Abstract
This chapter is divided into four sections. The first section introduces the concept of person-centred care within pharmaceutical care delivery and provides a historical context. The second section focuses on the professionals and explores the role of person-centred pharmaceutical care as part of multi-disciplinary health services delivery teams. The third section focuses on the patient and describes the role of health literacy in the implementation of person-centred pharmaceutical care. The last section examines E-pharmacy services and the implementation of telepharmacy with implications for person-centred care.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Pharmaceutical care
- Person-centered care
- Pharmaceutical intervention
- Health professionals team
- Patient
- e-pharmacy
1 Introduction
Pharmaceutical care is a diverse concept. Over the last 50 years, many researchers and practitioners tried to define pharmaceutical care [1]. One of the first and widely cited is Hepler’s and Strand’s definition. It is cited, for example, in the recently adopted Resolution on the implementation of pharmaceutical care for the benefit of patients and health services [18], Resolution CM/Res 2020). According to that definition, pharmaceutical care is “the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life” and it “involves the process through which a pharmacist co-operates with a patient and other professional in designing, implementing and monitoring a therapeutic plan that will produce specific therapeutic outcomes for the patient” [18]. The pharmacists’ role in the pharmaceutical care provision has additionally been evaluated and described by Pharmaceutical Care Network Europe as “the pharmacist's contribution to the care of individuals in order to optimize medicines use and improve health outcomes” [1].
The main elements of pharmaceutical care involve the central role of the pharmacist and the patient-centered care approach, collaboration with carers, prescribers and other health care professionals (integrated care), prevention, detection and resolution of medication-related problems, and taking responsibility for optimising medication use in order to improve a patient’s health outcomes and quality of life (Resolution CM/Res 2020). In order to address noted elements, the following activities are purposed within the process of pharmaceutical care delivery: (i) assessment of patient's medication needs and health status, (ii) identification and prioritisation of medication-related problems, (iii) selection of intervention(s) and formulation of pharmaceutical care plan, (iv) patient agreement, implementation and monitoring, and (v) follow-up. Proposed activities results in pharmaceutical care benefits described in the literature, involving revealing of patients’ medication needs and drug related problems, optimising medication use and improve patients’ quality of life.
2 Person Centred Care Model in Pharmaceutical Care
Some pharmacy personnel have begun to integrate person-centred care to enhance pharmaceutical care delivery. Key aspects of person-centred care within pharmaceutical care “include listening to the individual to understand their perspective, providing information in a manner which enables the person to make informed decisions and supporting them to develop goals relating to their lifestyle, health and medicines”.
Barnet [3] described a model of person-centered care development and implementation within pharmacy practice in Great Britain. As a foundation for implementation of such model, two prerequisites were addressed: (i) the concept of self-care and self-management was introduced via regulations set out by the National Health System Plan in 2000, and (ii) the acceptance of the concept by leading authorities, such as the World Health Organisation [59]. The Royal Pharmaceutical Society (RPS) of Great Britain played an essential role in the implementation of person-centered care in the pharmaceutical sector. The RPS accepted and supported the concept within the publication “Now or never: shaping pharmacy for the future” [53], highlighting how pharmacists can help and maintain self-management. The RPS also issued the guideline “Medicines Optimisation: helping patients to make the most of medicines” where patient experience is listed as the first of four key principles of medicines optimisation [42]. Two years later, the RPS suggested measures to implement person-centered care delivery through pharmacies, primarily to patients with long-term conditions [3]. The concept was also incorporated in the publication “Standards for pharmacy professionals”, defined by the General Pharmaceutical Council [14]. Further efforts were made by The Centre for Postgraduate Pharmacy Education to provide continuing professional education to support the transition to the active participation of people in their own care, shared decision-making between healthcare professionals and users of healthcare services and the introduction of health coaching to support medicines optimisation and improve adherence [3].
The capability of pharmacists to deliver person-centered care as a concept which integrates the person’s needs, values and preferences is well-established within the main elements of pharmaceutical care. It is predominantly reflected through taking the responsibility for optimising medication use in order to improve health outcomes and quality of life. Accordingly, many pharmaceutical care services were suggested as convenient for delivery of person-centered care, such as medication reviews and helping people with discharge medicines when leave hospital, broader support for physical and mental wellbeing and inhaler technique support, etc.
However, several challenges in delivery of person-centered pharmaceutical care have been recognized. People are not familiar with pharmaceutical care services and support which can be accessed in community pharmacies. To address this, efforts should be made to raise the awareness of pharmacists and the services they offer. Collaboration with the voluntary and community sectors has been seen as the model for raising the awareness among people with long-term conditions about the support that pharmacists can offer. Non-governmental organisations, such as different associations of patient groups, can play an important role. Pharmacists need to be recognized as members of multidisciplinary teams, and collaboration with general practitioners must be improved (RPS 2017).
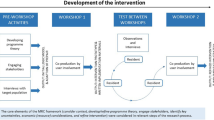
In summary, the contributions and the support of regulatory authorities and professional associations, community, other healthcare professionals and educational organisations are essential in the development, implementation and sustainability of person-centred pharmacy services. These elements represent pillars of person-centred pharmaceutical care, which are presented in the model illustrated in the Fig. 4.1.
