamara DJ, Brown CD, Kolb R, Ahrens Jr EH (1984) Plasma mevalonate as a measure of cholesterol synthesis in man. J Clin Invest 74: 795–804
Wuttke H, Papalexiou P, Kasper FR (1983) Zum optimalen Einnahmezeitpunkt von Lipanthyl R250 Retard Kapseln. Therapiewoche 33: 6913–6922
Peters JR, Hunninghake DB (1985) Effect of time of administration of cholestyramine on plasma lipids and lipoproteins. Artery 13: 1–6
Illingworth DR (1986) Comparative efficacy of once versus twice daily mevinolin in the therapy of familial hypercholesterolemia. Clin Pharmacol Ther 40: 338–343
Hanefeld M, Lang PD, Fischer S, Leonhardt W, Bergman S, Jaroß W (1988) Effects of bezafibrate sustained release formulation on plasma lipoproteins in patients with hypercholesterolemia. Importance of timing of tablet intake for efficacy. Drug Res 38: 1835–1837
Furjimura A, Ohashi K, Ebihara A (1992) Time-dependent change in the effect of probucol in subjects with elevated cholesterol. Eur J Clin Pharmacol 43: 299–301
Hanefeld M (1989) Timing of intake of lipid lowering drugs: is that of importance? Klin Wocheschr 67: 511–512
Anon. (1991) Patient compliance in clinical trials. Lancet 337: 823–824
Pullar T (1991) Compliance with drug treatment. Br J Clin Pharmacol 32: 535–539
Pullar T, Kumar S, Tindall H, Feely M (1989) Time to stop counting the tablets? Clin Pharmacol Ther 46: 163–168
Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Quellette VL (1989) How often is medication taken as prescribed? A novel assessment technique. JAMA 261: 3273–3277
Mäenpää H, Manninnen V, Heinonen OP (1987) Comparison of the digoxin marker with capsule counting and compliance questionnaire methods for measuring compliance to medication in a clinical trial. Eur Heart J [Suppl I]: 39–43
Norell SE (1981) Monitoring compliance with pilocarpine therapy. Am J Ophthalmol 92: 727–731
Eisen SA, Woodward RS, Miller D, Spitznagel E, Windham CA (1987) The effect of medication compliance on the control of hypertension. J Gen Intern Med 2: 298–305
Cheung R, Dickins J, Nicholson PW, Thomas ASC, Smith HH, Larson HE, Desmukh AA, Dobbs RJ, Dobbs SM (1988) Compliance with antituberculous therapy: a field trial of a pill-box with a concealed recording device. Eur J Clin Pharmacol 35: 401–407
Kruse W, Weber E (1990) Dynamics of drug regimen compliance — its assessment by microprocessor-based monitoring. Eur J Clin Pharmacol 38: 561–565
Averbuch M, Weintraub M, Pollack DJ (1990) Compliance assessment in clinical trials: the MEMS device. J Clin Pharmacoepidemiol 4: 199–204
Kruse W, Eggert-Kruse W, Rampmaier J, Runnebaum B, Weber E (1991) Dosage frequency and drug-compliance behaviour — a comparative study on compliance with medication to be taken twice or four times daily. Eur J Clin Pharmacol 41: 589–592
Kruse W, Schlierf G, Weber E (1989) Continuous compliance monitoring — its utility for the interpretation of drug trials. Eur J Clin Pharmacol 36 [Suppl 1]: 289
Schlierf G, Schuler G, Wirth A, Kohlmeier M, Vogel G (1988) Treatment of coronary heart disease by diet and exercise: fasting and diurnal lipoproteins. Klin Wochenschr 66: 1103–1109
Rudd P, Byyny RL, Zachary V, Lo Verde ME, Mitchell WD, Titus C, Marshall M (1988) Pill count measures of compliance in a drug trial, variability and suitability. Am J Hypertens 1: 309–312
Cramer JA, Quelette VL, Mattson RH (1990) Effect of microelectronic observation on compliance. Epilepsia 31: 617–618
Henwood JM, Heel RC (1988) Lovastatin A preliminary review of its pharmacologic properties and therapeutic use in hyperlipidaemia. Drugs 36: 429–454
Cochrane AL (1972) Effectiveness and efficiency — Random reflections on health services. The Nuffield Provincial Hospitals Trust, Nuffield
Rudd P, Ahmed S, Zachary V, Barton C, Bonduelle D (1990) Improved compliance measures: applications in an ambulatory hypertensive drug trial. Clin Pharmacol Ther 48: 676–685
Vander Stichele RH, Thomson M, Verkoelen K, Droussin AM (1992) Measuring patient compliance with electronic monitoring: lisinopril versus atenolol in essential hypertension. Post Market Surv 6: 77–90
Infratest Gesundheitsforschung (1990) Compliance, München
Bradford RH, Shear CL, Chremos AN, Dujovne C, Downton M, Franklin FA, Gould AL, Hesney M, Higgins J, Hurley DP, Langendorfer A, Nash DT, Pool JL, Schnapper H (1991) Expanded clinical evaluation of lovastatin (EXCEL) study results. Arch Intern Med 151: 43–49
Author information
Authors and Affiliations
Additional information
Professor Ellen Weber died on 7th December 1992
Rights and permissions
About this article
Cite this article
Kruse, W., Nikolaus, T., Rampmaier, J. et al. Actual versus prescribed timing of lovastatin doses assessed by electronic compliance monitoring. Eur J Clin Pharmacol 45, 211–215 (1993). https://doi.org/10.1007/BF00315385
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00315385