Abstract
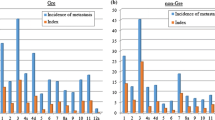
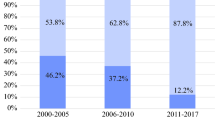
Surgery for gastric cancer in Japan has frequently been combined with resection of the spleen (splenectomy) or of the pancreatic body and tail and spleen (pancreatosplenectomy, PS). Splenectomy in patients with gastric cancer has been performed with two major purposes in mind: (1) curability of the cancer and (2) immunologic reasons. Direct cancerous invasion to the pancreas requires PS, although examination of these cases revealed that in 34.3% of such macroscopic invasions only fibrous adhesion to pancreas existed. Metastases to lymph nodes at the splenic hilus (no. 10) or along the splenic artery (no. 11) also required splenectomy. The incidences of no. 10 or no. 11 lymph node metastasis were as high as 26.7% and 22.2% respectively, for cancers of whole stomach, and 15.5% and 12.1% for cancers of the upper portion of stomach. Concerning the immunologic aspect of splenectomy for gastric cancer, the reports of fundamental research and clinical studies suggest that the spleen plays sometimes acts as a suppressor and at other times as a helper to the tumor activity, according to the number of tumor cells. From these data, we concluded that the spleen should be preserved in stage I, II, and III patients with curative operation; for stage IV patients the spleen should be resected. The immunologic significance of splenectomy should be clarified precisely in the near future.
Résumé
Dans la chirurgie pour cancer gastrique au Japon, on associe souvent à la gastrectomie la résection soit de la rate (splénectomie), soit de la queue voire du corps du pancréas et de la rate (splénopancréatectomie gauche ou SPG). Les indications de la splénectomie en matière de gastrectomie pour cancer gastrique se divisent en deux catégories: 1) splénectomie dont le but est la guérison du cancer; 2) splénectomie pour des raisons immunologiques. L'indication principale de la SPG est l'envahissement direct du pancréas par le cancer (bien que dans 34.3% des cas, l'envahissement apparent s'est révélé être seulement l'existence d'adhérences fibreuses). Des métastases soit au niveau des ganglions lymphatiques du hile de la rate (no 10), soit le long de l'artère splénique (no 11), nécessitent aussi une splénectomie. L'incidence des métastases lymphatiques des ganglions no 10 ou 11 est de 26.7% et de 22.2%, respectivement, dans les cancers de l'estomac dans leur ensemble, et de 15.5% et de 12.1%, respectivement, dans les cancers du tiers proximal de l'estomac. En ce qui concerne la splénectomie pour des raisons immunologiques, les expériences des recherches fondamentale et clinique suggèrent que la rate jour un rôle soit de «suppresseur» soit de «helper» de l'activité tumorale, selon la quantité de cellules tumorales. A partir de ces données, on conclue que la rate doit être conservée dans les stades I, II, et III chez les patients ayant une résection à visée curative. Ceux du stade IV doivent avoir une splénectomie. Les indications de la splénectomie pour des raisons immunologiques restent à éclaircir.
Resumen
En la cirugía para cáncer gástrico la resección combinada del bazo (esplenectomía) o del cuerpo y cola del páncreas y el bazo (pancreatoesplnectomía, PE) ha sido practicada frecuentemente en el Japón. Las indicaciones para esplenectomía en cáncer gástrico se dividen de acuerdo a dos propósitos principales: 1) esplenectomía orientada a la curación del cáncer. 2) esplenectomía desde el punto de vista inmunológico. La invasión cancerosa directa del páncreas requirió PE, aunque 34.3% de tales invasiones macroscópica revelaron sólo adherencias fibrosas al páncreas. La presencia de metástasis a los ganglios linfáticos del hilio esplénico (grupo ganglionar 10) o a lo largo de la arteria esplénica (grupo ganglionar 11) también requirió esplenectomía. La incidencia de metástasis a los grupos ganglionares 10 u 11 ascendieron hasta 26.7%, 22.2% en los cánceres de la totalidad del estómago y 15.5%, 12.1% en los cánceres de la porción superior del estómago, respectivamente. En relación a los aspectos inmunológicos de la esplenectomía para cáncer gástrico, los informes de investigación básica así como los estudios clínicos sugieren que el bazo puede jugar un papel en ocasiones como supresor y en otros como ayudador de la actividad tumoral de acuerdo con el número de células cancerosas. Con base en tales datos, el bazo debería ser preservado en los pacientes en estado I, II y III en quienes se emprende operación curativa, aunque el bazo tenga que ser resecado en los pacientes en estado IV. La significación inmunológica de la esplenectomía debe ser clarificada con mayor precisión en el futuro.