There are promising indicators regarding the implementation of person-centred principles in pharmacy practice. Twigg and colleagues report on the Pharmacy Care Plan Service, introduced in Great Britain as a new community pharmacy intervention. It includes use of the Patient Activation Measure, a new tool for health professionals aimed to tailoring advice to individual needs of person. As part of the service, patients and pharmacists identify and agree on patient health goals. Patients have regular consultations with a pharmacist, who coaches and motivates the patients to enhance their quality of life through improved management of symptoms, lifestyle choices, weight loss and resulting improvement in health conditions. In conclusion, this example of implementation of person-centred pharmacy care in practice demonstrates that pharmacists can successfully recruit a large number of patients who are appropriate for such a service. Patients are willing to identify goals with the pharmacist. Future research will examine the impact of this service on health outcomes, but it is reasonable to argue that benefits will result from this service. If the majority of patient goals are met, they are likely to lead to improvements in quality of life for patients and their families.
3 Pharmacists as Collaborators in Multi-disciplinary Health Services Delivery Teams
The period between 2010 and 2020 will be remembered as a period of transformation of health care systems in their orientation to people-centered care (PCC) [63]. Providing services tailored to the identified people’s needs has become a challenge for all healthcare professionals and health care systems. The integrated health care is a complex approach and requires consideration of persons’ and population health needs, implementation of services related to identified needs, and transformation of health systems in order to provide customized services and strategic change management [61].
Integrated health services are defined, according to the WHO [61], as “an approach to strengthen people-centred health systems through the promotion of the comprehensive delivery of quality services across the life-course, designed according to the multi-dimensional needs of the population and the individual and delivered by a coordinated multi-disciplinary team of providers working across settings and levels of care”. Integrated health services should be managed in the most cost-effective manner and should deliver optimal health outcomes [61]. According to Fulop’s typology of integrated care, such “integration” might be established on four levels where the “service” integration level requires multi-disciplinary inter-sectoral and multi-sectoral teams of professionals to provide appropriate clinical services [28, 61]. Most definitions of pharmaceutical care focus on the improvement of patient health outcomes. Yet, the providers of pharmaceutical care vary from “anyone”, to “pharmacists with their team”, to “pharmacists only” to “practitioners”, depending on the definition [1]. Ultimately, enhanced pharmacist-physician collaboration will allow both groups of professionals to provide effective pharmaceutical care that results in optimal health outcomes for the patient.
According to McDonough and Doucette [30], the collaboration between pharmacists and general practitioners can be described in five progressive stages: (1) “professional awareness”, (2) “professional recognition”, (3) “exploration and trial”, (4) “expansion of professional relationships” and (5) “commitment to the collaborative working relations”. The first stage represents the lowest degree of interaction, while, in the second stage, the collaboration is initiated from one party (mostly pharmacists) without any recognition of collaboration benefits by physicians. In the last stage, Stage 5, the pharmacist-physician collaboration is strong and there are mutual benefits for both parties with a high degree of trust and respect established. The model identifies other factors that can affect the pharmacist-physician collaboration, including individual personal characteristics, context characteristics (e.g., practices and settings), and social interaction (exchange) characteristics of collaborators [30].
Bradley and colleagues [7] propose an extended conceptual model that describes the levels of collaboration between pharmacists and general practitioners using a matrix. One side of the matrix indicates the elements deemed important for the collaboration, which include locality, service provision, trust, “knowing” each other, communication, professional roles and professional respect. The other side of the matrix describes the levels of collaboration for each element: isolation, communication and collaboration [7]. Rathbone and colleagues [45] examined collaboration between pharmacists and general practitioners with the specific aim to support patient medication adherence. They found various factors that influenced successful collaboration: proactive communication, direct communication (including electronic communication in situations where face-to-face communication is not possible), regular interactions, location, perceptions of credibility and common vision [45].
Some studies investigated physician and pharmacist perceptions about barriers to collaboration to achieve the best patient health outcomes. In one study, general practitioners identified the two most important activities of pharmacists as dispensing medicines and helping patients to achieve improved medication adherence. The two most important barriers for pharmacist-physician collaboration were a perceived lack of need to collaborate with a variety of health care professionals and a lack of compensation for collaboration [23]. Another study found that the image of a pharmacist as a “shopkeeper” influences general practitioners’ opinions about extending pharmacy services or prescribing rights. Pharmacists viewed general practitioners’ secretaries as barriers to establishing collaboration. The “lack of awareness” between pharmacists and general practitioners was stressed as another barrier. General practitioners expressed that they did not know what skills and training pharmacists have, and pharmacists felt that general practitioners underestimated them and their contributions to patients’ health care [19].
