Abstract
Today, hospitals are facing difficult challenges: increasing proportion of immunologically vulnerable patients often affected by diseases requiring high complex level of healthcare; rapidly evolving medical technologies and healthcare models; and budget restrictions. All these features interfere with healthcare and can modify the risk of acquiring healthcare-associated infections (HCAIs). Therefore, HCAI prevention is a high priority for healthcare systems. Authors describe human and environmental origin of HCAIs, focusing on the modality of transmission of those airborne pathogens, including the new insight derived from the recent acquisitions about SARS and Ebola epidemiology. They also describe the state of the art about microorganism concentration (infective dose) required to determine a HCAI and the role played by other virulence factors. Finally, the effective control measures used for the prevention of airborne pathogen transmission are described, focusing mainly on the risk assessment and infection control.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
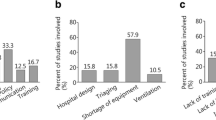
Hospitals are confronted today with difficult challenges, represented by the increasing proportion of immunologically vulnerable patients often affected by diseases requiring high complex levels of healthcare (Capolongo et al. 2014); the rapidly evolving medical technologies and healthcare models; and the budget restrictions (Astley et al. 2015; Zantedeschi et al. 2003; Capolongo et al. 2016). All these features interfere with healthcare and can modify the risk to acquire healthcare-associated infections (HCAIs). Therefore, HCAI prevention is a high priority for all healthcare systems (WHO 2011).
Many studies show that hospital built environment influences the risk of acquiring HCAIs (Sehulster and Chinn 2003; Capolongo 2016), although, at present, its quantitative impact is not yet known (WHO 2011); some studies show that a careful consideration of environmental transmission routes in the design and operation of healthcare facilities can significantly reduce the burden of HCAIs (Sehulster and Chinn 2003; Seigel et al. 2007; D’Alessandro and Capolongo 2009; Bartley and Streifel 2010).
Several environmental HCAI agents do not usually involve person-to-person transmission. For example, spores of environmental fungi and bacteria (e.g., Aspergillus spp. and Legionella spp.) may cause disease, mainly in immunocompromised subjects, who inhale aerosolized microorganisms coming from construction dust, or moisture and dust accumulated within heating, ventilation, and air-conditioning (HVAC) systems, or water aerosolized from distribution systems, etc. (Seigel et al. 2007; Kumari et al. 1998; D’Alessandro et al. 2015).
Several factors make hospitals suitable for microbial environmental colonization, increasing the HCAI risk; for example,
-
1.
the abuse of antimicrobials induces the formation of a large reservoir of resistant microbial strains (WHO 2011);
-
2.
the infrastructure repairs and the renovation of aging hospitals cause the release of dust-containing fungal spores during construction and, in particular, demolition activities (D’Alessandro and Capolongo 2009; Baglioni and Capolongo 2002);
-
3.
the simultaneous presence and interaction of different types of subjects, such as patients, healthcare workers, and visitors, often in the absence of behavioral rules;
-
4.
the lack of financial support for maintenance and adequate sanitization (WHO 2011);
-
5.
the inadequate training of personnel in the field of HCAI control (D’Alessandro et al. 2014).
This paper examines in particular how HCAI agents spread among hospitalized patients via environmental routes, focusing on the mechanisms of airborne transmission and the ways the design, construction, renovation, and maintenance of the hospital play a critical role in preventing—or favoring—the environmental contamination and the spread of infections.
Microorganisms in Hospital Indoor Environments: Where Do They Come from?
Airborne pathogens, involved in HCAIs, may have (a) a human or (b) environmental origin. Therefore, they can enter the air by a variety of routes.
Most airborne microorganisms within the building are of human origin: staff, patients, and visitors. Generally, the higher the bed occupancy level, the greater the microbial bioburden in the air (Beggs 2003). Humans spread infectious particles of respiratory secretions by coughing, sneezing, or talking. On average, a cough can generate some 3,000 droplet nuclei, and the same can do speaking for 5 min; sneeze can generate as many as 40,000 droplet nuclei. Droplet nuclei are large particles that settle out from the air, but once evaporated into particles in the 0.5–12 μm range (Cole and Cook 1998), they can be resuspended in the indoor air. Other aerosol-generating activities are represented by making a bed: In that case, skin scales shed by patients infected with methicillin-resistant Staphylococcus aureus represent a reservoir for airborne infections (Ulrich et al. 2008).
