Abstract
Objectives
The purpose of this study was to determine whether a mid-infrared laser can induce selective fibrinolysis and to analyze the effect of altered fibrin structure (thin vs. thick fibers) on laser-clot interaction.
Background
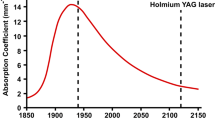
Mechanical disruption of thrombus can be achieved with balloon angioplasty, sonication, and thermal energy. Thrombi avidly absorb light in the mid-infrared optical spectrum due to their high water content. This phenomenon provides a potential for mid-infrared lasers as a source for selective thrombolysis. As fibrin is the essential component of clot, a study of mid-infrared laser-fibrin interaction is warranted.
Methods
Clots of varying fibrin structure were lased in cuvettes with a solid-state, pulsed-wave, mid-infrared laser (2.1 micron, 500 mJ/pulse, 250 msec pulse length). Total pulse energies of 5 Joules (J), 10 J, 37.5 J, 75 J, and 112.5 J were tested. Protein content of the extruded fluid was measured by optical density absorbance at 280 nm. The amount of released material was studied as a function of lasing energy and clot structure. SDS-polyacrylamide gel electrophoresis was applied for analysis of protein bands in order to identify unique protein bands released by the selective effect of laser fibrinolysis.
Results
A threshold for mid-infrared laser induced fibrinolysis was found; application of up to 20 J of energy did not result in dissolution. As lasing energy was increased above 37.5 J, the structure of these gels was mechanically destroyed and 12.4 ± 6.7% (mean ± SEM) of the original content of protein was released. Electrophoresis revealed that lased gels did not release any unique protein band. Lased, thin fibers released significantly less protein than thick fibers, indicating that they are more resistant to the effect of this wavelength of energy.
Conclusions
Mid-infrared laser can induce in-vitro photoacoustic dissolution of fibrin clots. However, this wave-length laser achieves fibrinolysis by mechanical destruction of the target clot rather than by a selective effect, as induced by the pulsed-dye laser. A threshold exists for energy levels required. Thin fibrin fibers, with their high elastic modulus (i.e., gel rigidity) appear more resistant than thick fibers to the effect of lasing at this wavelength.
Similar content being viewed by others
References
Abela GS, Barbeau GR. Laser angioplasty: Potential effects and current limitations. In: Topol EJ, ed. Textbook of Interventional Cardiology, 1st ed. Philadelphia: W.B. Saunders, 1990:724–737.
Gregory KW. Laser thrombolysis. In: Topol EJ, ed. Textbook of Interventional Cardiology, 2nd ed. Philadelphia: W.B. Saunders, 1993;892–902.
Topaz O: Holmium laser coronary thrombolysis—a new treatment modality for revascularization in acute myocardial infarction: Review. J Clin Laser Med Surg 1992;10:427–431.
Topaz O, Rozenbaum E, Battista S, Peterson C, Wysham D. Laser facilitated angioplasty in acute myocardial infarction complicated by prolonged or recurrent chest pain. Cathet Cardiovasc Diagn 1993;28:7–16.
Topaz O. Holmium: YAG coronary angioplasty: The Multicenter Registry: In: Topol EJ, ed. Textbook of Interventional Cardiology, 2nd ed. Philadelphia: W.B. Saunders, 1993:867–891.
Carr ME, Gabriel DA. Dextran-induced changes in fibrin fiber size and density based on wavelength dependence of gel turbidity. Macromolecules 1980;13:1473–1477.
Carr ME, Hermans J. Size and density of very long fibers from turbidity—application to fibrin gels. Macromolecules 1978;11:46–50.
Carr ME, Gabriel DA. The effect of dextran 70 on the structure of plasma-derived fibrin gels. J Lab Clin Med 1980;96:985–993.
Topaz O. A new, safer lasing technique for laser-facilitated coronary angioplasty. J Intervent Cardiol 1993;6:297–306.
Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T. Nature 1970;227: 680–683.
LaMuraglia GM, Anderson RR, Parrish JA, Zhana D, Prince MR. Selective laser ablation of venous thrombus: Implications for a new approach in the treatment of pulmonary embolus. Lasers Surg Med 1988;8:486–493.