The Kaiser Permanente (USA) population-based model is primarily based on multi-disciplinary medical practice where pharmacists are active members of professional health care teams [17]. The Kaiser Permanente model is oriented towards optimal patient care via multi-disciplinary practice. As such, this model does not include a strict division of services that should be provided at the primary, secondary or tertiary levels. Provision of services from mixed health care levels led to proven cost-effective services. The model is based on population and case management. The population management aspect is focused on services provided to patients depending on the complexity of their health condition and risk factors. Therefore, the population management aspect includes services within health promotion and disease prevention, self-management support and disease management. These services apply to the majority of the population. The case management aspect includes services provided to a sub-set of the population. This is the smallest part of all patients and includes services for treatment of severe complications [62]. Applying these principles resulted in fewer hospitalized patients comparing to United Kingdom National Health System. The role of pharmacists in such a model is of great importance, as they can make important contributions in both population and case management levels [12, 29, 63].
The collaborative practice of pharmacists and medical practitioners is widely recognized in the care of patients with chronic conditions such as diabetes, hypertension, asthma, and chronic obstructive pulmonary disease. Successful collaboration may lead to better care of patients, improved disease management and, ultimately, lower health care costs [20, 31, 39, 50]. Nowadays, in many countries, medications can be prescribed via electronic prescriptions and can be dispensed repeatedly for a period of several months without need for a visit with a general practitioner. In these cases, the role of the pharmacist is crucial in monitoring of health outcomes, medication optimization, managing drug-related problems and patient education [6].
In recent years organizations such as the World Health Organization (WHO) and the Organisation for Economic Co-operation and Development (OECD) recognized community pharmacists as health care professionals who can provide direct health care services of high quality to patients by themselves or in collaboration with other health care professionals [54, 65]. Although the primary role of community pharmacists is supply of medicines, which is very important for access to and safety of medicines, there are many other services that pharmacists can provide. In fact, the Pharmaceutical Group of the European Union (PGEU) has identified 38 different pharmacy services in PGEU member countries. In line with the Kaiser Permanente model principles, all services were stratified as dispensing and related services, services in health promotion and disease prevention, screening and referral services, and disease and individual case management services [21]. The effectiveness of many of these services could be enhanced if they were implemented in collaboration with other health care professionals.
The pandemic of coronavirus disease revealed that European health systems are also facing a shortage of health care professionals [34]. This trend is expected to increase [60, 62]. At the same time, the number of chronic patients is increasing every year [55]. Pharmacists possess specific knowledge on medicines and patient care, and they develop competencies throughout their careers to be able to provide effective and efficient pharmaceutical care. Since pharmaceutical and medicine are related sciences, there is a partial overlap in a number of relevant services delivered to patients with chronic diseases. In conclusion, it is of paramount importance that pharmacists begin to be recognized as health professionals who can provide more services and work in teams with other health care professionals. Within the PGEU vison for community pharmacy in Europe, patient-centred care and person-centred care provided in multi-disciplinary collaborative care teams of pharmacists and other health care professionals on different levels and in different health care settings are recognized as a challenge and an opportunity to foster quality of care and patient safety (Pharmaceutical Group of European Union).
4 Patients as Collaborators in Their Own Care: The Role of Health Literacy and Pharmacotherapy Literacy
How person-centred care (PCC) is defined, applied and measured differs within and across countries. There is general agreement that PCC refers to ‘care that is centred on the person’ or care of the ‘whole person’ [10, 24, 33]. A substantial international body of work describes person-centred healthcare as a multi-dimensional concept that delivers care responsive to people’s individual abilities, preferences, lifestyles and goals [33, 35, 49]. According to The Health Foundation (2014) person-centred care could mean, at the very least, four different things: (i) affording people dignity, respect and compassion, (ii) offering coordinated care, support or treatment, (iii) offering personalised care, support or treatment and (iv) being enabling [11]. Achieving person-centred healthcare requires a system that supports people in making informed decisions about and successfully managing their own health and care, including therapy choices and choosing when to let others act on their behalf. The patient experience of receiving care within the spectrum of healthcare is core to the concept of person-centred care.
In order for patients to play an important role in their own health care, as advocated in person-centred care, health literacy is a key factor influencing this capacity. Health literacy has been recognized as an important component of health care, and the World Health Organisation describes health literacy as “the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health” [26]. Health literacy is a multi-dimensional concept composed of a variety of cognitive, affective, social, and personal skills and attributes. Buchbinder and colleagues [8] identified seven key abilities required for an individual to be able to seek, understand, and use health information: (1) knowing when to seek health information,(2) knowing where to seek health information,(3) verbal communication skills; (4) assertiveness; (5) literacy skills; (6) capacity to process and retain information; and (7) skills in applying health-related information.
Information about the health literacy of people in a community can offer better insight into the challenges people experience when trying to access and engage with healthcare services. Low literate patients may also provide poor self-assessment of their health, wellbeing or engagement with their care. Individuals with limited health literacy experience difficulties in understanding medicines labels, which may include misunderstanding of written medicine instructions, inadequate adherence to prescribed regimens, and inability to follow advice from health professionals regarding side effects and possible contraindications [25, 57]. Studies suggest that differences in health literacy abilities may explain observed health inequalities among people of different race and with different levels of educational levels [5, 37, 52, 58, 64]. Therefore, developing interventions to address low health literacy offers an opportunity to improve person-centred healthcare, health outcomes and reduce health inequalities. There are many measures to assess health literacy at the individual (clinical) and population level. The most widely used clinical measures include the Rapid Estimate of Adult Literacy in Medicine (REALM), which tests ability to read and pronounce a list of words, and the Test of Functional Health Literacy in Adults (TOFHLA), which tests reading comprehension and numeracy, whereas the Newest Vital Sign (NVS) is designed to be a quick clinical screening instrument.