As far as the environmental origin of airborne pathogens, a problem until now underestimated is the “microbial ecology” of hospital building. Actually, their potential effects on human health can be minimized through proper design, construction, operation, maintenance, and cleaning. In particular, the extent and persistence of moisture in various structural, finishing, and furnishing materials is a problem of greatest importance (Cole and Cook 1998; D’Alessandro and Capolongo 2009). If relative humidity is uncontrolled or if leaks, floods, or sewage backups are not readily and properly repaired, the result is an altered microbial ecology that permits the amplification (overgrowth) and dissemination of fungal and bacterial species with the potential for opportunistic nosocomial infections (Cole and Cook 1998; Vonberg and Gastmeier 2006). Microorganisms grow in moisture films on several surfaces and within porous materials. The amount of free water available to them for growth on a substrate or microenvironment (e.g., ceiling tile) is described as water activity (aw), the ratio of the vapor pressure of water in the substrate to the vapor pressure of free water. Increased aw due to high relative humidity, leaks, or floods, if allowed to persist more than 24 h, changes the normal ecology of a microenvironment or of the entire building, with microbial competition resulting in the predominance of one or more organisms with potentially damaging effects upon materials and health. Fungi require the lowest aw level to grow. Most fungi have a minimum requirement of aw of at least 0.88%, but some fungi have even lower limits, down to 0.66–0.70% (Cole and Cook 1998; D’Alessandro et al. 2016).
Other, more occasional cases or outbreaks of environmental airborne HCAI are due to exhaust ducting of the ventilation systems, cooling towers, aerosol produced by faucets, shower heads, humidifiers, nebulizers, etc. (Sehulster and Chinn 2003; Kumari et al. 1998; D’Alessandro et al. 2015). Furthermore, outdoor and indoor construction, ceiling tile, and contaminated carpets have been involved in outbreaks due to fungal spores (D’Alessandro and Capolongo 2009; Sehulster and Chinn 2003).
How Can Microorganisms Be Transmitted Through the Air?
Establishing how microorganisms are transmitted under different circumstances, and whether transmission requires close contact, is of great importance as such information affects the choice of infection control measures in healthcare settings.
The main routes of HCAI transmission are contact, droplet, and airborne.
Contact modality includes all the infections where the victim is in direct (person-to-person) or indirect (person–inanimate object–person) contact with the source of infection (Beggs 2003; Seigel et al. 2007).
Droplet transmission is, technically speaking, a kind of contact transmission, and some infectious agents transmitted by the droplet route are the same which are transmitted by the direct contact route (Seigel et al. 2007). However, in contrast with the traditional contact transmission, respiratory droplets carrying infectious pathogens transmit infection when they travel directly from the respiratory tract of the infectious individual to susceptible mucosal surfaces of the recipient, generally over short distances. Respiratory droplets are generated when an infected person coughs, sneezes, or talks or during procedures such as suctioning, endotracheal intubation, cough induction by chest physiotherapy, and cardiopulmonary resuscitation (Seigel et al. 2007).
The maximum distance for droplet transmission is an unresolved issue, even if the pathogens transmitted by droplet route have not been transmitted through the air over long distances (Sehulster and Chinn 2003, Seigel et al. 2007; Jones and Brosseau 2015). The literature suggested that area of defined risk has been a distance of <3 feet around the patient (Sehulster and Chinn 2003; Seigel et al. 2007; Jones and Brosseau 2015), although other studies on smallpox (Fenner et al. 1988) and SARS (Wong et al. 2004) indicate that droplets from patients could reach persons located 6 feet or more from their source, depending on the velocity and mechanism by which respiratory droplets are propelled from the source, the density of respiratory secretions, environmental factors such as temperature and humidity, and the ability of the pathogen to maintain infectivity over that distance (Cole and Cook 1998).
Droplet size is another variable under discussion (Seigel et al. 2007; Jones and Brosseau 2015). Droplets traditionally have been defined as being >5 μm in size. Droplet nuclei, particles arising from drying of suspended droplets, have been associated with airborne transmission and defined as ≤5 μm in size (Seigel et al. 2007). These values arose from a study (Wells 1955) regarding pulmonary tuberculosis transmission, which is not exactly applicable to other organisms; at that time, sampling methods were unable to measure particles suspended in air around the infectious source. Observations of particle dynamics have demonstrated that a range of droplet sizes, including those with diameters of 30 μm or greater, can remain suspended in the air (Cole and Cook 1998). In general, whereas fine airborne particles containing pathogens that are able to remain infective may transmit infections over long distances, organisms transmitted by the droplet route do not remain infective over long distances and therefore do not require special air handling and ventilation (Seigel et al. 2007).
