Summary
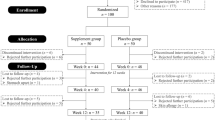
The long-term vitamin requirements of men (n=22) with moderate hyperhomocysteinemia (plasma total homocysteine concentration > 16.3 μmol/1) were investigated over a period of 48 weeks. An initial 6-week period of vitamin supplementation (1.0 mg folic acid, 10 mg pyridoxine, 0.05 mg cyanocobalamin) reduced plasma homocysteine levels 54.7% (P<0.001). However, 18 weeks after vitamin therapy was discontinued, only seven participants (subgroup A) still had plasma homocysteine levels of 16.3 μmol/l or lower. The remainder of the participants (subgroup B) required a second 6-week period of vitamin therapy to normalize the elevated plasma homocysteine levels. Substitution of vitamin supplementation by dietary guidelines to increase folate intake from food products failed to maintain normal plasma homocysteine levels in participants from subgroup B. Long-term vitamin supplementation may be required in some individuals to prevent hyperhomo-cysteinemia.
Similar content being viewed by others
Abbreviations
- HPLC:
-
high-performance liquid chromatography
- Lp(a):
-
lipoprotein(a)
- PLP:
-
pyridoxal 5′-phosphate
References
Allen RH, Stabler SP, Savage DG, Lindenbaum J (1990) Diagnosis of cobalamin deficiency 1: usefulness of serum methylmalonic acid and total homocysteine concentrations. Am J Hematol 34:90–98
Araki A, Sako Y (1987) Determination of free and total homocysteine in human plasma by HPLC with fluorescence detection. J Chromatogr 422:43–52
Brattström LE, Hardebo JE, Hultberg BL (1984) Moderate homocysteinemia — a possible risk factor for arteriosclerotic cerebrovascular disease. Stroke 15:1012–1016
Brattström LE, Israelsson B, Jeppson JO, Hultberg BL (1988) Folic acid — an innocuous means to reduce plasma homocysteine. Scand J Clin Lab Invest 48:215–221
Brattström L, Israelsson B, Norrving B, Bergqvist D, Thorne J, Hultberg B, Hamfelt A (1990) Impaired homocysteine metabolism in early — onset cerebral and peripheral occlusive arterial disease. Atherosclerosis 8:51–60
Christensen B, Refsum H, Vintermyr O, Ueland PM (1991) Homocysteine export from cells cultured in the presence of physiological or superfluous levels of methionine: methionine loading of non-transformed, transformed, proliferating, and quiescent cells in culture. J Cell Physiol 146:52–62
Coull BM, Malinow MR, Beamer N, Sexton G, Nordt F, De Garmo P (1990) Elevated plasma homocyst(e)ine concentration as a possible independent risk factor for stroke. Stroke 21:572–576
Food and Nutrition Board, National Academy of Sciences (USA) Recommended Dietary Allowances, 1989. National Academy Press, Washington DC
Genest JJ, McNamara DN, Salem JR, Wilson PWF, Scaefer EJ, Malinow MR (1990) Plasma homocyst(e)ine levels in men with premature coronary artery disease. J Am Coll Cardiol 16:1114–1119
Gouws E, Langehoven ML (1986) NRIND food composition tables, 2nd edn. National Research Institute for Nutritional Diseases, South African Medical Research Council, Parow, South Africa
Harker LA, Ross R, Slichter SJ, Scott CR (1976) Homocystine-induced arteriosclerosis. The role of endothelial cell injury and platelet response in its genesis. J Clin Invest 58:731–741
Harpel PC, Chang VT, Borth W (1992) Homocysteine and other sulfhydryl compounds enhance the binding of lipoprotein(a) to fibrin: a potential biochemical link between thrombosis, atherogenesis, and sulfhydryl compound metabolism. Proc Natl Acad Sci USA 89:10193–10197
Israelsson B, Brattstrom LE, Hultberg BL (1988) Homocysteine and myocardial infarction. Atherosclerosis 71:227–233
Kang SS, Wong PWK, Susmano A, Sora J, Norusis M, Ruggie N (1991) Thermolabile methylenetetrahydrofolate reductase: an inherited risk factor for coronary artery disease. Am J Hum Genet 48:536–545
Malinow MR, Kang SS, Taylor LM, Wong PWK, Coull B, Inahara T, Mukerjee D, Sexton G, Upson B (1989) Prevalence of hyperhomocyst(e)inemia in patients with peripheral arterial occlusive disease. Circulation 79:1180–1188
Mudd SH, Levy HL, Skovby F (1989) Disorders of transsulfuration. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic basis of inherited disease. McGrawHill, New York, pp 693–734
Parthasarathy S (1987) Oxidation of low-density lipoprotein by thiol compounds leads to its recognition by the acetyl LDL receptor. Biochim Biophys Acta 917:337–340
Stampfer MJ, Malinow R, Willet WC, Newcomer LM, Upson B, Ullmann D, Tishler PV, Hennekens CH (1992) A prospective study of plasma homocyst(e)ine and risk of myocardial infarction in US physicians. JAMA 268:877–881
Starkebaum G, Harlan JM (1986) Endothelial cell injury due to copper-catalyzed hydrogen peroxide generation from homocysteine. J Clin Invest 77:1370–1376
Stipanuk MH (1986) Metabolism of sulfur-containing amino acids. Anna Rev Nutr 6:179–209
Svardal AM, Djurhuus R, Refsum H, Ueland PM (1986) Disposition of homocysteine in rat hepatocytes and in non-transformed and malignant mouse embryo fibroblasts following exposure to inhibitors of s-adenosylhomocysteine catabolism. Cancer Res 46:5095–5100
Taylor LM, DeFrang RD, Harris EJ, Porter JM (1991) The association of elevated plasma homocyst(e)ine with progression of symptomatic peripheral arterial disease. J Vasc Surg 13:128–136
Ubbink JB, Serfontein WJ, De Villiers LS (1985) Stability of pyridoxal-5-phosphate semicarbazone: application in plasma vitamin B6 analysis and population surveys of vitamin B6 nutritional status. J Chromatogr 342:277–284
Ubbink JB, Vermaak WJH, Bennett JM, Becker PJ, Van Staden DA, Bissbort S (1991) The prevalence of homocysteinemia and hypercholesterolemia in angiographically defined coronary heart disease. Klin Wochenschr 69:527–534
Ubbink JB, Vermaak WJH, Bissbort S (1991) Rapid high-performance liquid chromatographic assay for total homocysteine levels in human serum. J Chromatogr 565:441–446
Ubbink JB, Vermaak WJH, Van der Merwe A, Becker BPJ (1993) Vitamin B12, vitamin B6 and folate nutritional status in men with hyperhomocysteinemia. Am J Clin Nutr 57:47–53
Ueland PM, Refsum H, Brattström L (1992) Plasma homocysteine and cardiovascular disease. In: Francis BR (ed) Atherosclerotic cardiovascular disease, hemostatis, and endothelial function. Dekker, New York, pp 183–235
Wilcken DEL, Gupta VJ, Betts AK (1981) Homocysteine in the plasma of renal transplant recipients: effects of cofactors for methionine metabolism. Clin Sci 61:743–749
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ubbink, J.B., van der Merwe, A., Vermaak, W.J.H. et al. Hyperhomocysteinemia and the response to vitamin supplementation. Clin Investig 71, 993–998 (1993). https://doi.org/10.1007/BF00180030
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/BF00180030