One of the most comprehensive measures of health literacy at the population level relevant to person-centered healthcare is the Health Literacy Questionnaire (HLQ) developed by Deakin University and Monash University in Australia [4, 16]. It consists of 44 questions within nine domains: 1. Feeling understood and supported by healthcare providers 2. Having sufficient information to manage my health 3. Actively managing my health 4. Social support for health 5. Appraisal of health information 6. Ability to actively engage with healthcare providers 7. Navigating the healthcare system 8. Ability to find good health information 9. Understanding health information well enough to know what to do. Osborne and colleagues [41] found it acceptable to patients and healthcare workers, but it has been designed and tested for use at the population level, not for use with individual patients. It was designed for self-administration using pen and paper and can also be interviewer-administered. Data derived from HLQ included both subjective (e.g. ‘did you feel respected?’) and objective (e.g. ‘were you offered a care plan?’) items, as well as general (e.g. ‘how satisfied were you with your care?’) and specific (e.g. ‘how satisfied were you with family visiting arrangements?’) items [41].
Medication or pharmacotherapy literacy is a sub-area of health literacy. It is particularly important to patient safety in the context of person-centred care. Many studies have stressed that inadequate levels of medication literacy may negatively affect pharmacotherapy outcomes and safety of care delivery, particularly in areas of greater social deprivation and where significant health inequalities exist. Any analysis of pharmacotherapy literacy must navigate a quite heterogeneous body of literature and commentary and innovative practice. “Medication literacy” was generally defined as the individual’s ability to understand and act on medication-related information. Pouliot and colleagues [44] defined it as “the degree to individuals can obtain, comprehend, communicate, calculate and process patient specific information about their medications, and make informed medication and health decisions in order to safely and effectively use their medications- regardless of the mode by which the content is delivered “ [44]. The overlap with person-centred care is highlighted in this definition of pharmacotherapy literacy as “an individual’s capacity to obtain, evaluate, calculate, and comprehend basic information about pharmacotherapy and pharmacy related services necessary to make appropriate medication-related decisions, regardless of the mode of content delivery (e.g., written, oral, visual images and symbols)” [25, 57]. Although medication literacy is a relatively recent concept, several tools have already been developed to assess it [57]. In conclusion, the linkage between pharmacotherapy literacy and person-centred care approaches is currently relatively under-developed and may be an important area for development in the future [25, 43, 44, 46, 57].
5 E-Pharmaceutical Service and Implications for Person-Centred Care
Many health systems in Europe are characterized by a shortage of health workers, overwork and high costs, all of which lead to unsustainability in the long run [38]. Population aging is a long-term trend that began in Europe several decades ago. The age structure of the population has been reshaped, so there is an increasing percentage of the elderly and consequently a decreasing percentage of working people in the total population [13]. On the other hand, beneficiaries of health care services are insufficiently informed or uninformed, they usually wait too long for specialist examinations, interventions and have the feeling that doctors do not pay enough attention to them. This current status couldn’t achieve Person-centred care framework.
Might telemedicine/telepharmacy be one solution to address some of these issues identified by health system professionals and users?
Historically, the beginnings of telemedicine can be traced back to the nineteenth century and the invention of the electric telegraph and telephone, which allowed doctors and patients to communicate remotely [22]. For the first time, in 1959, the University of Nebraska used two-way (interactive) television to transmit neurological examinations to students [51]. The American Telemedicine Association (ATA) was founded in 1993 with the aim of promoting access to telemedicine care through telecommunications technology [27]. In the early twenty-first century a wider use of the Internet made the development of telemedicine and telepharmacy possible, together with advancements in their regulations and standards. Despite the legal basis in European Union regulations, where telemedicine falls under health and information services, international and national legal frameworks for the use of telemedicine are lacking. To overcome these challenges, telemedicine must be regulated by comprehensive legal guidelines which must be placed within a single international legal framework [47].
Operatively, telemedicine covers two broad areas. The first is the virtual interaction between the patient and the health care provider, and the second is the flow of information [36].
Telepharmacy, which is a part of telemedicine, may help improve pharmacy service coverage regardless of the pharmacist's location. Telepharmacy considers activities such as: electronic data entry, prescription order verification, centrally, online benefit adjudication, medication dispensing, and telehealth consultation with medication use evaluation using computer technology [48].
One of the first studies demonstrating the person-centered nature of pharmaceutical care, delivered via a telepharmacy service model, was introduced by Sankaranarayanan and colleagues [48].
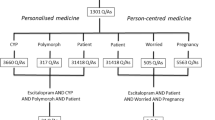
Regarding this telepharmacy service model, three definitions at the intervention level have been introduced: the patient-centered medication management level, the health system-centered medication use process level and the remote pharmacist role across hospitals with and without an on-site hospital pharmacist.