Airborne transmission (AT) is a type of indirect contact, and it refers to infections which are contracted from microorganisms which have become airborne, namely particles that are transported by convective air currents (Beggs 2003). AT generally applies to microorganisms contained in droplet nuclei produced by coughing, sneezing, or some other form of aerosolization, but it also applies to dust particles of environmental origin or skin scales, carrying pathogenic microorganisms and fungal spores, also widely disseminated via the airborne route (Beggs 2003). Overall, this route of transmission accounts for 10–20% of endemic HCAIs (Beggs 2003). Microorganisms carried in this manner may be dispersed over long distances by air currents and may be inhaled by susceptible individuals who have not had face-to-face contact with (or been in the same room with) the infectious individual (Seigel et al. 2007). The prevention of the spread of airborne transmitted pathogens (e.g., Mycobacterium tuberculosis, measles (rubeola) virus, and varicella zoster virus) requires the use of special air-handling and ventilation systems to contain and then safely remove the infectious agent and also a specific respiratory protection.
After the emergence of SARS in 2002 and other subsequent outbreaks (e.g., avian influenza), the literature showed conflicting information about possible route of transmission. For certain respiratory infectious agents (e.g., influenza and rhinovirus and SARS-CoV) and some gastrointestinal viruses (e.g., norovirus and rotavirus), the pathogen may be transmitted via small-particle aerosols, in addition to the primary droplet and contact routes. In the case of gastrointestinal viral infections, it is hypothesized that the aerosolized particles from vomitus or fecal material are inhaled and subsequently swallowed (Seigel et al. 2007). Such transmission has occurred over distances longer than 3 feet but within a defined airspace (e.g., patient room), suggesting that it is unlikely that these agents remain viable on air currents that travel long distances. Small-particle aerosol, however, is not defined relative to the three conventional transmission routes (Cole and Cook 1998).
Therefore, a new classification for aerosol transmission was proposed by Roy and Milton (2004) to evaluate the routes of SARS transmission. It includes the following:
-
1.
Obligate: Under natural conditions, disease occurs following transmission of the agent only through inhalation of small-particle aerosols (e.g., tuberculosis);
-
2.
Preferential: Natural infection results from transmission through multiple routes, but small-particle aerosols are the predominant route (e.g., measles and varicella); and
-
3.
Opportunistic: Agents that naturally cause disease through other routes, but under special circumstances may be transmitted via fine particle aerosols.
This conceptual framework can explain rare occurrences of airborne transmission of agents that are transmitted most frequently by other routes (e.g., smallpox, SARS, influenza, and noroviruses). Concerns about unknown routes of transmission of agents associated with severe disease often result in more extreme prevention strategies than may be necessary; therefore, recommended precautions could change as the epidemiology of an emerging infection is defined and controversial issues are resolved.
Recently, after the 2013 Ebola Virus Disease (EVD) outbreak, other authors introduced the concept of aerosol transmission (Jones and Brosseau 2015) to better define the route for small-particle aerosol and to move from the artificially dichotomized airborne and droplet transmission routes toward a more physically appropriate representation of the exposure and infection process. An aerosol is a collection of solid or liquid particles suspended in a gas, such as air, that may contain particles of any size. The fate of an aerosol in the environment is governed by physical processes (gravitational force, air movement, etc.). In the context of infectious disease transmission, many processes and procedures generate aerosols that may contain both body fluid particles and pathogens. Infectious aerosols are subject to the same transport processes of other aerosols. The range of particle sizes included depends on several factors such as the mechanism of aerosol generation, the viscosity of the aerosolized fluid, and its liquid content. The liquid content influences the extent to which the particle size reduces with evaporation. From the authors’ perspective, the concept of aerosol transmission is of primary importance to occupational health and it should trigger consideration for controls, such as respiratory protection, that limit workers’ exposures when in the proximity of infectious patients, regardless of evidence for airborne transmission (Jones and Brosseau 2015).