Esenaliev RO, Oraevsky AA, Letokhov VS, Karabutov AA, Malinsky TV. Studies of acoustical and shock waves in the pulsed laser ablation of biotissue. Lasers Surg Med 1993;13:470–484.
Haase KK, Hanke H, Baumbach A, et al. Occurrence, extent and implications of pressure waves during excimer laser ablation of normal arterial wall and atherosclerotic plaque. Lasers Surg Med 1993;13:263–270.
Lee G, Ikeda RM, Strobbe D. Effect of laser irradiation on human thrombus: Demonstration of a linear dissolution-dose relation between clot length and energy density. Am J Cardiol 1983;52:876–877.
Gabriel DA, Muga K, Boothroyd EM. The effect of fibrin structure on fibrinolysis. J Biol Chem 1992;267:259–263.
Collet J, Soria J, Mirshahi M, et al. Dusart syndrome: A new concept of the relationship between fibrin clot architecture and fibrin clot degradability: Hypofibrinolysis related to an abnormal clot structure. Blood 1993;82:2462–2469.
Mirshahi M, Soria J, Soria O, Bertrand M, Besdevant A. Glycosylation of human fibrinogen and fibrin in vitro its consequences on the properties of fibrin(ogen). Thromb Res 1987;48:279–289.
Gabriel DA, Smith LA, Folds JD, Davis L, Canelosi SE. The influence of immunoglobin (IgG) on the assembly of fibrin gels. J Lab Clin Med 1983;101:545–552.
Carr ME, Powers PL, Jones MR. Effects of poloxamer 1988 on the assembly, structure and dissolution of fibrin clots. Thromb Haemostas 1991;66:565–568.
Geiger M, Binder BR. Nonenzymatic glucosylation as a contributing factor to defective fibrinolysis in diabetes mellitus. Haemostasis 1986;16:439–446.
Carr ME, Hardin CL. Large fibrin fibers enhance urokinase-induced plasmin digestion of plasma clots. Blood 1987;70:400a.
Nair CH, Azhar A, Wilson JD, Dhall DP. Studies on fibrin network structure in human plasma, part II-clinical application: Diabetes and antidiabetic drugs. Thromb Res 1991;64: 477–485.
Carr ME, Zekert SL. Abnormal clot retraction, altered fibrin structure, and normal platelet function in multiple myeloma. Am J Physiol 1994;266:H1195-H1201.
Craddock CG, Adams WS, Figueroa WG. Interference with fibrin formation in multiple myeloma by an unusual protein found in blood and urine. J Lab Clin Med 1953;42:847–859.
Davies MJ, Thomas AC. Plaque fissuring: The case of myocardial infarction, sudden ischemic death and crescendo angina. Br Heart J 1985;53:363–373.
Schroder R, Neuhaus KL, Leizorovicz A, Linderer T, Tebbe U, for the ISAM Study Group. A prospective placebo-controlled double-blind multicenter trial of intravenous streptokinase in acute myocardial infarction (ISAM): Long term mortality and morbidity. J Am Coll Cardiol 1987;9:197–203.
O'Neill WW, Brodie BR, Ivanhoe R, et al. Primary coronary angioplasty for acute myocardial infarction. Am J Cardiol 1994;73:627–634.
Topaz O, Minisi AJ, Luxenberg M, Rozenbaum E. Laser angioplasty for lesions unsuitable for PTCA in acute myocardial infarction: Quantitative coronary angiography and clinical results. Circulation 1994;90(Suppl I):I434.
Dehmer GJ, Gresalfi N, Daly D, Oberhardt B, Tate DA. Impairment of fibrinolysis by streptokinase, urokinase and recombinant tissue-type plasminogen activator in the presence of radiographic agents. J Am Coll Cardiol 1995;25: 1069–1075.
Author information
Authors and Affiliations
Additional information
This work was supported in part by a research grant from Boston Scientific, Boston, MA.
Rights and permissions
About this article
Cite this article
Topaz, O., Minisi, A.J., Morris, C. et al. Photoacoustic fibrinolysis: Pulsed-wave, mid-infrared laser-clot interaction. J Thromb Thrombol 3, 209–214 (1996). https://doi.org/10.1007/BF00181663
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00181663