An interprofessional and collaborative practice between physician and pharmacist is one of the perquisites of person-centered care [9]. Using telemedicine/ telepharmacy, communication is facilitated and incredibly useful for improving patients' health. The inclusion of telepharmacy may expand the reach of the pharmacist's intervention and provide pharmacy operations and patient care at a distance with further benefits for patients and their managing physicians [40].
An e-pharmaceutical intervention improved health outcome in many clinical areas: anticoagulant therapy monitoring, oncology, diabetes, hypertension [15]. E- pharmaceutical interventions was an efficient, safe, and cost-effective method for implementing person-centered approach.
The global Covid-19 virus pandemic demonstrated the urgent need for implementation of telemedicine services. In the Republic of Slovenia, for example, new providers of telemedicine services grew each day of the pandemic, while the Public Institute Pharmacy Ljubljana has only recently introduced telepharmacy services [32].
Recent research on the attitudes of Slovenian pharmacists indicate that telepharmacy services should be charged for (Mandic 2020, unpublished data). In other words, they suggested a model of financing separate from compulsory health insurance in to ensure the financial sustainability of the new service and allow it to always be available to patients. Although there are important challenges with regards to the systemic, legal regulation of this area and the protection of personal data, as discussed earlier in the section, the study participants endorsed the need to introduce new services into the pharmacy system and, in general, a very positive attitude towards the introduction of telepharmaceutical services. Their motivation for learning and acquiring new skills was clear, and readiness for change is an important precondition for the implementation of new services. They see telepharmacy as a potential for progress and further development and contribution to the health system in the Republic of Slovenia, as well.
This study of Slovenian pharmacists also provided positive results regarding digital literacy. Pharmacists indicated that they actively use digital communication channels and were confident in their levels of digital literacy. If educating elderly patients were possible or telepharmaceutical services were set up so that they are extremely easy to use, the pharmacists who participated in the survey did not see any major obstacles in providing new services based on digital communication channels. They expressed a clear interest in using digital technologies for the purpose of providing a service that would be more accessible to patients, but also to enable greater and easier interaction to pharmacists, allowing greater supervision and control over the health of their patients. Personal contact is certainly best for conversation, counseling and understanding the needs of patients. However, if personal contact is hindered for some reason, the pharmacists believed that they could make up for this by offering a slightly higher degree of empathy because the patients were already comfortably at home. Telepharmaceutical services should not additionally burden pharmacists nor require too much administration, and certainly those services should be financially valued in some way (Mandic 2020, unpublished data).
In order to fully develop and implement telepharmacy services with a health system, in context of person-centered care, certain resources are required. For instance, adequate standards, education and training of pharmacists are needed [2].
Telepharmacy, i.e. e-pharmacy, can take place through special platforms (applications or sites), but this is not a necessary prerequisite. Implementation can start at a simpler level, using already available resources, such as ordinary telephone conversations or calls via free online communication channels (Skype, Viber, Whatsapp, Zoom, Webex, etc.).
Any new service, including telepharmacy, should be simple, safe, financially viable and, above all, assist both patients and pharmacists in achieving their joint goal: person in the center of the healthcare system.
6 Conclusion
This chapter examined person-centred care within pharmaceutical care delivery in detail. The importance of the pharmacist as part of a multi-disciplinary care team and the need for close collaboration with general practitioners, including barriers to such collaboration, was examined. Then the role of the patient in person-centred pharmaceutical care, with an emphasis on health literacy, and medication literacy in particular, was explored. The chapter concluded with an overview of telemedicine and e-pharmacy or telepharmacy services, with implications for person-centred care.
References
Allemann, S.S., van Mil, J.W., Botermann, L., Berger, K., Griese, N., Hersberger, K.E.: Pharmaceutical care: the PCNE definition 2013. Int. J. Clin. Pharm. 36(3), 544–555 (2014). https://doi.org/10.1007/s11096-014-9933-x