The assessment of airborne infectious entities requires investigation not only into their generation, their particle sizes, and their aerodynamic properties, but also into their concentrations, their infectivity and virulence, and their viability with respect to climate factors (temperature and relative humidity) (Cole and Cook 1998).
Obviously, the survival of bioaerosols is a key factor and depends on their suspending medium, temperature, relative humidity, oxygen sensitivity, and exposure to UV or electromagnetic radiations. Once aerosolized in the indoor environment, microorganisms are subject to lethal desiccation, which results from an interplay of organism morphology, physiology, oxygen sensitivity, and suspending medium, with varying levels of relative humidity and temperature, in addition to air movements, pressure fluctuations, air ions, and other airborne pollutants (Cole and Cook 1998). Thus, the survival potential of any given microbial pathogen when aerosolized is unique to that organism under those specific conditions at that particular point in time.
The variability of impact of climatic conditions on the survival of different microorganisms makes the role of the environment extremely complex, and the knowledge in this field needs to be further developed.
Infective Doses and Implication for Building Ventilation
As known, the infectious disease depends on the microorganism concentration (infective dose) and its virulence that enable the agent to overcome the normal defenses of the host. Some microbial diseases require only small infective doses because the agents have affinity for specific tissue and possess one or more potent virulence factors that make them resistant to inactivation (e.g., F. tularensis, M. tuberculosis, measles, and influenza viruses) (Cole and Cook 1998).
Since the number of microorganisms required is frequently unknown, to model the transmission of respiratory pathogens, such as TB or measles, that spread more easily in a crowd rather than by close contact, Wells–Riley in late 1970s (Riley et al. 1978) proposed an equation and used the term “quanta” (q) as “the number of infectious airborne particles required to infect which may be one or more airborne particles.” The Wells–Riley equation has several important limitations: it assumes that the air in the space is fully mixed and does not account for heterogeneity in infectiousness or susceptibility to infection (Yates et al. 2016). Subsequently, adaptations of the equation have been published. One popular variant uses a rebreathed fraction, the fraction of inhaled air that has been exhaled previously by someone in the building (Nardell 2016). This rebreathed fraction can be obtained from paired indoor and outdoor carbon dioxide measurements. This process avoids the need to measure Q, which can be technically challenging. It is an indirect way to evaluate the exposure level.
However, patients vary greatly in infectiousness. For example, for tuberculosis, this variability is related to the characteristics of the source patient (e.g., frequency of cough, viscosity of respiratory secretions, and presence of lung cavities or laryngeal disease), the strain virulence, the vulnerability of exposed hosts, and environmental factors, but they are difficult to separate. The same source patient and strain will infect more contacts in a crowded, poorly ventilated environment with highly susceptible hosts (Nardell 2016).
Building occupancy correlates with risk for at least two synergistic reasons: the greater the number of those present in the room (or building), rebreathing each others’ air, the greater the risk of presence of an infectious source or sources in that population and the greater the number of exposed occupants (Nardell 2016).
Airborne fungi, most notably A. fumigatus and other species, pose an extremely serious infectious disease threat to those who are immunocompromised as a result of immunosuppressive or cytotoxic therapy (D’Alessandro and Capolongo 2009). Hospital outbreaks of pulmonary aspergillosis have occurred mainly among patients with granulocytopenia, especially in bone marrow-transplant units. For these high risk patients, it has been estimated that even concentrations of Aspergillus spp below 1 colony-forming unit/m3 were sufficient to cause infection (Vonberg and Gastmeier 2006).
Control of Airborne Transmission of Pathogens
In order to apply the appropriate control measures and to avoid unnecessary costs, to control airborne transmission of pathogens, it is necessary to identify the areas where the risk of airborne infection is the greatest. This can be done through a process called infection control risk assessment (ICRA) and its subsequent revisions (FGI 2014); it is a multidisciplinary, organizational, documented proactive process designed to enable the organizations to anticipate the potential impact (D’Alessandro and Capolongo 2009). In summary, ICRA identifies groups of patients at risk and areas where infection control is necessary in order to define the appropriate measures for infection control and maintenance programs.
In particular, the hospital patients interested by the risks associated with airborne infection can be divided into two groups: (a) infectious patients, who may spread infectious agents such as tuberculosis, varicella, and rubella, and (b) susceptible patients (e.g., bone marrow- and solid organ-transplant recipients, those undergoing cancer treatment, babies born prematurely, AIDS patients, and patients whose immunity is compromised by interventions such as surgery), who are vulnerable to such agents but also to common opportunistic infectious agents.