Similar content being viewed by others
References
UICC: TNM Classification of Malignant Tumours (4th ed.), P. Hermanek, L.H. Sobin, editors. Berlin, Springer-Verlag, 1987
Japanese Research Society for Gastric Cancer: The general rules for the gastric cancer study in surgery and pathology. Jpn. J. Surg. 11:127, 1981
Kanai, H.: Significance of combined pancreatosplenectomy in gastric resection for gastric carcinoma. J. Jpn. Soc. Cancer Ther. 2:328, 1967 (in Japanese)
Kajitani, T., Hoshino, T.: Combined resection of pancreas in gastric cancer. Gekachiryo 10:80, 1964 (in Japanese)
Aikou, T.: Clinicopathological study on the significance of combined pancreatosplenectomy, especially, gross indication of the basis on the base of oncological features. Igakukenkyu 50:533, 1980 (in Japanese)
Maruyama, K., Okabayashi, K., Kinoshita, T.: Progress in gastric cancer surgery in Japan and its limits of radicality. World J. Surg. 11:418, 1987
Jinnai, D., Ono, M., Sakakihara, N., Uda, T., Chikuba, H.: Extended radical surgery for gastric cancer. Syujutu 15:11, 1961 (in Japanese)
Sugimachi, K., Kodama, Y., Okamura, K., Shiraishi, M., Kuwano, H., Iguchi, K.: Splenectomy in total gastrectomy. Syujutu 36:337, 1982 (in Japanese)
Toge, T., Hamamoto, S., Itagaki, E., et al.: Concanavalin-A induced and spontaneous suppressor cell activities in spleen cells from gastric cancer patients. Cancer 52:1624, 1983
Yoshino, K., Kumai, K., Asanuma, S., Ishibiki, H.: Is a splenectomy in the operation for gastric carcinoma useful or harmful to survival? Rinsyogeka 39:1539, 1984 (in Japanese)
Nishioka, B., Watanabe, S., Fujita, Y., et al.: Evaluation of resection of stomach and adjacent organs for advanced gastric cancer in special reference to splenectomy and pancreatico-splenectomy. Jpn. J. Gastroenterol. Surg. 12:955, 1979 (in Japanese)
Takahashi, M.: Effect of splenectomy in the operation for gastric cancer on the immunological status. Gan No Rinsyo, 25:1059, 1979 (in Japanese)
Toge, T., Seto, Y., Yanagawa, E., Hattori, T.: Effect of splenectomy on the prognosis in gastric cancer patients. Syokakigeka 9:1887, 1989 (in Japanese)
Miwa, H., Orita, K.: Splenectomy for cancer therapy. Rinsyo To Kenkyu 60:2913, 1983 (in Japanese)
Miyashita, K., Muto, K., Sasaki, K., Tanaka, O., Nashimono, A., Yoshikawa, H.: Significance of lymph node dissection at the splenic hilus along the splenic artery. Rinsyo Geka 39:1535, 1984 (in Japanese)
Maruyama, K., Kitaoka, H., Hirata, K., Okabayashi, K., Kikuchi, S.: Is combined resection necessary for no. 10 and no. 11 lymph node dissection in radical gastrectomy? Syokakigeka 7:1509, 1984 (in Japanese)
Saji, S., Kunieda, K.: Evaluation of splenectomy on the prognosis of gastric cancer patients, with special reference to effects of post-operative immunochemotherapy. Syokakigan 165:1991 (in Japanese)
Takagi, H., Okuno, K., Nakamura, T., Kokudo, S., Iwasa, Z., Yasutomi, M.: Induction of tumoricidal effectors from the tumor-bearer's splenocytes and the prospects of their utilization for the adoptive immunotherapy. J. Jpn. Soc. Cancer Ther. 21:721, 1986 (in Japanese)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Okajima, K., Isozaki, H. Splenectomy for treatment of gastric cancer: Japanese experience. World J. Surg. 19, 537–540 (1995). https://doi.org/10.1007/BF00294715
Issue Date:
DOI: https://doi.org/10.1007/BF00294715