Baldoni, S., Amenta, F., Ricci, G.: Telepharmacy services: present status and future perspectives: a review. Medicina (Kaunas) 55(7), 327 (2019). https://doi.org/10.3390/medicina55070327
Barnet N.: Person-centred over patient-centred care: not just semantics. How does the technology giant’s marketing approach relate to person-centred care in health? Pharm. J. (2018)
Batterham, R.W., Buchbinder, R., Beauchamp, A., Dodson, S., Elsworth, G.R., Osborne, R.H.: The OPtimising HEalth LIterAcy (Ophelia) process: study protocol for using health literacy profiling and community engagement to create and implement health reform. BMC Public Health 14, 694 (2014). https://doi.org/10.1186/1471-2458-14-694
Berkman, N.D., Sheridan, S.L., Donahue, K.E., Halpern, D.J., Crotty, K.: Low health literacy and health outcomes: an updated systematic review. Ann. Intern. Med. 155(2), 97–107 (2011). https://doi.org/10.7326/0003-4819-155-2-201107190-00005
Bond, C., Matheson, C., Williams, S., Williams, P., Donnan, P.: Repeat prescribing: a role for community pharmacists in controlling and monitoring repeat prescriptions. Br. J. Gen. Pract. 50(453), 271–275 (2000)
Bradley, F., Ashcroft, D.M., Noyce, P.R.: Integration and differentiation: a conceptual model of general practitioner and community pharmacist collaboration. Res. Soc. Adm. Pharm. 8(1), 36–46 (2012). https://doi.org/10.1016/j.sapharm.2010.12.005
Buchbinder, R., Batterham, R., Ciciriello, S., Newman, S., Horgan, B., Ueffing, E., Rader, T., Tugwell, P.S., Osborne, R.H.: Health literacy: what is it and why is it important to measure? J. Rheumatol. 38(8), 1791–1797 (2011). https://doi.org/10.3899/jrheum.110406
Bugnon, O., Hugentobler-Hampaï, D., Berger, J., Schneider, M.P.: New roles for community pharmacists in modern health care systems: a challenge for pharmacy education and research. CHIMIA (Aarau) 66(5), 304–307 (2012). https://doi.org/10.2533/chimia.2012.304
Care Quality Commission: The State of Healthcare and Adult Social Care in England - An Overview of Key Themes in Care 2009/10. Care Quality Commission, London (2010)
Collins, A.: Measuring What Really Matters. The Health Foundation, London (2014)
Curry, N., Ham, C.: Clinical and service integration. The route to improved outcomes (2010)
Eurostat Statistics Explained. Available at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing/sl#Pretekli_in_prihodnji_trendi_staranja_prebivalstva_v_EU. Accessed 20 Dec 2020
General Pharmaceutical Council: Standards for pharmacy professionals (2017). Available at: https://www.pharmacyregulation.org/sites/default/files/standards_for_pharmacy_professionals_may_2017_0.pdf. Accessed 20 Dec 2020
Hawes, E.M., Lambert, E., Reid, A., Tong, G., Gwynne, M.: Implementation and evaluation of a pharmacist-led electronic visit program for diabetes and anticoagulation care in a patient-centered medical home. Am. J. Health Syst. Pharm. 75(12), 901–910 (2018). https://doi.org/10.2146/ajhp170174
Hawkins, M., Gill, S.D., Batterham, R., Elsworth, G.R., Osborne, R.H.: The health literacy questionnaire (HLQ) at the patient-clinician interface: a qualitative study of what patients and clinicians mean by their HLQ scores. BMC Health Serv. Res. 17(1), 309 (2017). https://doi.org/10.1186/s12913-017-2254-8
Helling, D.K., Nelson, K.M., Ramirez, J.E., Humphries, T.L.: Kaiser Permanente Colorado region pharmacy department: innovative leader in pharmacy practice (2003). J. Am. Pharm. Assoc. 46(1), 67–76 (2006). https://doi.org/10.1331/154434506775268580
Hepler, C.D., Strand, L.M.: Opportunities and responsibilities in pharmaceutical care. Am. J. Hosp. Pharm. 47(3), 533–543 (1990)
Hughes, C.M., McCann, S.: Perceived interprofessional barriers between community pharmacists and general practitioners: a qualitative assessment. Br. J. Gen. Pract. 53(493), 600–606 (2003)
Hwang, A.Y., Gums, T.H., Gums, J.G.: The benefits of physician-pharmacist collaboration. J. Fam. Pract. 66(12), E1–E8 (2017)
Institute for Evidence Based Health: Pharmacy services in Europe: evaluating trends and value report. Lisboa (2020)
Institute of Medicine (US): Committee on evaluating clinical applications of telemedicine. In: Field, M.J. (eds.) Telemedicine: A Guide to Assessing Telecommunications in Health Care. National Academies Press (US), Washington (DC) (1996). Available at: https://www.ncbi.nlm.nih.gov/books/NBK45445. Accessed 20 Dec 2020
Kelly, D.V., Bishop, L., Young, S., Hawboldt, J., Phillips, L., Keough, T.M.: Pharmacist and physician views on collaborative practice: findings from the community pharmaceutical care project. Can. Pharm. J. (Ott) 146(4), 218–226 (2013). https://doi.org/10.1177/1715163513492642
Kidd M.: Personal correspondence. World Organisation of Family Doctors (WONCA) and Flinders University, Australia, July 2015
King, S.R., McCaffrey, D.J., Bouldin, A.S.: Health literacy in the pharmacy setting: defining pharmacotherapy literacy. Pharm. Pract. 9(4), 213–220 (2011). https://doi.org/10.4321/s1886-36552011000400006