The areas in which airborne infection control is necessary include (a) airborne infection isolation rooms, where airborne infectious agents could be contained (e.g., convalescence rooms, emergency rooms, examination rooms, intensive care units, radiology and diagnostic rooms, and procedure rooms), and (b) protective environments, such as operating and bone marrow-transplant rooms, which must be free of airborne infectious agents.
Pressure control via an offset between supply and exhaust air volumes is essential to prevent the migration of unwanted airborne contaminants into critical areas. Over supplying a protective environment, it provides an airflow from clean to less clean direction.
Isolating a patient in a room with controlled airflow is another strategy to prevent the airborne spread of infection. The 2003 CDC guidelines address controlling airflow from unclean to clean through the use of pressurization and anterooms (Sehulster and Chinn 2003). Positive pressure rooms prevent the outside air from getting into the room and are useful for keeping potentially contaminated air away from immunocompromised patients, including those with neutropenia following chemotherapy.
Patients with highly transmittable airborne pathogens should be placed, on the contrary, in a negative pressure isolation room, which can prevent the transmission of pathogens such as Mycobacterium tuberculosis, varicella (chicken pox), and rubeola (measles) (Sehulster and Chinn 2003). These negative pressure isolation rooms are typically single-patient rooms.
Positive pressure ventilation is used to protect the vulnerable patients. While the needed number of rooms with special ventilation depends to some degree on the patient population served by the hospital, single-patient rooms with negative pressure ventilation should be added to all existing and new constructions (Bartley and Streifel 2010).
Actually, single-patient rooms and flexible acuity rooms are the trend in hospital planning and design (Bartley and Streifel 2010). In addition to the reduction in the risk of cross-infection, the reported advantages of single-occupancy rooms included also improvements in patient care and greater flexibility in operation. However, it is important to view and interpret the benefits of single rooms within the context of patient care issues, other environmental changes, and management policy changes to bring about desired and sustainable outcomes.
Other suggested measures to interrupt the airborne transmission of pathogens (Jacob et al. 2013) include the control of the flow and quality of air to minimize the exposure to airborne pathogens and the use of filters to trap particles, including pathogens, and to remove them from circulation.
Specific indications on most of indoor air quality requirements are reported in the 2003 CDC guidelines (Sehulster and Chinn 2003). HVAC systems are the primary mechanism for controlling air in the hospital environment; their goals are to replace potentially contaminated air with clean air, to minimize the mixing of dirty and clean air, and to regulate ambient temperature and humidity. In addition, filtration of ventilated air can reduce the number of airborne pathogens. Air filters are rated based on the size of particles they are able to remove, and high-efficiency particulate air (HEPA) filters are widely used in healthcare settings, having an efficiency of at least 99.97% at a test aerosol diameter of 0.3 µm (Sehulster and Chinn 2003). HEPA filters remove airborne pathogens in critical areas such as operating rooms, transplant units, isolation rooms, and intensive care units. Filtration is a strategy that utilizes several levels of filters, the highest of which is HEPA filter. The use of HEPA filters is widespread in hospitals, especially in areas that house immunocompromised patients. Another issue related to HVAC systems is the appropriate type of airflow direction to recommend for protective environment. Multiple technologies are currently available to control the direction of airflow inside the hospital, although no consensus exists whether turbulent, displacement, or unidirectional airflow is the most effective (Jacob et al. 2013). Traditional ventilation systems in patient care areas utilize turbulent air to direct airflow rapidly away from patients. also called unidirectional airflow), used most commonly in operating room, is a method of air ventilation in which ultraclean air that has passed through a HEPA filter is distributed either vertically or horizontally in a smooth stream directed over the patient. Although unidirectional airflows seem to be the gold standard, the evidence supporting their use in operating rooms and other protective environments is not enough, because their impact on infection rates remains unresolved (Jacob et al. 2013; Agodi et al. 2015); therefore, further investigations are required.
Effective Air Quality Control Measures During Construction and Renovation
Finally, it is extremely important to employ effective control and prevention measures during construction and renovation, because such activities have been frequently implicated in outbreaks of airborne infection. The ICRA approach, described above, can help to classify the risk level of each yard and to define the appropriate control measures for air quality (D’Alessandro and Capolongo 2009). Examples of such measures include using portable HEPA filters, installing barriers between patient care areas and construction/renovation areas, generating negative air pressure for construction/renovation areas relative to patient care areas, and sealing patients’ room windows (D’Alessandro and Capolongo 2009; Ulrich et al. 2008). The application of accurate cleaning protocols to reduce environmental dust is also required (D’Alessandro and Capolongo 2009).