Krajnović, D., Ubavić, S., Bogavac-Stanojevic, N.: Pharmacotherapy literacy and parental practice in use of over-the-counter pediatric medicines. Medicina (Kaunas) 55(3), 80 (2019). https://doi.org/10.3390/medicina55030080
Krupinski, E.A., Antoniotti, N., Bernard, J.: Utilization of the American telemedicine association’s clinical practice guidelines. Telemed. E-Health 19(11), 846–851 (2013). https://doi.org/10.1089/tmj.2013.0027
Lewis, R., Rosen, R., Goodwin, N., Dixon, J.: Where next for integrated care organizations in the English NHS? The Nuffield Trust, London (2010)
Light, D., Dixon, M.: Making the NHS more like Kaiser Permanente. BMJ 328(7442), 763–765 (2004). https://doi.org/10.1136/bmj.328.7442.763
McDonough, R., Doucette, W.: Developing collaborative working relationships between pharmacists and physicians. J. Am. Pharm. Assoc. 41(5), 682–692 (2001)
Mes, M.A., Katzer, C.B., Chan, A.H.Y., Wileman, V., Taylor, S.J.C., Horne, R.: Pharmacists and medication adherence in asthma: a systematic review and meta-analysis. Eur. Respir. J. 52(2), 1800485 (2018). https://doi.org/10.1183/13993003.00485-2018
Mestna občina Ljubljana <Ali ste vedeli:Lekarna Ljubljana prva v Sloveniji uvaja telefarmacevtsko svetovanje>. Available at: www.ljubljana.si/sl/moja-ljubljana/ali-ste-vedeli/ali-ste-vedeli-lekarna-ljubljana-prva-v-sloveniji-uvaja-telefarmacevtsko-svetovanje/. Accessed Oct 2020
Mezzich, J.E., Appleyard, J., Botbol, M., Ghebrehiwet, T., Groves, J., Salloum, I., van Dulmen, S.: Ethics in person centered medicine: conceptual place and ongoing developments. J. Pers.-Cent. Med. 3(4), 255–257 (2013)
Michel, J.P., Ecarnot, F.: The shortage of skilled workers in Europe: its impact on geriatric medicine. Eur. Geriatr. Med. 11(3), 345–347 (2020). https://doi.org/10.1007/s41999-020-00323-0
Miles, A., Asbridge, J.E.: Clarifying the concepts, epistemology and lexicon of person-centeredness: an essential pre-requisite for the effective operationalization of PCH within modern healthcare systems. Eur. J. Pers. Cent. Healthc. 2(1), 1–15 (2014). https://doi.org/10.5750/ejpch.v2i1.857
Nittari, G., Khuman, R., Baldoni, S., Pallotta, G., Battineni, G., Sirignano, A., Amenta, F., Ricci, G.: Telemedicine practice: review of the current ethical and legal challenges. Telemed. E-Health 26(12), 1427–1427 (2020). https://doi.org/10.1089/tmj.2019.0158
Nutbeam, D.: The evolving concept of health literacy. Soc. Sci. Med. 67(12), 2072–2078 (2008). https://doi.org/10.1016/j.socscimed.2008.09.050
OECD: Health workforce (2020). Available at: www.oecd.org/els/health-systems/workforce.htm. Accessed 20 Dec 2020
Omboni, S., Caserini, M.: Effectiveness of pharmacist's intervention in the management of cardiovascular diseases. Open Hear. 5(1), e000687 (2018). https://doi.org/10.1136/openhrt-2017-000687
Omboni, S., Tenti, M., Coronetti, C.: Physician-pharmacist collaborative practice and telehealth may transform hypertension management. J. Hum. Hypertens. 33(3), 177–187 (2019). https://doi.org/10.1038/s41371-018-0147-x
Osborne, R.H., Batterham, R.W., Elsworth, G.R., Hawkins, M., Buchbinder, R.: The grounded psychometric development and initial validation of the health literacy questionnaire (HLQ). BMC Public Health 13, 658 (2013). https://doi.org/10.1186/1471-2458-13-658
Picton, C., Wright, H.: Medicines optimisation: helping patients to make the most of medicines. Royal Pharmaceutical Society (2013). Available at: www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy/helping-patients-make-the-most-of-their-medicines.pdf. Accessed 20 Dec 2020
Pouliot, A., Vaillancourt, R.: Medication literacy: why pharmacists should pay attention. Can. J. Hosp. Pharm. 69(4), 335–336 (2016). https://doi.org/10.4212/cjhp.v69i4.1576
Pouliot, A., Vaillancourt, R., Stacey, D., Suter, P.: Defining and identifying concepts of medication literacy: an international perspective. Res. Soc. Adm. Pharm. 14(9), 797–804 (2018). https://doi.org/10.1016/j.sapharm.2017.11.005
Rathbone, A.P., Mansoor, S.M., Krass, I., Hamrosi, K., Aslani, P.: Qualitative study to conceptualise a model of interprofessional collaboration between pharmacists and general practitioners to support patients’ adherence to medication. BMJ Open 6(3), e010488 (2016). https://doi.org/10.1136/bmjopen-2015-010488
Raynor, D.K.: Addressing medication literacy: a pharmacy practice priority. Int. J. Pharm. Pract. 17(5), 257–259 (2009)
Ryu, S.: Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth 2009 (Global Observatory for eHealth, Volume 2). Healthc. Inform. Res. 18(2), 153–155 (2012). https://doi.org/10.4258/hir.2012.18.2.153
Sankaranarayanan, J., Murante, L., Moffett, L.: A retrospective evaluation of remote pharmacist interventions in a telepharmacy service model using a conceptual framework. Telemed. E-Health 20(10), 893–901 (2014). https://doi.org/10.1089/tmj.2013.0362
Scholl, I., Zill, J.M., Härter, M., Dirmaier, J.: An integrative model of patient-centeredness– a systematic review and concept analysis. PLoS One 9(9), e107828 (2014). https://doi.org/10.1371/journal.pone.0107828