Conclusions
After the outbreaks of SARS in 2002–2003, the concerns about an expected avian influenza (H5N1) pandemic and the recent outbreak of Ebola virus disease, the airborne infections have attracted more attention, following a long period in which their role may have been underestimated, due to the difficulty of culturing many airborne organisms and the complexities of assessing the role played by such pathogens in the contamination of environmental surfaces and subsequent contact transmission (Ulrich et al. 2008; Beggs 2003).
Although spread by contact is an important and well-known environmental mechanism of infections, this paper has been intentionally focused on HCAI of airborne origin. Therefore, some design aspects of interest in the prevention of HCAI (e.g., handwashing station design and placement, surfaces and furnishing features) have not been described.
Despite these intentional choices, some conclusions can be of general interest. One is that in order to prevent HCAIs, two kinds of expertise are necessary, namely knowledge of traditional infection control and knowledge of human behaviors, to help healthcare workers employ infection control science effectively (Hamilton and Stichler 2013). Actually, the effectiveness of preventive measures is related to the availability of appropriate periodic maintenance programs to assure the safe ventilation of indoor air, but also the strict compliance with the procedures by the staff (D’Alessandro et al. 2014; Agodi et al. 2015).
Therefore, it is of paramount importance to increase the healthcare workers’ awareness of the risks associated with incorrect behaviors and to improve their training, because, independently from the technology available, the human behavior is crucial to ensure the indoor air quality and safety in healthcare setting (Pitzurra et al. 1997; D’Alessandro et al. 2014; Agodi et al. 2015).
References
Agodi A, Auxilia F, Barchitta M, Cristina ML, D’Alessandro D, Mura I, et al. Operating theatre ventilation system and microbial air contamination in total joint replacement surgery: results of the GISIO-ISChIA study. J Hosp Infect. 2015;90:2013–9. doi:10.1016/j.jhin.2015.02.014.
Astley P, Capolongo S, Gola M, Tartaglia A. Operative and design adaptability in healthcare facilities. Technè. 2015;9:162–70. doi:10.13128/Techne-16118.
Baglioni A, Capolongo S. Ergonomics in planning and reconstruction. G Ital Med Lav Ergon. 2002;24(4):405–9.
Bartley J, Streifel AJ. Design of the environment of care for safety of patients and personnel: does form follow function or vice versa in the intensive care unit? Crit Care Med. 2010;38:S388–98. doi:10.1097/CCM.0b013e3181e6d0c1.
Beggs CB. The airborne transmission of infection in hospital buildings: fact or fiction? Indoor Build Environ. 2003;12:9–18.
Capolongo S. Social aspects and well-being for improving healing processes’ effectiveness. Ann Ist Super Sanità. 2016;52(1):11–4. doi:10.4415/ANN_16_01_05.
Capolongo S, Bellini E, Nachiero D, Rebecchi A, Buffoli M. Soft qualities in healthcare method and tools for soft qualities design in hospitals’ built environments. Ann Ig. 2014;26(4):391–9. doi:10.7416/ai.2014.1998.
Capolongo S, Gola M, di Noia M, Nickolova M, Nachiero D, Rebecchi A, et al. Social sustainability in healthcare facilities: a rating tool for analyzing and improving social aspects in environments of care. Ann Ist Super Sanità. 2016;52(1):15–23. doi:10.4415/ANN_16_01_06.
Cole EC, Cook CE. Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies. Am J Infect Control. 1998;26(4):453–64.
D’Alessandro D, Capolongo S. La gestione dei cantieri in ospedale: la proposta del GISIO. Ann Ig. 2009;21(suppl 1):131–8.
D’Alessandro D, Fabiani M, Cerquetani F, Orsi GB. Trend of Legionella colonization in hospital water supply. Ann Ig. 2015;27(2):460–6. doi:10.7416/ai.2015.2032.
D’Alessandro D, Tedesco P, Rebecchi A, Capolongo S. Water use and water saving in Italian hospitals. A preliminary investigation. Ann Ist Super Sanità 2016;52(1):56–62. doi:10.4415/ANN_16_01_11.
D’Alessandro D, Agodi A, Auxilia F, Brusaferro S, Calligaris L, Ferrante M, et al. Prevention of healthcare associated infections: medical and nursing students’ knowledge in Italy. Nurse Educ Today. 2014;34(2):191–5. doi:10.1016/j.nedt.2013.05.005.
Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID. The epidemiology of smallpox. In: Smallpox and its eradication. Switzerland: WHO; 1988.
FGI (Facility Guidelines Institute). Guidelines for design and construction of health care facilities. Chicago: American Society of Healthcare Engineering of the American Hospital Association; 2014. http://www.fgiguidelines.org.
Hamilton KD, Stichler J (eds). Understanding the role of facility design in the acquisition and prevention of healthcare-associated infections. HERD. 2013;7(suppl).
Jacob JT, Altug Kasali M, Steinberg JP, Zimring C, Denham ME. The role of the hospital environment in preventing healthcare-associated infections caused by pathogens transmitted through the air. HERD. 2013;7(suppl):74–98. doi:10.1177/193758671300701S07.
Jones RM, Brosseau LM. Aerosol transmission of infectious disease. J Occup Environ Med. 2015;57(5):501–8. doi:10.1097/JOM.0000000000000448.
Kumari DN, Haji TC, Keer V, Hawkey PM, Duncanson V, Flower E. Ventilation grilles as a potential source of methicillin-resistant Staphylococcus aureus causing an outbreak in an orthopaedic ward at a district general hospital. J Hosp Infect. 1998;39(2):127–33.
Nardell EA. Indoor environmental control of tuberculosis and other airborne infections. Indoor Air. 2016;26:79–87. doi:10.1111/ina.12232.
Pitzurra M, D’Alessandro D, Pasquarella C, Mura I, Cerquetani F, et al. Survey of air conditioners’ characteristics and management in same Italian operating theatres. Ann Ig. 1997;9:429–38.
Riley EC, Murphy G, Riley RL. Airborne spread of measles in a suburban elementary school. Am J Epidemiol. 1978;107:421–32.
Roy CJ, Milton DK. Airborne transmission of communicable infection—the elusive pathway. N Engl J Med. 2004;350(17):1710–2. doi:10.1056/NEJMp048051.
Sehulster L, Chinn RYW. Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the healthcare infection control practices advisory committee (HICPAC) MMWR 2003;52(RR10):1–42.
Siegel JD, Rhinehart E, Jackson M, Chiarello L, The Healthcare Infection Control Practices Advisory Committee. Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. 2007. http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf.
Ulrich RS, Zimring C, Zhu X, DuBose J, Seo H, et al. A review of the research literature on evidence-based healthcare design. HERD. 2008;3:61–125.
Vonberg RP, Gastmeier P. Nosocomial aspergillosis in outbreak settings. J Hosp Infect. 2006;63:246–54. doi:10.1016/j.jhin.2006.02.014.
Wells WF. Airborne contagion and air hygiene: an ecological study of droplet infections. Boston, MA: Harvard University Press; 1955.
WHO. Report on the Burden of Endemic Healthcare-Associated Infection Worldwide. Geneva, Switzerland: World Health Organization; 2011. http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf.
Wong TW, Lee CK, Tam W, Lau JT, Yu TS, Lui SF, et al. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerg Infect Dis. 2004;10(2):269–76. doi:10.3201/eid1002.030452.
Yates TA, Khan PY, Knight GM, Taylor JG, McHugh TD, Lipman M, et al. The transmission of Mycobacterium tuberculosis in high burden setting. Lancet Infect Dis. 2016;16:227–38. doi:10.1016/S1473-3099(15)00499-5.
Zantedeschi E, D’Alessandro D, Fara GM. Hospitals between present and future. Ann Ig. 2003;16:7–16.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 The Author(s)
About this chapter
Cite this chapter
D’Alessandro, D., Fara, G.M. (2017). Hospital Environments and Epidemiology of Healthcare-Associated Infections. In: Capolongo, S., Settimo, G., Gola, M. (eds) Indoor Air Quality in Healthcare Facilities. SpringerBriefs in Public Health. Springer, Cham. https://doi.org/10.1007/978-3-319-49160-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-49160-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-49159-2
Online ISBN: 978-3-319-49160-8
eBook Packages: MedicineMedicine (R0)