Siaw, M.Y.L., Ko, Y., Malone, D.C., Tsou, K.Y.K., Lew, Y.J., Foo, D., Tan, E., Chan, S.C., Chia, A., Sinaram, S.S., Goh, K.C., Lee, J.Y.: Impact of pharmacist-involved collaborative care on the clinical, humanistic and cost outcomes of high-risk patients with type 2 diabetes (IMPACT): a randomized controlled trial. J. Clin. Pharm. Ther. 42(4), 475–482 (2017). https://doi.org/10.1111/jcpt.12536
Simson, A.: A brief history of NASA’s contributions to telemedicine (2013). Available at: www.nasa.gov/content/a-brief-history-of-nasa-s-contributions-to-telemedicine. Accessed 20 Dec 2020
Sørensen, K., Pelika, J.M., Röthlin, F., Ganahl, K., Slonska, Z., Doyle, G., Fullam, J., Kondilis, B., Agrafiotis, D., Uiters, E., Falcon, M., Mensing, M., Tchamov, K., van den Broucke, S., Brand, H., HLS-EU Consortium: Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 25(6), 1053–1058 (2015). https://doi.org/10.1093/eurpub/ckv043
Smith, J., Picton, C., Dayan, M.: Now or never: shaping pharmacy for the future. Royal Pharmaceutical Society (2013). Available at: www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Publications/Now%20or%20Never%20-%20Report.pdf. Accessed 20 Dec 2020
The Organisation for Economic Co-operation and Development: Health at a Glance 2019, OECD Indicators. Pharmacists and Pharmacies (2019)
The Organisation for Economic Co-operation and Development: Health at a Glance 2019: OECD Indicators (2019)
The Royal Pharmaceutical Society: The role of pharmacy in delivering person-centred care. Available at: www.rpharms.com/resources/reports/role-of-pharmacy-in-delivering-person-centred-care. Accessed 20 Dec 2020
Ubavić, S., Bogavac-Stanojević, N., Jović-Vraneš, A., Krajnović, D.: Understanding of information about medicines use among parents of pre-school children in Serbia: parental pharmacotherapy literacy questionnaire (PTHL-SR). Int. J. Environ. Res. Public Health 15(5), 977 (2018). https://doi.org/10.3390/ijerph15050977
United Nations Economic and Social Council (ECOSOC): Health literacy and the millennium development goals. United Nations Economic and Social Council (ECOSOC) regional meeting background paper (abstracted). J. Health Commun. 15(Suppl 2), 211–223 (2010). https://doi.org/10.1080/10810730.2010.499996
World Health Organization: People-centred health care: a policy framework (2007). Available at: www.wpro.who.int/health_services/people_at_the_centre_of_care/documents/ENG-PCIPolicyFramework.pdf. Accessed 12 Dec 2020
World Health Organization: A universal truth: no health without a workforce (2014). Available at https://www.who.int/workforcealliance/knowledge/resources/hrhreport2013/en/. Accessed 12 Dec 2020
World Health Organization: The European framework for action on integrated health services delivery: an overview (2016). Available at https://www.euro.who.int/en/health-topics/Health-systems/health-services-delivery/publications/2016/the-european-framework-for-action-on-integrated-health-services-delivery-an-overview-2016. Accessed 12 Dec 2020
World Health Organization: Global strategy on human resources for health: workforce 2030 (2016). Available at https://www.who.int/hrh/resources/globstrathrh-2030/en/. Accessed 12 Dec 2020
World Health Organization: Integrated care models: an overview (2016). Available at https://www.euro.who.int/en/health-topics/Health-systems/health-services-delivery/publications/2016/integrated-care-models-an-overview-2016. Accessed 20 Dec 2020
World Health Organization: Shanghai declaration on promoting health in the 2030 agenda for sustainable development. Health Promot. Int. 32(1), 7–8 (2017). https://doi.org/10.1093/heapro/daw10
World Health Organization: The legal and regulatory framework for community pharmacies in the WHO European region (2019). Available at https://apps.who.int/iris/handle/10665/326394. Accessed 20 Dec 2020
Acknowledgements
This publication is based upon work from COST Action “European Net-work for cost containment and improved quality of health care-CostCares” (CA15222), supported by COST (European Cooperation in Science and Technology)
COST (European Cooperation in Science and Technology) is a funding agency for research and innovation networks. Our Actions help connect research initiatives across Europe and enable scientists to grow their ideas by sharing them with their peers. This boosts their research, career and innovation.

Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Marinkovic, V., Odalovic, M., Tadic, I., Krajnovic, D., Mandic, I., Rogers, H.L. (2022). Person-Centred Care Interventions in Pharmaceutical Care. In: Kriksciuniene, D., Sakalauskas, V. (eds) Intelligent Systems for Sustainable Person-Centered Healthcare. Intelligent Systems Reference Library, vol 205. Springer, Cham. https://doi.org/10.1007/978-3-030-79353-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-79353-1_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-79352-4
Online ISBN: 978-3-030-79353-1
eBook Packages: Intelligent Technologies and RoboticsIntelligent Technologies and Robotics (R0)